Polymorphous Low Grade Adenocarcinoma of Retromolar Region - A Rare Case Report with Distinct Clinical Manifestations
T Radhika1, Nadeem Jeddy2, K.Kamal Kannadasan3, R Aartrthi4, Ramachandra Prabakar5
1Reader, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Golden George Nagar, Chennai, India.
2Professor and Head, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Golden George Nagar, Chennai, India.
3Professor and Head, Department of Oral and Maxillofacial Surgery, Thai Moogambigai Dental College and Hospital, Golden George Nagar, Chennai, India.
4Postgraduate Student, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Golden George Nagar, Chennai, India.
5Professor and Head, Department of Orthodontia, Thai Moogambigai Dental College and Hospital, Golden George Nagar, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. T. Radhika,Reader, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital,Golden George Nagar, Chennai-600107, India.E-mail :radhikasashi26@gmail.com
Polymorphous low grade adenocarcinoma (PLGA) is a rare, low-grade malignancy of minor salivary glands accounting for 2% of salivary gland tumours. The most common sites are palate (60%), lip, buccal mucosa, alveolar ridge and base of the tongue with retromolar region being very rare (0.5%). It is considered to be a low grade malignancy with indolent nature. Very few cases with metastatic spread to lymph nodes and lung have been reported in literature. This report of PLGA is a rare case presenting in an uncommon location (retromolar area) with suspected lymph node and lung metastases.
Low grade malignancy, Lung metastasis, Minor salivary glands, Retromolar area
Case Report
A 59-year-old male reported to the Department of Oral Medicine and Radiology of Thai Moogambigai Dental College and Hospital, Chennai, India with the chief complaint of a painless growth in the right lower back region for past one year. On intraoral examination, a single, solitary, polypoid, sessile growth was seen on the right posterior alveolus in the retromolar region [Table/Fig-1]. The growth was measuring approximately 6x4cm in its greatest dimension, extending from the distal aspect of 48 anteriorly, extending towards the tonsillar region posteriorly, floor of the mouth inferiorly and extends 3cms above the alveolar crest superiorly. The surface of the lesion was irregular with the colour of the adjacent normal mucosa interspersed with areas of erythema. A foci of ulceration was seen on the inferior surface of the growth measuring 0.4cm in diameter approximately. On palpation, inspectory findings of site, size, shape and surface were confirmed. The growth was tender, firm and fixed. On extraoral examination, a single, discrete right submandibular lymph node measuring approximately 2cm in diameter was palpable. It was non-tender, firm and fixed to the underlying structures.
A provisional diagnosis of squamous cell carcinoma was provided by the department of Oral Surgery following which haematological and radiological investigations were done. Baseline haematological parameters were within normal limits except for elevated levels of serum creatinine (2.7mg/dl).
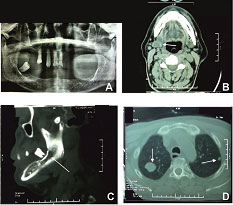
Orthopantamograph (OPG) revealed radiolucency in relation to 48, indicating bony resorption [Table/Fig-2a]. Serial axial Computed
Tomographic (CT) sections of the neck were studied withoutintravenous (i.v.) contrast. IV contrast was deferred due to elevated creatinine levels. CT revealed a well defined proliferative mass measuring 4x3x3.8cm arising from the right side of the mandible obliterating the gingivobuccal sulcus extending to the soft palate, lateral and posterior third of the tongue. The lesion involved the anterior pillar of the tonsillar fossa abutting the pterygoid process and the oropharynx posteriorly on the right side [Table/Fig-2b]. CT impression was consistent with a malignant lesion. Destruction of the body of the mandible was noted on right side adjacent to the lesion with involvement of mandibular canal [Table/Fig-2c]. Enlarged necrotic left sublingual, level IB and level IIA lymphnode involvement was evident. Multiple pulmonary nodules in both the lung fields were an incidental finding and were reported as likely pulmonary metastasis [Table/Fig-2d].
After obtaining informed consent from the patient, an incisional biopsy was taken from the representative area of the lesion which also included the foci of ulceration. The incisional biopsy specimen was received by the Department of Oral Pathology in 10% buffered formalin. Microscopic examination of haematoxylin and eosin stained section revealed uniform round to oval cells arranged in diverse architectural patterns. The lesional cells appeared bland with pale staining vesicular nuclei, eosinophilic cytoplasm arranged in solid, trabecular, tubular and cribriform patterns. Characteristic linear arrangement of the tumour cells in an “Indian file” or “beads on a string” pattern was present[Table/Fig-3a-3f] Perineural invasion was not evident in the given tissue section. Based on the histopathological features, a diagnosis of Polymorphous low grade adenocarcinoma was provided.
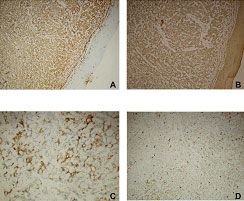
Immunohistochemically, the tumour cells were strongly positive for vimentin and cytokeratin. Focal positivity for C-Kit (CD117) was observed only in the luminal cells. The tumour cells were negative for S100 [Table/Fig-4a-d]. Based on the histopathological and immunohistochemical findings, a final diagnosis of Polymorphous low grade adenocarcinoma was provided. Wide surgical excision of the lesion and lung biopsy was planned. Unfortunately, the patient did not turn up and was lost to follow up.
A solitary sessile polypoid growth in the right posterior alveolus

Radiographic investigations 2a) Orthopantamograph reveals radiolucency in relation to 48 indicating bony resorption 2b) Computed tomography (CT) scan shows well defined proliferative mass in the right side of the mandible 2c) CT scan showing destruction of the body of the mandible 2d) CT scan showing multiple pulmonary nodules in both the lung fields
Histopathologic features (Haematoxylin and eosin stain - H&E) 3a) Tumour mass of glandular origin in the connective tissue exhibiting polymorphous pattern (H&E, 4X) 3b) Solid sheets of uniform round tumour cells with eosinophilic cytoplasm. Duct-like structures are also seen (H&E, 20X) 3c) Tumour cells arranged in trabecular pattern in a hyalinised stroma (H&E, 10X) 3d) Tumour cells arranged in pseudo-cribriform and trabecular pattern (H&E, 10X) 3e) Foci of hyalinisation (H&E, 10X) 3f) Tumour cells arranged in Indian file pattern (H&E, 10X)

Immunohistochemical analysis (10X) 4a) Tumour cells exhibiting strong positivity for vimentin 4b) Tumour cells exhibiting diffuse strong positivity for cytokeratin4c) Tumour cells exhibiting focal positivity for CKit - only luminal cells are positive 4d) S100 negative tumour cells
Discussion
Polymorphous low grade adenocarcinoma is a low grade malignancy presenting histopathologically with morphologically uniform cells exhibiting multiple architectural patterns. The tumour was first described by Freedman and Lummerman (Lobular carcinoma) and Batsakis et al., (Terminal duct carcinoma) in 1983. The term "Polymorphous low grade adenocarcinoma" was coined by Evans and Batsakis in 1984 [1]. PLGA constitutes to around 19% to 26% of malignant tumours of minor salivary glands [2]. The lesion almost exclusively involves minor salivary glands [3]. It is the second most common malignant tumour in minor salivary glands following mucoepidermoid carcinoma [4].
It occurs in a wide age range from 16 to 94 years with a mean age of 59 years and has a female predilection [5]. In the present case report the patient was a 59-year-old male. The most common site for PLGA is palate (60% of cases occur in this region) followed by buccal mucosa, upper lip, retromolar triangle and tongue with retromolar area accounting to only 0.5% of tumours [5-7]. This case report describes PLGA in such a rare location.
Histopathologically, PLGA is characterised by cytologically uniform bland-looking round cells arranged in multiple architectural patterns and hence it is termed as polymorphous. The growth patterns include solid, trabecular, tubular, cribriform, fascicular, microcystic and papillary. Characteristic single-cell arrangement in a linear fashion described as “Indian file” or “beads on a string” pattern is pathognomonic of the tumour. Perineural invasion with “Targetoid pattern” (concentric arrangement of cords of cells around nerves) is common [8]. Solid, trabecular and cribriform areas with "Indian file" arrangement of cells in the periphery was seen in the present case. Other patterns such as tubular, fascicular, microcystic and papillary patterns were not seen in our case. Perineural invasion was not evident in our case.
Microscopically, many features of PLGA mimic other salivary gland tumours such as pleomorphic adenoma (PA) and adenoid cystic carcinoma (ACC). A well circumscribed lesion with a definite capsule and presence of chondromyxoid stroma is suggestive of Pleomorphic adenoma. Characteristic features of PLGA such as cribriform morphology and perineural invasion are not seen in PA. Glial fibrillary acidic protein (GFAP) is a useful immunohistochemical marker in distinguishing PLGA (negative expression) from PA (positive expression).
ACC is more aggressive with poor prognosis and higher metastatic potential. Cells in ACC are basaloid, angular and hyperchromatic compared to the pale staining cuboidal or columnar cells with vesicular nuclei in PLGA. Cribriform pattern is predominant in ACC compared to the polymorphous pattern in PLGA. Necrosis, nuclear pleomorphism and increased mitotic activity are present in ACC but not in PLGA [1,4,9]. The present case was composed of uniform round to oval cells arranged in polymorphous pattern - Solid, trabecular, tubular and cribriform. The lesional cells exhibit eosinophilic cytoplasm with pale staining and vesicular nuclei. There was no evidence of pleomorphism or Increased mitotic activity.
Immunohistochemically, PLGA is positive for Vimentin and cytokeratin. The tumour exhibits variable positivity for S100. IHC has been reported to be useful in distinguishing PLGA from ACC and PA. C-Kit (CD117) and CD 43 are strongly positive in Adenoid cystic carcinoma whereas only focal or no positivity is seen in PLGA [10]. PA exhibits strong positivity for Glial fibrillary acidic protein but the marker is negative in PLGA. However, some authors consider immunohistochemistry to be non-contributory in distinguishing these neoplasms [11].
Surgical excision with wide margins is the recommended treatment for the primary lesion [3]. In some cases, modified radical neck dissection is indicated. Long term follow up is essential as recurrences and transformation into high grade malignancy even many years after initial surgery have been documented [12,13].
Conclusion
PLGA has been designated as a low grade malignancy. However, reports of aggressive cases with distant metastases question its indolent nature. Awareness on distinct clinical manifestations of the tumour such as involvement of rare sites, recurrence and metastases is essential to facilitate early diagnosis and provide appropriate treatment to aid in better prognosis.
[1]. A Shah, S Patel, J Pathak, N Swain, S Shah, An insight into diagnostically [1]challenging salivary gland malignancy with case report: Polymorphous low grade adenocarcinoma.Journal of Dental Research and Scientific Development 2014 1:20-23. [Google Scholar]
[2]. K Takubo, R Doi, K Kidani, M Nakabayashi, M Sonoda, F Ohtake, Polymorphous Low Grade Adenocarcinoma Arising at the Retromolar Region: A Rare Case of High-Grade Malignancy.Yonago Acta medica 2007 50:17-22. [Google Scholar]
[3]. SV Jagtap, PG Chougule, DB Nikumbh, SR Kanetkar, G Jain, Polymorphous Low Grade Adenocarcinoma Presenting as Recurrent Oral UlcerationsJCDR. 2012 6:712-14. [Google Scholar]
[4]. AA Olusanya, OA Akadiri, VI Akinmoladun, BF Adeyemi, Polymorphous Low Grade Adenocarcinoma: Literature Review and Report of Lower Lip Lesion with Suspected Lung Metastasis.J Maxillofac Oral Surg 2011 10:60-63. [Google Scholar]
[5]. L Ruiz-Godoy, L Suarez, A Mosqueda, A Meneses, Polymorphous low grade adenocarcinoma of the parotid gland. Case report and review of the literatureMed Oral Patol Oral Cir Bucal 2007 12:E30-33. [Google Scholar]
[6]. R Gupta, K Gupta, R Gupta, Polymorphous low grade adenocarcinoma of the tongue: a case report.Journal of Medical Case Reports 2009 3:9313 [Google Scholar]
[7]. AM Barasoain, VFJ Martin, GE De La Fuente, SJ Santamaria, A Pampin – Franco, JL Lopez-Estebaranz, Polymorphous low-grade adenocarcinoma in the upper lip: a well-described but infrequently recognized tumourDermat Online J 2013 19:19265 [Google Scholar]
[8]. RH Simpson, EM Pereira, AC Ribeiro, Polymorphous low grade adenocarcinoma of the salivary glands with transformation to high-grade carcinoma.Histopathology. 2002 41:250-59. [Google Scholar]
[9]. SD Chandekar, SS Dantkale, RR Narkhede, SV Chavhan, K Birla, Swelling on the hard palate presenting as Polymorphous Low Grade Adenocarcinoma: A Case Report and Review Of Literature.J of Evolution of Med and Dent Sci 2014 3(36):9484-88. [Google Scholar]
[10]. JM Salehinejad, N Mohtasham, A Bagherpour, Abbaszadeh-bidokhty H, Ala Ghazi. Evaluation of c-kit protein (CD117) expression in common salivary gland neoplasms.J Oral Maxillofac Pathol 2014 18:177-82. [Google Scholar]
[11]. N Zaib, S Mushtaq, N Mamoon, N Akhter, B Ayaz, Immunohistochemical Pattern of Pleomorphic Adenoma, Polymorphous Low Grade Adenocarcinoma and Adenoid Cystic Carcinoma in Minor Salivary Glands.J Dent (Tehran). 2014 11:38-46. [Google Scholar]
[12]. JT Castle, LD Thompson, RA Frommelt, Polymorphous low grade adenocarcinoma: a clinicopathologic study of 164 casesCancer. 1999 86:207-19. [Google Scholar]
[13]. TA Fife, B Smith, CA Sullivan, JD Browne, JD Waltonen, Polymorphous low-grade adenocarcinoma: a 17 patient case series.Am J Otolaryngol 2013 34:445-48. [Google Scholar]