Introduction
Acute cholecystitis is an inflammatory disease of the gallbladder. Ultrasonography (US) is the initial and the most valuable method in the diagnosis of acute cholecystitis. Also, laboratory findings are used to support the diagnosis. The aim of the present study was to evaluate the diagnostic value of mean platelet volume (MPV) and platelet (PLT) counts in patients with acute cholecystitis.
Materials and Methods
From January to August 2014, the medical records of patients were reviewed for the diagnosis of acute cholecystitis. The study included 60 age-matched patients with acute cholecystitis and 60 healthy individuals as a control group. Patients with a chronic disease were excluded from the study. Over all, patients with acute cholecystitis and patients in the control group were evaluated for their MPV, PLT count, platelet distribution width (PDW), platelet crit (PCT) and erythrocyte sedimentation rate (ESR) in a complete blood count (CBC).
Results
The MPV values were found to be significantly lower in the acute cholecystitis group when compared to the control group. The PDW and PCT were found to be significantly higher in the acute cholecystitis group when compered to the control group. When a correlation test was performed, MPV was negatively correlated with PLT and PCT counts.
Conclusion
US is the initial and the most important imaging method for diagnosing and evaluating the biliary system. Also, laboratory findings such as WBC, ESR and CRP support the diagnosis but may have some undesirable limitations. However, MPV is an acute phase reactant that does not require an additional cost because it is already worked in the CBC. Therefore, MPV can be used as a marker in diagnosing inflammatory diseases.
Introduction
Acute cholecystitis is an inflammatory disease of the gallbladder that develops in hours. In many cases, the underlying aetiology is the obstruction of the cystic duct due to an impacted stone in either the neck of the gallbladder or the cystic duct. Through early diagnosis and treatment there is a marked decrease in morbidity and mortality. Ultrasonography (US) is the initial and the most valuable method in the diagnosis of acute cholecystitis [1]. The sensitivity of US for acute calculous cholecystitis ranges from 80% to 100% and specificity ranges from 60% to 100% [2]. Additionally, laboratory findings such as white blood cell (WBC) count, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are used to support the diagnosis [1]. Nowadays, platelets are known to have a large variety of functions. Circulating platelets are prothrombotic agents that have a close association with inflammatory markers and play a key role in vascular and inflammatory diseases [3]. Platelets are activated to release inflammatory mediators following tissue injury. There are three complete blood count (CBC) parameters related to platelets: mean platelet volume (MPV), platelet crit (PCT) and platelet distribution width (PDW). MPV is the best platelet function and activation marker and, also can be easily measured by routine complete blood count tests [4,5]. MPV was previously investigated and found to have diagnostic value in detecting inflammatory disease such as celiac disease, rheumatoid arthritis, ankylosing spondylitis, ulcerative colitis and acute pancreatitis. [6-10]. However, to the best of our knowledge, there is only one study investigating MPV changes in patients with acute cholecystitis [1]. Acute cholecystitis has a high mortality rate if left untreated. Therefore, early diagnosis and treatment is very important for the survival of the patient. Like other inflammatory diseases, alterations of the MPV can be expected in acute cholecystitis. Thus, the aim of the present study was to evaluate the diagnostic value of MPV and PLT counts in patients with acute cholecystitis.
Materials and Methods
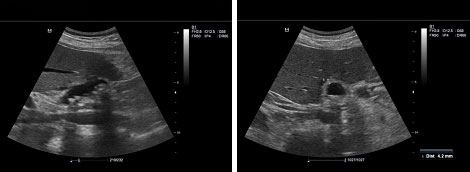
From January to August 2014, the medical records of patients were reviewed for the diagnosis of acute cholecystitis. Acute cholecystitis patients who had abdominal US and laboratory findings (WBC, CRP and ESR) on the same day were included in the study. The diagnosis of acute cholecystitis was made through a physical examination (pain in the upper right quandrant is indicative of acute cholecystitis), laboratory findings (elevated ESR and WBC are indicative of acute cholecystitis), positive CRP and positive sonographic findings [Table/Fig-1,2]. All ultrasonographic examinations (Mindray DC-7, Shenzhen, China) were performed by the same radiologist (ATS). Sixty patient were found with a diagnosis of acute cholecystitis using medical records. Also, the data of 60 age-matched, healthy individuals with a normal abdominal ultrasound were evaluated as the control group. WBC count, PLT count, PDW, PCT and MPV values in CBC results and CRP results were obtained from the patient records for the control group.
Reference range values for complete blood count data according to local calibration from our hospital’s laboratory were: platelets – 150 to 400 ×103/μL; platelet distribution width (PDW) 15 to 17; PCT – 0.1 to 0.3%; MPV 6 to 11 femtolitres (fl).
Patients with trombocytopenia and any chronic underlying diseases (including cardiovascular disorders, malignancy, hypertension, peripheral vascular diseases, metabolic disease and kidney or liver disease) were excluded from the study. Also, patients on anticoagulant or non-steroidal anti-inflammatory medication were excluded because these medications can affect platelet functions.
Statistical Analysis
The SPSS statistical software package (SPSS, version 20 for Windows; SPSS Inc., Chicago, Illinois, USA) was used to perform all statistical calculations. A Student's t-test was used for the statistical comparison of data that matched normal distribution and the Mann-Whitney U-test was used for the statistical comparison of the groups when data was not distributed normally. The Pearson Correlation testing was used to evaluate the association between MPV, ESR, PLT, PCT and PDW. The multiple linear regression analysis was used to determine the prognostical factors that may impact the MPV values. A value of p< 0.05 was considered significant in all statistical analyses. All data was expressed as mean ± SD.
Results
[Table/Fig-3] shows the following results: The acute cholecystitis group consisted of 60 patients (25 males and 35 females) with a mean age of 61.38 ± 16 years. The control group consisted of 60 healthy subjects (25 males and 35 females) with a mean age of 58.45 ± 16.4 years. There was no significant difference between the two groups regarding age and gender distribution (p = 0.325).
Mean white blood count (WBC) values were 8.63 ± 3.83 x 103/µl in patients with acute cholecystitis, vs. 7.01 ± 1.81 x 103/µl in the control group. WBC values were found to be significantly higher in the acute cholecystitis group (p = 0.004). Mean haemoglobin (HB) values were 12.31 ± 2.09 g/dl in patients with acute cholecystitis, vs. 13.18 ± 1.84 g/dl in the control group. There were significant differences in HB values between the two groups (p = 0.018).
Mean MPV values were 8.82 ± 1.45 fL in patients with acute cholecystitis, vs. 9.72 ± 0.98 fL in the control group. MPV values were found to be significantly lower in the acute cholecystitis group (p<0.05). Mean PLT counts were 265.12 ± 113.57 x 103/µl in patients with acute cholecystitis, vs. 251.33 ± 57.63 x 103/µl in the control group. There was no significant differences in the PLT counts between the two groups (p = 0.404).
PDW values were 16.62 ± 1.11 fL in patients with acute cholecystitis, vs. 16 ± 0.35 fL in the control group. PDW values were found to be significantly higher in the acute cholecystitis group (p<0.05).
PCT values were 0.27% ± 0.33% in patients with acute cholecystitis, vs. 0.23% ± 0.052% in the control group. The PCT count was found to be significantly higher in the acute cholecystitis group (p = 0.003). Mean erythrocyte sedimentation rate was 32.08 ± 27.29 in patients with acute cholecystitis. When a correlation test was performed, MPV was negatively correlated with the PLT count and PCT. Also, MPV was independent from ESR and PDW [Table/Fig-4].
Discussion
Our aim with this study was to evaluate the value of MPV and PLT counts in the diagnosis of acute cholecystitis. Acute cholecystitis is an acute inflammatory disease of the gallbladder. Signs and symptoms of cholecystitis may include severe pain in the upper right abdomen, pain that radiates from left to right in the shoulders or back, tenderness over the abdomen, nausea, vomiting and fever. Acute cholecystitis signs and symptoms often occur after a meal, particularly a large or fatty meal. Ultrasonography (US) is the initial and the most important imaging method in diagnosing and evaluating the biliary system. Also, laboratory findings such as WBC, ESR and CRP support the diagnosis [1]. Diagnostic criteria for the acute cholecystitis are local signs of inflammation, systemic signs of inflammation and imaging findings. Local signs of inflammation include Murphy’s sign as well as right upper quadrant pain and tenderness. Systemic signs of inflammation include fever, elevated CRP and high WBC count. One item in the local signs of inflammation and one item in the systemic signs of inflammation must be positive for the definitive diagnosis of acute cholecystitis. Furthermore, imaging findings confirmed the diagnosis when acute cholecystitis was clinically suspected [11]. Imaging findings characteristic of acute cholecystitis are positive sonographic Murphy's sign, thickened gallbladder wall (> 4 mm), enlarged gallbladder (long axis diameter > 8 cm, short axis diameter > 4 cm), incarcerated gallstone, debris echo, pericholecystic fluid collection, sonolucent layer in the gallbladder wall and striated intramural lucencies [11]. Laboratory findings include elevated CRP (≥ 3 mg / dL) and elevated WBC and ESR [1,11]. Although inflammatory markers (ESR and CRP) are usually elevated in inflammatory diseases, they have some disadvantages. ESR may be affected depending on the age and gender of the patient and the presence of non-inflammatory events such as anemia and renal failure. CRP concentration begins to rise 48 hours after the onset of symptoms. Furthermore, they have similar limitations to ESR [1]. Because of these limitations, researchers have begun the search for a new inflammatory marker and studies have focused on the MPV.
MPV is a machine-calculated measurement of the average size of PLTs. It also shows the activation and function of PLTs. Platelets are vital components of normal haemostasis, and they can release several inflammatory cytokines. MPV has been shown to reflect inflammatory burden and disease activity in several diseases such as preeclampsia, acute pancreatitis, unstable angina, myocardial infarction and systemic inflammation such as ulcerative colitis and Crohn’s disease [3].
Increased MPV in Crohn's disease, rheumatoid arthritis, familial Mediterranean fever, ulcerative colitis, diabetes, acute pancreatitis and acute ischemic stroke patients reported in the literature [6,7,12-14] such as active rheumatoid arthritis, ankylosing spondylitis, ulcerative colitis and familial Mediterranean fever [9,10,15]. In our study, MPV values were found to be significantly lower in the acute cholecystitis group when compared to the control group.
Among other CBC parameters that are associated with platelets are PCT and PDW. Platelets are acute-phase reactants; therefore, they increase in response to various stimuli, including systemic infections, inflammatory conditions, bleeding, and tumours. But, PLT values are still controversial in the literature. In our study, PCT, PLT and PDW values were found to be significantly higher in the acute cholecystitis group when compared to the control group, but there were no significant differences between these groups. However, Seker et al reported that PLT values were significantly lower in the acute cholecystitis group than in the control group [1]. In our study, a significant negative correlation was determined between MPV, PCT and PLT values. However, Seker et al reported a significant positive correlation between MPV and PLT [1]. Finally, no correlation was detected between the MPV and ESR values in our study.
Ultrasonography of the right upper quadrant in a 54-year-old female with severe abdominal pain in the right hypochondrium revealing a marked thickening of the gallbladder wall (4.2 mm) and the presence of gallstones
Comparison of groups regarding Age, WBC, Hb, MPV, PLT, PCT and PDW measurements
| Acute cholecystitis (n=60) | Control groups (n=60) | p-value |
|---|
| Age | 61.38±16.05 | 58.45±16.44 | 0.325 |
| WBC (x103/ul) | 8.63±3.83 | 7.01±1.81 | 0.004 |
| Hb (g/dl) | 12.31±2.09 | 13.18±1.84 | 0.018 |
| MPV (fL) | 8.82±1.45 | 9.72±0.98 | 0.00013 |
| PLT (x103/µl) | 265.12±113.57 | 251.33±57.63 | 0.00001 |
| PCT (%) | 0.27±0.33 | 0.23±0.05 | 0.003 |
| PDW (fL) | 16.62±1.11 | 16±0.35 | 0.00010 |
Abbreviations: n: number; WBC: white blood cell; Hb: haemoglobin; MPV: Mean platelet volume; PLT: Platelet; PCT: Platelet crit; PDW: Platelet distribution width
Relationship between MPV and ESR, PLT, PCT, PDW
| | ESR | PLT | PCT | PDW |
|---|
| MPV | Pearson correlation | 0.003 | -0.398 | -0.185 | 0.082 |
| Sig. (2-tailed) | 0.981 | 0.001 | 0.044 | 0.375 |
Abbreviations: MPV: Mean platelet volume; ESR: Erythrocyte sedimentation rate; PLT: Platelet; PCT: Platelet crit; PDW: Platelet distribution width
Limitations
Limitations of the present study includes the retrospective design and small sample size.
Conclusion
MPV may be used as a supportive marker in addition to other CBC parameters in acute cholecystitis. It has no additional cost and does not expend a lot of time because it is already worked in the CBC. Therefore, it can be used as a marker for diagnosing inflammatory diseases. In addition, further longitudinal studies with larger sample sizes may be beneficial in the evaluation of the MPV in the inflammatory disease.
Abbreviations: n: number; WBC: white blood cell; Hb: haemoglobin; MPV: Mean platelet volume; PLT: Platelet; PCT: Platelet crit; PDW: Platelet distribution width
Abbreviations: MPV: Mean platelet volume; ESR: Erythrocyte sedimentation rate; PLT: Platelet; PCT: Platelet crit; PDW: Platelet distribution width
[1]. A Seker, A Incebiyik, A Kucuk, A Terzi, Y Yucel, Mean Platelet Volume in Patients with Acute and Chronic CholecystitisActa Medica Mediterr 2013 29:515-19. [Google Scholar]
[2]. ABR Barbosa, LRM Ferreira de Souza, RS Pereira, G D’Ippolito, Gallbladder wall thickening at ultrasonography: how to interpret it?Radiol Bras 2011 44(6):381-87. [Google Scholar]
[3]. B Suvak, S Torun, H Yildiz, A Sayilir, Y Yesil, A Tas, Mean platelet volume is a useful indicator of systemic inflammation in cirrhotic patients with ascitic fluid infectionAnn Hepatol 2013 12:294-300. [Google Scholar]
[4]. K Coskun, O Mentes, A Atak, A Aral, M Eryilmaz, O Onguru, Is neopterin a diagnostic marker of acute appendicitis?Ulus Travma Acil Cerrahi Derg 2012 18(1):1-4. [Google Scholar]
[5]. LR Dixon, The complete blood count: physiologic basis and clinical usageJ Perinat Neonatal Nurs 1997 11:1-18. [Google Scholar]
[6]. T Purnak, C Efe, O Yuksel, Y Beyazit, E Ozaslan, E Altiparmak, Mean platelet volume could be a promising biomarker to monitor dietary compliance in celiac diseaseUps J Med Sc 2011 116(1):208-11. [Google Scholar]
[7]. Y Yesil, ME Kuyumcu, M Cankurtaran, B Uz, A Kara, MK Kilic, Increased mean platelet volume (MPV) indicating the vascular risk in Alzheimer's disease (AD)Arch Gerontol Geriatr 2012 55:257-60. [Google Scholar]
[8]. Y Beyazit, A Sayilir, S Torun, B Suvak, Y Yesil, T Purnak, Mean platelet volume as an indicator of disease severity in patients with acute pancreatitisClin Res Hepatol Gastroenterol 2012 36:162-68. [Google Scholar]
[9]. O Yüksel, K Helvaci, O Basar, S Köklü, S Caner, N Helvaci, An overlooked indicator of disease activity in ulcerative colitis: mean platelet volumePlatelets 2009 20:277-81. [Google Scholar]
[10]. B Kisacik, A Tufan, U Kalyoncu, O Karadag, A Akdogan, MA Ozturk, Mean platelet volume (MPV) as an inflammatory marker in ankylosing spondylitis and rheumatoid arthritisJoint Bone Spine 2008 75:291-94. [Google Scholar]
[11]. M Hirota, T Takada, Y Kawarada, Y Nimura, F Miura, K Hirata, Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo GuidelinesJ Hepatobiliary Pancreat Surg 2007 14:78-82. [Google Scholar]
[12]. I Chung, A Choudhury, GY Lip, Platelet activation in acute, decompensated congestive heart failureThromb Res 2007 120:709-13. [Google Scholar]
[13]. S Pikija, D Cvetko, M Hajduk, V Trkulja, Higher mean platelet volume determined shortly after the symptom onset in acute ischemic stroke patients is associated with a larger infarct volume on CT brain scans and with worse clinical outcomeClin Neurol Neurosurg 2009 111:568-73. [Google Scholar]
[14]. AY Gasparyan, A Stavropoulos-Kalinoglou, TE Toms, KM Douglas, GD Kitasn, Association of mean platelet volume with hypertension in rheumatoid arthritisInflamm Allergy Drug Targets 2010 9:45-50. [Google Scholar]
[15]. B Makay, Z Turkyilmaz, E Unsal, Mean platelet volume in children with familial Mediterranean feverClin Rheumatol 2009 28:975-78. [Google Scholar]