Oral health related quality of life (OHRQoL) is that aspect of dentistry which looks into the patient’s own perception of his or her oral health status and its impact upon his or her quality of life which includes social well being and emotional well being. OHRQoL includes different domains like esthetics which affects smiling, laughing and talking which in turn affects our social well being. It also includes the functional aspect of teeth and oral cavity like efficacy of mastication and other aspects like absence of symptoms like pain and hypersensitivity [1]. Smile is one of the most effective measures by which people convey their emotions and from a social point of view a beautiful smile is an added asset to a beautiful face. Children, with or without smiling, communicate whether they are happy or sad, confident or uncertain [2]. Children’s smiling patterns are influenced by oral health related quality of life in two ways, the psychological aspect which includes the child’s self perception of their own smile and the social aspect which includes the degree to which they have an open and relaxed smile. To obtain information on child’s oral health related quality of life, it is necessary to develop questionnaires, which take into account a number of domains i.e. oral symptoms, functional limitations, emotional well being, and family well being/parental distress [3,4].
In the past, socio-dental indicators used in oral epidemiology as a single measure of impact of clinical diseases did not document the full impact of oral diseases. These indicators were constructed and tested in epidemiological studies on different population but most of these studies have been conducted in adult and older population [5]. Because traumatic injuries to the teeth are very common, present study was undertaken to assess the impact of these injuries on the oral health status, oral health related quality of life based on the child’s perception, parent perception and correlation between the child’s oral health status with their smiling pattern in 58 children in the age group of 5–15 years in Bengaluru city, India.
Materials and Methods
A randomized controlled hospital based study was conducted in the Department of Pedodontics and Preventive dentistry, KLE’S Institute of Dental Sciences, Bengaluru in 2014 to assess the impact of fractured anterior teeth on the oral health status, oral health related quality of life based on the child’s perception, parent perception and the correlation between the child’s oral health status with their smiling pattern in 58 children in the age group of 5–15 years in Bengaluru city. The study sample was divided into 2 groups, Trauma group and Control group. The trauma group consisted of 29 children with 10 boys and 19 girls and control group consisted of 29 children with 10 boys and 19 girls.
Children in the trauma group were examined for traumatized anterior teeth. The selected subjects and their parents were informed about the study and they were asked to sign on consent form after which the parents responded to survey concerning their children’s oral health related quality of life and smiling patterns. Similarly children with good oral health were selected for the control group and their parents were informed about the study and they were asked to sign on consent form after which the parents responded to survey concerning their children’s oral health related quality of life and smiling patterns.
Child perception Questionnaire: Child survey was conducted by using Michigan’s Oral Health Related Quality of Life Scale - child version [6]. The children answered these questions with a simple YES/NO. The sum of YES answers was used as an indicator of children’s self evaluation of their smiles.
Parent perception questionnaire and proxy questionnaire: The participating parents were asked to fill the questionnaire based on Michigan’s Oral Health Related Quality of Life Scale - parent version [7]. The questions were divided into 4 indices while calculating the parent perception score. Index 1 was for the parents ‘proxy assessment’ of their children’s satisfaction with their smiles. The questions included in this index were “my child likes his/her smile”, “my child is happy with his/her teeth”. Index 2 represented the parent’s perception of their children’s smile with an “impact score”. The questions included in this index were “how much do you think that the health of your child’s teeth affect the way your child smiles?” and how much do you think the condition of your child’s teeth affect the way your child feels about herself/himself ? Likert’s type rating scale was used for index 1 and 2 while index 3 and 4 were the numbers of positive and number of negative adjectives selected to describe their children’s smile out of the nine adjectives like ‘happy’, ‘reserved’, ‘wide smile’, ‘shows teeth’, ‘hides teeth’, ‘hesitant’, ‘shy’, ‘open mouth’ and ‘closed mouth’. The number of positive items and number of negative items were calculated by adding 1 point each for checking the adjectives.
Selection of cartoon films: Cartoon watching is one of the favourite hobbies of children these days. It has been observed that Cartoon Network is the favourite channel among 68% children between the age group of 2 to 17 years. It was also observed that Tom and Jerry was ranked as best cartoon among these children [8]. The cartoon films of Tom and Jerry and Chip and Dale of 4 minutes 30 seconds were carefully selected based on the subject’s age. In the present study for subjects of 5 to 7 years of age, the cartoon films that were funny, easy to understand and had no script were selected while subjects of 8 to 10 years and 11 to 15 years were shown funny Tom and Jerry cartoons with scripts.
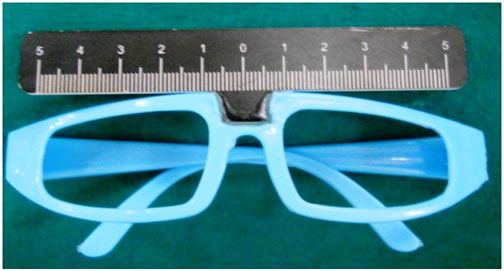
Video based smile assessment: The selected subjects were asked to watch a short cartoon film in a room by themselves. While they watched the video, their faces were being videotaped with an in built webcam in Lenovo laptop model 550 using the Windows live movie maker software. The camera of the laptop was set approximately 25 cm away from the sitting subject. The subjects were instructed to hold their head in natural head position by looking straight into the laptop screen [Table/Fig-1]. If position required correction the researcher helped the subject into natural head orientation. The camera was adjusted and focused on to the subjects face. The subjects were asked to wear the eye gear with the attached ruler with millimeter markings while watching the video [Table/Fig-2]. The recording was started as soon as the funny cartoon film started.
Child watching cartoon film wearing smile measurement scale 152x101mm (300 x 300 DPI)

Smile measurement scale 381 x 203mm (300 x 300 DPI)
After watching the cartoon, the children answered questions concerning their oral health and smiling patterns. The digital recordings were downloaded to the system. A segment of these tapes starting at a certain point in the movie that was 5 seconds before a funny sequence began and lasting for 2 minutes and 30 seconds was cropped for smile analysis and uploaded to the Wonder share video editor software program and converted into 25 jpeg still frames and then renamed with Microsoft windows 7 with appropriate subject number [Table/Fig-3].
25 still frames the smile recorded using Wonder share Video editor software 304 x 254mm (300 x 300 DPI)

Measurements on smile frame: Each file was opened in adobe Photoshop with a resolution of 320 x 240 pixels. The ruler function was chosen on the adobe Photoshop and set to millimeter. The measurement obtained were entered into Microsoft excel. The first measurement was a base line measurement 6 seconds before the beginning of the funny segment of the video. The next 25 measurements were spaced every 6 seconds from the time this funny sequence started. For each measurement point, three measurements were made namely–the child’s smile width in mm (outer commissural width), the child’s smile height in mm (inter labial height at smile), and the visible maxillary dental width (number of maxillary incisor display). These three indicators were chosen based on consideration concerning the measured of facial expressions.
Smile index (ratio of smile width and smile height) was determined by standardizing each of the 25 width measurements by dividing it with the child’s base line smile measurement before the funny sequence of the movies started. These 25 standardized scores were averaged. A score of “1” would indicate that the child’s mouth width at baseline and when watching the movie did not change, while a score of <1 would indicate that the child’s mouth was narrower when watching the funny movie and a score >1 that is wider was given.
Results
Correlation of Oral health indicators, Self evaluation by children, parents’ evaluations, and video based assessments of children’s smiles
Using Pearson’s correlation coefficient we correlated the children’s self evaluations of their smiles–as measured with the number of positive self descriptions–and found a significant correlation between the average ratings of the video-based smile assessment that is “width of the smile” and “number of teeth shown during smiling”. In addition the correlation between the number of traumatized teeth and mouth openness was found to be significant [Table/Fig-4]. However, no significant correlation was found between the negative adjectives used by the parents and the smiling pattern.
Correlations between children self report, the parents proxy and own assessments based on video smile assessment
| Smile parameters | Children self report | Proxy s core | Impact score | Number of positive adjectives | Number of negative adjectives | Number of Traumatized teeth |
|---|
| Width of smile | r=0.395,p=0.042* | r=0.456,p=0.017* | 0.932,NS | 0.45, NS | 0.448,NS | 0.869,NS |
| Mouth Opening | 0.154,NS | 0.307,NS | r=0.904,p=0.018* | 0.22,NS | 0.594,NS | r=0.405,p=0.036* |
| Number of teeth shown | r=0.045,p= 0.012* | 0.217,NS | 0.725,NS | 0.904,p<0.001* | 0.335,NS | 0.635,NS |
*statistically significant
The more the parents thought that a traumatized tooth kept their child from smiling, the less positive the children were about their smiles. However, the more positive the children were about their smiles, the more positive adjectives the parents had chosen to describe their children’s smile and a significant correlation was found between the positive adjectives used by the parents to describe the smile and number of teeth shown during smiling. The impact score i.e. “how much do you think that the health of your child’s teeth affect the way your child smiles?” Was correlated with the mouth openness and was found to be highly significant. It was also seen that more the number of traumatized teeth in the child’s mouth, less was the mouth opening during smiling. In summary, the results supported the hypothesis that responded to children’s self evaluations of their smiles correlated with the video based assessments of their smiles, parents’/guardians’ evaluations of their children’s smiles and their oral health status.
Comparison of the smiling patterns in trauma group and control group
On comparison of the smiling patterns in trauma group and control group using student’s t-test it was seen that there was a highly significant difference in the smiling pattern in the trauma group and control group with p-value less than 0.001 [Table/Fig-5].
Comparison of smiling pattern in Trauma and Control group
| Mean±S.D | t-value | P -value | Result |
|---|
| Trauma | 7.01±1.51 | 19.47 | <0.001 | Highly significant |
| Control group | 5.06±1.2 |
This supports the hypothesis that children in control group were more positive about their smiles when compared with the trauma group.
Discussion
OHRQOL measures are being increasingly used to measure the impact of various oral diseases on the general population and in the recognition of high risk groups in order to understand the success of various preventive and curative procedures on improving the quality of life of an individual [9]. As children grow, they experience various dental problems like dental caries, malocclusions, dental injuries and consequences of previous dental traumas. Various studies have been reported on the effect of these dental problems on the OHRQoL. The present study focuses on the effect of trauma on the OHRQL. Due to decreased experience and coping skills, children of younger age will undergo more of physical trauma than psychological trauma where as the older children may have broader experience with pain and seem better able to manage the pain aspect of injury which will diminish more rapidly than the psychological effects of the quality of life [10].
In the present study it was seen that children affected by dental trauma reported negatively to the OHRQoL questionnaire and they were more hesitant to smile and show their teeth. These findings in the present study are similar to the results of a study conducted on Bendo CB et al., on the OHRQoL and traumatic dental injuries in Brazilian adolescents where the adolescents with more severe untreated TDI, such as fractures involving dentin and/or pulp, were more likely to self-report a higher negative impact on their OHRQoL than those without TDI [11].
A study by Abanto J et al., showed that dental injuries had a negative impact on the OHRQoL of pre-school children and their parents. Dental injuries especially involving exposure of the pulp tissue may require the family to dedicate a considerable amount of time to addressing the child’s symptoms [12].
There existed a positive and significant correlation between the proxy parent’s perception of child’s oral status (affected by dental trauma) and the width of the child smile. Proxy score was considered in this study as there was little evidence to show that preschool-aged children could provide valid and reliable assessments of their own OHRQoL [13].
The more the parents thought that a traumatized tooth kept their child from smiling, the less positive the children were about their smiles. The parents used more negative adjectives to describe the smile of their children affected by dental trauma. This finding was in par with a study conducted by Siqueria M B et al., which showed that the evaluation of parents regarding the oral health of their children and a history of trauma were associated with a negative impact on quality of life of the Children [14].
It was also seen that children with fractured incisors were significantly more dissatisfied with the appearance of their teeth than are children without any traumatic injury.
Difficulties with ‘eating and enjoying food’ were also more frequently experienced by children with fractured teeth than without fractured teeth. Children with fractured teeth were more concerned with aesthetics than with function. Thus proving that dental trauma had a negative effect on the smile – related quality of life in children. These findings were similar to results of a study conducted by Feldens CA et al., on the Traumatic dental injuries in the first year of life and associated factors in Brazilian infants [15].
In the intergroup comparison of smiles of the children with anterior permanent teeth fracture with control group, it was seen that children with anterior permanent tooth fracture were less positive in describing their self assessed smiles when compared to their healthy counterparts. The children in the control group showed more teeth when they smiled and the width of their smile too was more than the baseline width. These results are in par with the results of a Canadian study by Cortes et al., on the impact of traumatic injuries to the permanent teeth on the OHRQoL in 12–14-year-old children [16,17].
A study conducted by Piovesan et al., in Brazil on 792 children on the child’s OHRQL and socioeconomic factors associated with traumatic dental injuries in school children showed that dental traumatic injuries had no effect on the child’s quality of life but in our present study we found that dental trauma not only affected the children OHRQL but also their parent’s perception about their child’s oral health [18].
The parent’s evaluation and proxy evaluation of the smiles of their children in the anterior teeth fracture group did not differ from the children’s self assessment of their smiles, it was observed that parent’s own evaluation was more stronger when compared to their proxy assessments. The parents were more affected by the dental health of the child after trauma. The results of our study supported the hypothesis that traumatic injury to anterior teeth significantly affected the quality of life in children and their smiling pattern.
Smile Analysis
It was seen that as the number of traumatized teeth and severity of dental trauma increased, the smile width and number of teeth shown during smiling decreased the smile ratio was significantly less compared to the control group. This finding was very similar to the data put forth by Patel RR et al.,
Limitations of the Study
A possible limitation of this study was the fact that the children participated in this research while they were at a regularly scheduled dental appointment. It is possible that they would have expressed more positive emotions and smiled more while watching the movie if they had not been in a dental clinic awaiting dental treatment.
In the present study the web camera used for recording the smiles was of a lower resolution which caused mild distortion of the images used for measuring smile. The future development of sophisticated software to measure the video-based smile characteristics would improve the already high reliability of these measurements.
Conclusion
Children develop a concern for their esthetic appearance at a very young age which may later affect their personality development. Children with untreated traumatic injuries to anterior teeth were more likely to experience a negative impact on social wellbeing, especially with regard to avoiding smiling or laughing and being more concerned about what other people may think or comment. The findings of this study add yet another reason to the set of arguments that stresses the importance of promoting good oral healthcare practices to prevent oral disease in children, and to meet children’s unmet oral healthcare needs. These findings will hopefully add to the growing evidence that child advocates can use to inform policy makers about the significance of good oral health for children’s lives.