Anaesthesia for a “Scalped” Patient
M.M. Rizvi1, Raj Bahadur Singh2, Arindam Sarkar3, Sanjay Choubey4
1 Assistant Professor, Department of Anaesthesiology and Critical Care, Era’s Lucknow Medical College and Hospital, Lucknow, India.
2 Assistant Professor, Department of Anaesthesiology and Critical Care, Era’s Lucknow Medical College and Hospital, Lucknow, India.
3 Assistant Professor, Department of Anaesthesiology and Critical Care, Era’s Lucknow Medical College and Hospital, Lucknow, India.
4 Professor, Department of Anaesthesiology and Critical Care, Era’s Lucknow Medical College and Hospital, Lucknow, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raj Bahadur Singh, Assistant Professor, Department of Anaesthesiology and Critical Care, Era’s Lucknow Medical College and Hospital, Lucknow-226003 India. E-mail : virgodocraj36@yahoo.co.in
Trichilemmal carcinoma of scalp is a rare malignant tumour of scalp. A 52-year-old female presented with an extensive ulcerative lesion of the scalp. As the location of the tumour was in the occipital region and there was loss of bony skull in the region, this case became challenging. This patient was managed in the left lateral which was a difficult situation for even the experienced Anaesthesiologist. Intravenous access was acquired, central venous catheter (CVC) was placed in the right internal jugular vein under ultrasonography (USG) guidance and intubation was carried out in the lateral position. After the procedure, patient was again returned to the left lateral position. The trachea was extubated in the lateral position once the patient was awake, after thorough reversal of neuromuscular blockade. Patient had an uneventful postoperative period. This case report highlights the management of an unusual case of Trichilemmal carcinoma of the scalp.
Cutaneous, Lateral position, Occipital region, Trichilemmal carcinoma
Case Report
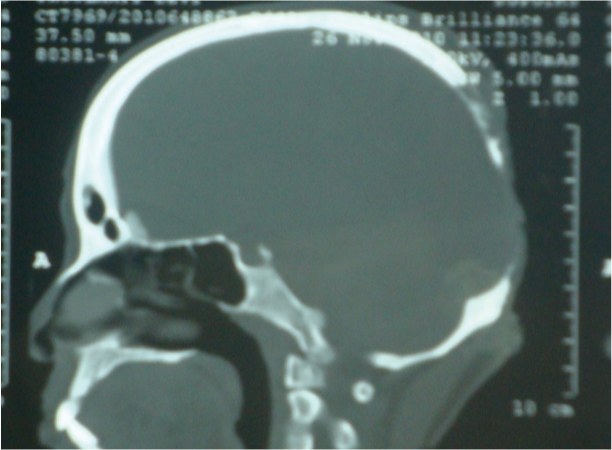
A 52-year-old female presented to the Neurosurgery outpatient department for a painless, extensive ulcerative lesion of the scalp, in the occipital region [Table/Fig-1,2]. The patient had this lesion for the past two years, initially it was the size of a coin however, it gradually progressed to the present size. A provisional diagnosis of Trichilemmal carcinoma of scalp was established after FNAC and the plan was to give a flap cover to the exposed area, along with clearing the Duramater of adhesions and a cranioplasty. Neurosurgeons and Plastic surgeons were involved in the management of the case. Initial lab workup of the case showed a baseline Haemoglobin of 12.2 gm%. Other relevant investigations were within normal limits. Spiral CT scan with 3D reconstruction image [Table/Fig-3&4] showed that the lesion had invaded into the skull and there was a huge defect in the skull and the brain was lying unprotected in the region of the tumour (without bony skull to protect it).
Lesion of Scalp from Back

Lesion of Scalp from side

Sagital view of the skull showing bony destruction due to invasive tumour
Spiral CT scan with 3D reconstruction from the back

The Duramater could be seen pulsating, reflecting cerebral pulsations. Her weight was 55 kg and relevant airway examination was done, and did not reveal any difficulty in airway management as mouth opening was adequate, full range of neck movements were possible and the Modified Mallampatti Grade was I. Patient was pre-medicated with alprazolam 0.5mg PO, the night before surgery and advised a fast of eight hours for solids and two hours for clear liquids. After wheeling the patient into the operation theatre, standard monitoring was placed as per American Society of Anaesthesiologists (ASA) guidelines (ECG, NIBP, SPO2, ETCO2 after induction, Temperature probe after intubation). The patient was placed in the left lateral position, which she preferred on her own and intravenous access was acquired under local anaesthesia. Pre-oxygenation was done with 100% oxygen for three minutes prior to induction of anaesthesia. She was co-induced with intravenous midazolam 1mg followed by intravenous Fentanyl 100mcgs and thiopentone 5mg/kg titrated, to eyelash reflex. Prior to administration of vecuronium 0.1mg/kg, adequate bag and mask ventilation (BMV) was confirmed. After administration of vecuronium, patient was ventilated for 5 minutes, to attain good intubating conditions. After this, direct laryngoscopy was done in the lateral position, revealing a Cormack and Lehane Grade I of the glottis. The trachea was intubated smoothly and swiftly with a flexo-mettallic endotracheal tube (7.5 ID). Tracheal intubation was confirmed with auscultation and end-tidal capnography (ETCO2).
Endotracheal tube was secured nicely with tincture benzoin and Dura pore adhesive tape. A Central venous catheter (CVC) 7 French, triple lumen was placed in the right internal jugular vein under ultrasonography (USG) guidance in the lateral position, as the surgery was presumed to be quite extensive and lengthy. Left radial artery was cannulated and arterial blood pressure was obtained by means of transducer. A Foley’s catheter was passed aseptically and urine output was monitored throughout the surgery. Patient was positioned, prone as per the neurosurgery team. All invasive lines, monitors and ETT were checked post positioning to rule out any kink, disconnection or migration. Anaesthesia was maintained with Isoflurane in oxygen and nitrous oxide gas mixture, titrated to the depth of anaesthesia. Intermittent boluses of vecuronium were given to maintain adequate muscle relaxation and prevent coughing on the tube. The surgical procedure lasted for eight hours, in which the neurosurgery team removed the invasive growth adjacent to dural sinuses followed by cranioplasty and a trapezius flap over the lesion.
Body temperature was continuously monitored and patient was kept warm with means of an in-line warmer and a forced air warmer. Blood loss was substantial from the bony edges of the skull and patient was transfused two units of packed cells to maintain oxygen delivery. After the procedure, patient was again returned to the left lateral position. The trachea was extubated in the lateral position once the patient was awake, after thorough reversal of neuromuscular blockade with neostigmine and glycopyrrolate. The patient was shifted to neurosurgery intensive care unit for postoperative care and managed in the lateral decubitus position. Her postoperative period was uneventful and she was discharged from Neurosurgery ICU on Day 4 of her surgery.
Discussion
Malignant proliferating trichilemmal tumour (MPTT) is a rare cutaneous malignancy that occurs on the sun-exposed areas. It usually occurs in elderly women [1] and predominantly affecting the scalp, eyelids, neck and face. A review of the literature reveals MPTT to be a neoplasm of the older age group [2-4]. It can be seen in both immunocompetent and immunosuppressed hosts [5]. Simply the patient’s scalp is destroyed, along with bony skull in the region and the Duramater lies exposed, hence the term “Scalped”.
Malignant proliferating trichilemmal tumour is an extremely uncommon tumour [6], and was originally described in 1983 by Saida et al [2,7]. The tumour may lie dormant for years and then start expanding suddenly and is treated by surgical excision [8,9]. Simply excise adequate margins and it is safe, inexpensive and effective treatment of trichilemmal carcinoma [10,11].
This case was definitely a challenge to the anaesthesia team, with two main issues at hand: 1) Airway Management (mask ventilation and laryngoscopy and intubation) 2) Preventing injury to unprotect brain and venous sinuses. We had to be able to perform all tasks, with a patient in the lateral position without causing any undue pressure on the exposed cranial structures. Pre-oxygenation and bag and mask ventilation were done without any difficulty, in this case and laryngoscopy and intubation were straightforward as well, but it required an experienced operator. A neatly folded drape sheet was kept under the head and neck, to support the head and neck and patient was maintained by two attendants in the lateral position, this was crucial in airway management in the lateral position.
Endotracheal intubation using direct laryngoscopy for patients in the lateral decubitus position may be an unfamiliar technique for many Anaesthesiologists. The difficulty with patients lying in the right lateral decubitus position is the positioning of the tongue, which (influenced by gravity) has a tendency to slip off the laryngoscope blade while the blade is being inserted from the right side of the tongue and moved centrally, upwards, there thus being a need to shift the tongue to the left side [12]. This is why our patient was positioned in the left lateral position deliberately, so as to facilitate laryngoscopy for a right handed Anaesthesiologist, although it did make bag-mask ventilation slightly difficult. However, this was managed with an efficient jaw thrust.
Other techniques to secure airway in lateral position are by using Trachlight or classic LMA or ILMA [13-16]. But these have been described for sudden accidental loss of the airway’s patency while lying in the lateral position.
Conclusion
This case report attempts to highlight that the Anaesthesiologist must be prepared to provide anaesthesia as demanded by the clinical situation. We describe the successful management of the airway, i.e. Mask ventilation, laryngoscopy, intubation and extubation in the lateral position in a “scalped” patient. It is obvious that practicing in routine cases by simulating the lateral position, our management skills will improve so that we may be prepared for the unexpected.
[1]. Karamese M, Akatekin A, Abaci M, Tosun Z, Keskin M, Unusual Invasion of Trichilemmal Tumors: Two Case ReportsModern Plastic Surgery 2012 2(3):54-57. [Google Scholar]
[2]. Rao S, Ramkrishna R, Kamakshi D, Chakravarthi S, Sundaram S, Pratibha D, Malignant proliferating trichilemmal tumour presenting early in life: An uncommon featureJ Cutan Aesthet Surg 2011 4(1):51-55. [Google Scholar]
[3]. Trabelsi A, Stita W, Gharbi O, Kanani N, Sriha B, Korbi S, Malignant proliferating trichilemmal tumour of the scalp: A case reportDermatol Online J 2008 14:11 [Google Scholar]
[4]. Garg PK, Dangi A, Khurana N, Hadke NS, Malignant proliferating trichilemmal cyst: A case report with review of literatureMalays J Pathol 2009 31:71-76. [Google Scholar]
[5]. Garrett AB, Azmi FH, Ogburia KS, Trichilemmal carcinoma: a rare cutaneous malignancy: a report of two casesDermatol Surg 2004 30(1):113-15. [Google Scholar]
[6]. Alsaad KO, Obaidat NA, Ghazarian D, Skin adnexal neoplasms-part 1: An approach to tumours of the pilosebaceous unitClin Pathol 2007 60:129-44. [Google Scholar]
[7]. Saida T, Oohara K, Hori Y, Tsuchiya S, Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cystsDermatologica 1983 166:203-08. [Google Scholar]
[8]. Nemetz MA, Cunha RM, Reeck P, Carreirão Neto W, Moreira MTS, Coelho MS, Carcinoma triquilemal: relato de um casoRev Bras Otorrinolaringol 2004 70:832-35. [Google Scholar]
[9]. Boscaino A, Terracciano LM, Donofrio V, Ferrara G, De Rosa G, Trichilemmal carcinoma: a study of seven casesJ Cutan Pathol 1992 19:94-99. [Google Scholar]
[10]. Peryassú BC, Peryassú RC, Peryassú MA, Maceira JP, Ramos-E-Silva M, Trichilemmal carcinoma - a rare tumour: case reportActa Dermatovenerol Croat 2008 16:28-30. [Google Scholar]
[11]. Wong TY, Suster S, Trichilemmal carcinoma. A clinicopathologic study of 13 casesAm J Dermatopathol 1994 16:463-73. [Google Scholar]
[12]. Cupitt JM, Induction of anaesthesia in morbidly obese patientsBr JAnaesth 1999 83:964-65. [Google Scholar]
[13]. Goyal K, Rath GP, Chowdhury T, Mahajan C, Boneless occiput and awake fibreoptic intubation in lateral positionIndian Journal of Anaesthesia 2010 54(3):265-6.doi:10.4103/0019-5049.65355 [Google Scholar]
[14]. Biswas BK, Agarwal B, Bhattacharyya P, Badhani UK, Bhattarai B, Intubating laryngeal mask for airway management in lateral decubitus state: comparative study of right and left lateral positionsBr J Anaesth 2005 95:715-18. [Google Scholar]
[15]. Dimitriou V, Voyagis GS, Iatrou C, Brimacombe J, Flexible lightwand-guided intubation using the intubating laryngeal mask airway in the supine, right, and left lateral positions in healthy patients by experienced usersAnesth Analg 2003 96:896-98. [Google Scholar]
[16]. Cheng KI, Chu KS, Chau SW, Ying SL, Hsu HT, Chang YL, Lightwand-assisted intubation of patients in the lateral decubitus positionAnesth Analg 2004 99:279-83. [Google Scholar]