Introduction
Inguinal hernia repair is one of the most frequently performed surgeries by a general surgeon and so even modest improvement in clinical outcome is important. The most important criteria for the choice of method are safety, recurrence rate and satisfaction to the patient. Numerous studies have been done to decide on the most suitable technique, but there is no general agreement regarding the same and search for a near perfect modality of treatment of inguinal hernia has not yet ended. Tension-free mesh repairs for adult inguinal hernias were originally popularized by Lichtenstein et al., [1] and have been popular ever since then. The other most commonly used techniques include the ‘plug & patch’ method of Robbins & Rutkow [2] , ‘pre-peritoneal’ approach of Nyhus [3] or Kugel [4] and, combined anterior and posterior repair using Prolene® Hernia System (PHS) [5] .
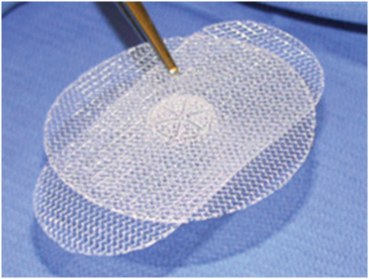
The Prolene® Hernia System (Ethicon; Somerville, NJ, USA) is a novel device developed for tension-free repair of inguinal hernia. It consists of two layers of polypropylene mesh joined by the connector, which provides three-point protection [Table/Fig-1] [6] .
• An ‘underlay’ mesh that is placed in the pre-peritoneal plane, like in Kugel or Nyhus pre-peritoneal repair.
• An ‘onlay’ mesh placed over the floor of the inguinal canal, similar to that used in Lichtenstein repair.
• A ‘connecting’ cylinder between the two plugging the deep ring, like in Robbin & Rutkow’s plug repair.
Few direct comparative studies have been done in the past between LHR and PHS [7-12] , but the latter technique is still not very popular in this part of the country. Hence, through this prospective and randomized study we aim to compare Prolene® Hernia System (PHS) repair with Lichtenstein Hernia Repair (LHR) for inguinal hernias and evaluate whether it has a favorable post-operative outcome in comparison to LHR.
Materials and Methods
A prospective and randomized comparative study was conducted over a period of two years from October 2011 to September 2013 in Department of General Surgery, People’s College of Medical Sciences and Research Centre, Bhopal. Total 64 patients were randomized by ‘odd and even’ method to undergo either Lichtenstein Hernia Repair (LHR) or Prolene® Hernia System Repair (PHS), thereby forming 2 groups of study population. Three patients with bilateral inguinal hernia were taken as two separate cases of right and left sided inguinal hernia, taking the final sample size to 67. All patients with age > 18 years and either having direct, indirect or mixed hernias were included in the study. Exclusion criteria were age <18 years, complicated hernia, recurrent hernia, BMI > 36, ASA Grade IV & V, and simultaneous any other surgical procedure being undertaken like TURP.
Approval from Institutional Research and Ethical Committees was taken before starting the study. Patients were counselled regarding the study and procedure, and written consent obtained prior to enrollment. The cost of the polypropylene mesh and PHS device was borne by the authors. Pre-op assessment and diagnosis was done clinically and relevant investigations carried out for pre-anaesthetic check-up. Patient’s characteristics, diagnosis, operative procedure including various outcome measures and follow-up visits were recorded in a fixed pro forma.
Outcome Measures
They included the following: duration of surgery, pain after surgery and requirement of analgesia, post-operative complications, time to return to normal activity, chronic groin pain, and recurrence of hernia.
Operative Procedure
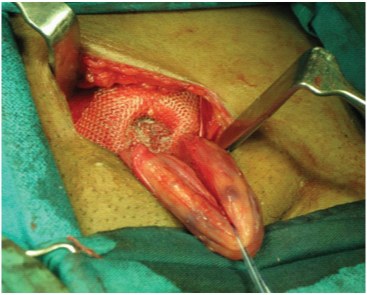
All the cases were done under regional or general anaesthesia. Pre-op antibiotic shot of 3rd generation cephalosporin was given to all the patients. Surgery was done by the same team of surgeons. Duration of surgery was the time taken from skin incision to last suture in minutes. Lichtenstein’s repair was done as described by Amid et al., [13] . In PHS repair entry to the pre-peritoneal space was gained through the internal ring in indirect hernias, or medial defect in direct hernias. PHS comes in three sizes: medium, large and extended. According to the need appropriate size was selected so as to get maximum protection. The circular sheet was deployed in the pre-peritoneal space, created by finger or gauze dissection with the connector coming out through the deep ring or medial defect, and rectangular sheet was placed over the floor of the inguinal canal [Table/Fig-2,3,4,5]. The cord was brought out through the slit (fish mouth) in the lateral or medial part of the external sheet depending upon indirect or direct hernia respectively and neo-ring closed around the cord. Single 2-0 polypropylene/nylon suture used to fix the onlay mesh at pubic tubercle. Hence, the underlay patch covers all three triangles of the groin (myopectineal orifice), and repairs and prevents the recurrence of indirect, direct and femoral hernias; the onlay patch covers the entire floor of inguinal canal and overlaps the pubic tubercle for added support; and the connector joins underlay and overlay patches virtually eliminating migration of the mesh. In addition minimal suturing secures the entire device. Intra-operative observation was done for any specific complication or difficulties.
Post-operative Care
Postoperatively, inj. diclofenac sodium 75 mg i/m was given as analgesic 12 hourly on day of surgery to both the groups, and subsequently as oral tablets on demand. Pain was measured with help of Wong-Baker FACES Pain Rating Scale on next morning. Requirement of analgesia was measured in days for which patient required analgesic medication. Early complications like seroma, hematoma, and wound infections were noted during hospital stay and also during follow-up.
Return to normal activity is taken in days in which patient sits, stands straight, and goes to bathroom, walks, and take steps without complaining of pain or discomfort. As a practice patients were usually not discharged prior to 3 days when the wound was first inspected.
Follow-up
Patients were followed up with first visit after seven days of discharge and subsequently after 3 months, 6 months and then every 6 months thereafter for a maximum of 18 months. They were clinically examined specifically for recurrence of hernia and chronic groin pain (inguinodynia).
Statistical Analysis
The continuous variables are presented as average mean and standard deviation (SD), while categorical variable as absolute number and percentage. The parametric data is analysed by ‘Student’s t-test for unpaired samples’, while non-parametric data is analysed using ‘chi-square test’ or ‘Fisher’s-exact test’, depending upon the data figure more than or less than 5 respectively. Pain score was analysed using ‘Mann-Whitney U-test’. p-value of <0.05 was taken as statistically significant.
Results
Out of total 67 cases, 34 underwent LHR and 33 PHS repair. The patient’s characteristics were comparable in the two groups [Table/Fig-6] with majority of patients being males (91%) and average age 41.7 years. Commonest type of hernia was indirect (65.7%), while direct being in 26.9% of patients. Per-operatively mixed hernia (pantaloon hernia) was detected in 7.5% of the patients. Most of the cases were performed under regional anaesthesia - spinal or epidural (89.55%) and only 7 (10.45%) cases were administered general anaesthesia either due to patient’s wish, spinal deformity or failed regional anaesthesia.
The mean duration of surgery was significantly higher for PHS group (65.4 min), than LHR group (51.3 min), with range being 50-105 min and 42-90 min respectively. No intra-op complications were noted in either of the groups [Table/Fig-7].
The average pain score for PHS group was 3.2/10 and for LHR group 4.2/10 (p = 0.0735). Amongst these 41.18 % patients in LHR group felt moderate to severe pain (score 6-8) where as in PHS group only 15.15% patients had such pain, which is statistically significant (p = 0.018). Requirement of analgesia in PHS group was average 3.7 days and in LHR group it was 4.6 days, with p-value of 0.024 which again is significant.
In PHS group 53% patients were able to do their daily work comfortably after 2nd post-operative day with average time of 2.8 days, whereas in LHR group only 25% patients were able to perform their normal activity after 2nd post-operative day. Their average time to return to normal activity was 3.4, implying a statistically significant difference (p = 0.023). Average duration of hospital stay in PHS group was 3.5 days against average of 4.8 days in LHR group (p-value = 0.001).
Overall 5 patients in PHS group and 6 patients in LHR group suffered from early complications like seroma, hematoma, and wound infections. But the difference is not statistically significant [Table/Fig-8]. Inguinodynia (chronic inguinal pain) was noted in 1 patient of PHS group and in 2 patients of LHR group, but again the difference is not statistically significant. No recurrence was noted in any of the groups. The average time of follow-up for the study was 7.8 month, ranging from 1 to 18 months.
Discussion
Both Lichtenstein hernioplasty and repair using PHS bilayer device are tension-free techniques. But the major drawback with simple onlay repair like LHR is that it deals only with superior half of the myopectenial orifice (MPO), that too from the external aspect. Recurrences after LHR are known to occur near the pubic tubercle, through the internal ring or lateral to the mesh, even though overall recurrence rate has been minimized from the days of simple suture repairs to less than 1% [14] . A French study found that all 206 recurrences in their series were located at the MPO and that the choice of mesh must take this into account [15] . There is also evidence suggesting that development of an ipsilateral femoral hernia after inguinal mesh repair may be more common place than previously thought; a study has found a 15-fold incidence of femoral hernia repair after previous inguinal hernia surgery than in the general population [16] .
The PHS technique involving pre-peritoneal dissection is well tolerated and easy to carry out without any major intra-op or post-op complications, as has been brought out from this study. It provides a stable anterior repair with the added benefits of a posterior repair and a plug repair. The ‘underlay’ component secures the whole of MPO, the ‘onlay’ component secures the floor of the inguinal canal, virtually eliminating any chance of recurrence, and ‘connector’ additionally preventing the risk of mesh migration [5] . Moreover, placement of the underlay component in the pre-peritoneal plane has theoretical advantages. It employs Pascal's principle of hydrostatic pressure to allow intra-abdominal pressure to keep the mesh secure in place.
Currently, attempts to develop newer hernia techniques are also to improve the element of performing the procedure [17] , besides lowering the recurrence rate. Such improvement can be ease of operation and low early & late complications, especially chronic groin pain. The ultimate goal of these advances is the improved quality of life and satisfaction level of the patients undergoing hernia surgery. In the present study, we observed there is a statistically significant difference in post-operative pain & requirement of analgesia, and time to return to normal activity, in favor of PHS group, thus indicating the increased comfort level of the patient. In a previous study Kingsnorth et al., have showed immediate postoperative pain and return to normal activity and work were shorter with PHS group compared with the Lichtenstein group [7] . Though Nienhuijs et al., reported no significant difference in the postoperative pain between the two groups [8] .
Patients in PHS group had less number of early complications than LHR group (5 compared to 6), though the difference is not statistically significant. No specific intra-operative complication was noted. In particular, no difficulty was encountered in creating the pre-peritoneal space for deployment of underlay sheet of PHS. Sanjay et al., did report in their study removal of PHS device in one case due to hematoma [9] , and this is a potential complication in creating the pre-peritoneal space. But careful surgical dissection can avoid such a complication. Few other studies [8,12] have also reported no significant difference in complication rates between the two techniques. So, as far as safety is concerned or the hesitation to enter pre-peritoneal space, it can be safely done with minimal of learning curve. The length of the learning curve to comfortably perform the PHS technique ranged from one to six cases, with a mean of four cases [18] .
We observed no recurrence in either of the groups till the time of follow-up, and this reaffirms the excellent results of prosthetic repairs irrespective of method as far as recurrences are concerned. In a study by Awad et al., significantly lower recurrence rate was found with PHS group as compared to LHR group [11] , though in another study by Vironen et al., no significant difference was found [10] . In a study published by Gilbert et al., who designed the PHS, it has been shown that intermediate recurrence rates for PHS repair were similar in the hands of hernia specialists and general surgeons [18] . Chronic inguinodynia was observed in total 3 patients (overall incidence of 4.48%), out of which one patient was in PHS group as against two in LHR group, though difference is statistically not significant. Less number of sutures used to fix the mesh probably minimizes the chance of nerve entrapment which is cited as an important cause of chronic groin pain in hernia surgery [19] .
In contrast to other studies [7,10] our operative time was significantly more for PHS group (65.4 min) than LHR group (51.3 min), but then with experience the duration of surgery for PHS also decreased. The operative time in PHS group could be brought down from 105 min in the first case to less than 60 min by the last case. Also this average difference of 14 min did not cause any added complication. Hence, in this study, there is no significant difference in the early and medium term outcome between PHS and LHR. Apart from the longer operative time for PHS technique, other parameters are significantly favorable for PHS than LHR technique. The PHS theoretically provides all the advantages of a tension-free repair, including more patient comfort, rapid return to normal activity and lower recurrence rates.
The only limiting factor in widespread use of PHS device in a developing country like ours is its cost. It adds about 20-25% to the total cost of hernia surgery. But if we take in account various advantages of PHS as highlighted by this study, the added cost might be justified. Though we would like to mention that exact costbenefit analysis was not the objective of this study, and this might be its limitation.
Prolene Hernia System [6]
Holding PHS with sponge holding forceps

Pushing PHS in the pre-peritoneal space

Inlay layer in preperitoneal space

Connector in deep inguinal ring and onlay layer covering the floor of inguinal canal
Patient’s characteristics between the two groups
| Patient’s Characteristic | PHS | LHR | ‘p’ value |
|---|
| No. of Patients (n) | 33 | 34 | - |
| Age in years (average) | 42.0 yrs. | 41.5 yrs. | 0.895 |
| Male/Female | 29 (87.9%) | 32 (94.1%) | 0.427 |
| Female | 4 (12.1%) | 2 (5.9%) |
| Right indirect | 17 (52%) | 17 (50%) | 0.887 |
| Right direct | 1 (3%) | 3 (9%) |
| Right mix | 1 (3%) | 1 (3%) |
| Left indirect | 6 (18%) | 4 (12%) |
| Left direct | 7 (21%) | 7 (21%) |
| Left mix | 1 (3%) | 2 (6%) |
| Spinal/Epidural anaesthesia | 30 (90.91%) | 30 (88.24%) | 0.721 |
| General anaesthesia | 3 (9.09%) | 4 (11.76%) |
Comparison of outcome measures between the two groups
| Outcome Measure (average) | PHS | LHR | ‘p’ value |
|---|
| Duration of surgery (min.) | 65.4 (SD: 10.1) | 51.3 (SD: 8.5) | <0.0001 |
| Postop Pain Score | 3.2/10 (SD: 1.6) | 4.2/10 (SD: 2.2) | 0.0735 |
| 2-4 (Mild) | 28 (84.85%) | 20 (58.82%) | 0.018 |
| 6-8 (Mod. To Severe) | 5 (15.15%) | 14 (41.18%) |
| Requirement of analgesia (days) | 3.7 (SD: 1.2) | 4.6 (SD: 2.0) | 0.024 |
| Return to normal activity (days) | 2.8 (SD: 1.1) | 3.4(SD: 1.2) | 0.023 |
Complications among the two groups
| Complication | Group | Total | |
|---|
| PHS | LHR | ‘p’ value |
|---|
| 33 | 34 | 67 |
|---|
| Seroma | 3 | 4 | 7 | 1.0 |
| Hematoma | 1 | 1 | 2 | 1.0 |
| Wound Infections | 1 | 1 | 2 | 1.0 |
| Inguinodynia | 1 | 2 | 3 | 1.0 |
| Recurrence | 0 | 0 | 0 | - |
| Total | 6 | 8 | 14 | 0.765 |
Conclusion
Based on the present study, we can recommend that PHS is a safe and better alternative to the time honored Lichtenstein hernia repair with added advantage of strengthening the whole of myopectineal orifice, and virtually eliminating any risk of recurrence.
[1]. IL Lichtenstein, AG Shulman, PK Amid, MM Montllor, The tension free hernioplastyAm J Surg 1989 157(2):188-93. [Google Scholar]
[2]. AW Robbins, IM Rutkow, The mesh plug hernioplastySurg Clin North Am 1993 73:501-12. [Google Scholar]
[3]. LM Nyhus, The preperitoneal approach and prosthetic buttress repair for recurrent hernia: the evolution of techniqueAnn Surg 1988 208:733-37. [Google Scholar]
[4]. RD Kugel, The Kugel repair for groin hernias Surg Clin North Am 2003 83(5):1119-39. [Google Scholar]
[5]. AI Gilbert, A bilayer patch device for inguinal hernia repairHernia 1999 3:161-66. [Google Scholar]
[6]. Prolene Hernia System, Ethicon product [image on the Internet]. Ecomed Ltd. [cited Oct 2014]. Available from: http://ecomed.com.ua/files/content/image/prolene_logo.jpg [Google Scholar]
[7]. AN Kingsnorth, D Wright, CS Porter, G Robertson, Prolene Hernia System compared to Lichtenstein patch: a randomized double blind study of short term and medium term outcomes in primary inguinal hernia repairHernia 2002 6:113-19. [Google Scholar]
[8]. SW Nienhuijs, I Van Oort, ME Keemers-Gels, LJ Strobbe, C Rosman, Randomized clinical trial comparing Prolene Hernia System, mesh plug repair and Lichtenstein method for open inguinal hernia repairBr J Surg 2005 92(1):33-38. [Google Scholar]
[9]. P Sanjay, D Harris, P Jones, A Woodward, Randomized controlled trial comparing prolene hernia system and Lichtenstein method for inguinal hernia repairANZ J Surg 2006 76(7):548-52. [Google Scholar]
[10]. J Vironen, J Nieminen, A Eklund, P Paavolainen, Randomized clinical trial of Lichtenstein patch or Prolene Hernia System for inguinal hernia repairBr J Surg 2006 93(1):33-39. [Google Scholar]
[11]. SS Awad, S Yallampalli, AM Srour, CF Bellows, D Albo, DH Berger, Improved outcomes with the Prolene Hernia System mesh compared with the timehonored Lichtenstein onlay mesh repair for inguinal hernia repairAm J Surg 2007 193(6):697-701. [Google Scholar]
[12]. J Dalenbäck, C Andersson, B Anesten, S Björck, S Eklund, O Magnusson, Prolene Hernia System, Lichtenstein mesh and plug-and-patch for primary inguinal hernia repair: 3-year outcome of a prospective randomised controlled trial. The BOOP study: bi-layer and connector, on-lay, and on-lay with plug for inguinal hernia repairHernia 2009 13(2):121-29. [Google Scholar]
[13]. PK Amid, AG Shulman, IL Lichtenstein, Open “tension-free” repair of inguinal hernias: the Lichtenstein techniqueEur J Surg 1996 162(6):447-53. [Google Scholar]
[14]. PK Amid, Lichtenstein tension-free hernioplasty: its inception, evolution, and principlesHernia 2004 8(1):1-7. [Google Scholar]
[15]. Pélissier EP, Blum D, Elhaimeur A, Marre P, Damas JM, Groin hernias: features of recurrencesHernia 2000 4:89-93. [Google Scholar]
[16]. T Mikkelsen, M Bay-Nielsen, H Kehlet, Risk of femoral hernia after inguinal herniorrhaphyBr J Surg 2002 89(4):486-88. [Google Scholar]
[17]. PK Amid, Classification of biomaterials and their related complications in abdominal wall hernia surgeryHernia 1997 1:15-21. [Google Scholar]
[18]. AI Gilbert, J Young, MF Graham, LT Divilio, B Patel, Combined anterior and posterior inguinal hernia repair: intermediate recurrence rates with three groups of surgeonsHernia 2004 8(3):203-07. [Google Scholar]
[19]. S Nienhuijs, E Staal, L Strobbe, C Rosman, H Groenewoud, R Bleichrodt, Chronic pain after mesh repair of inguinal hernia: a systematic reviewAm J Surg 2007 194(3):394-400. [Google Scholar]