Multiple Amoebic Liver Abscess As Initial Manifestation in Hiv Sero-Positive Male
Subrata Chakrabarti1
1Post Graduate Trainee, Department of General Medicine, Ipgmer, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subrata Chakrabarti, Doctor’s Hostel, Ajc Bose Road, Kolkata-700020, India.
E-mail: subratachakrabarti2011@gmail.com
Amoebic liver abscess is the most frequent extra-intestinal manifestation of Entamoeba histolytica infection. Immunosuppression is known to predispose to amoebic liver abscess. Although amoebic liver abscess is seen more commonly in patients of Human-Immunodeficiency virus (HIV), first presentation of HIV sero-positive patient as multiple liver abscess is quite uncommon.The author reports an unusual case of multiple liver abscesses in an HIV seropositive patient. This middle aged male with history of multiple unprotected sexual encounters presented with spasmodic abdominal pain, fever, diarrhoea and weight loss along with generalised ill-health and painful liver enlargement. HIV-1 serology was found to be reactive. Imaging revealed an enlarged liver with multiple, irregular, hypoechoic foci characteristic of abscesses. Amoebic aetiology was later confirmed by percutaneous aspiration and microscopy. Administration of appropriate chemotherapeutics along with institution of antiretroviral therapy led to both clinical resolution as well as disappearance of lesions.
Entamoeba histolytica, Extra-intestinal manifestation, Trophozoites
Case Report
A 37-year-old non-smoker, non-alcoholic male, farmer by occupation, presented with history of spasmodic abdominal pain, low-grade fever, diarrhoea and significant weight loss for last 7 months. He had previous history of multiple unprotected sexual encounters with commercial sex workers. On physical examination, he appeared chronically ill, emaciated with multiple enlarged lymph nodes in both axilla and cervical region.Oral thrush was also noted. Abdominal examination revealed tender hepatomegaly with intercostal tenderness. Rest of the systemic examination was non-contributory.
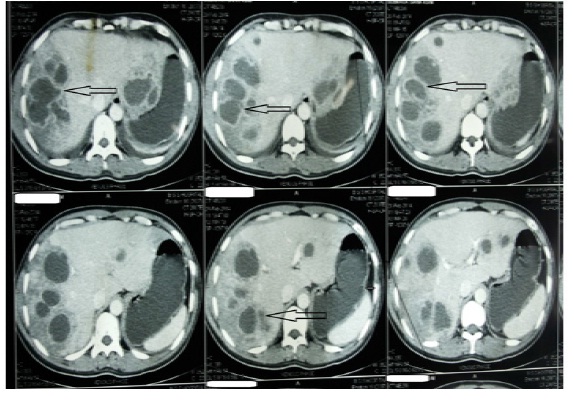
Complete blood count showed haemoglobin 8.6 g/dl with total WBC count 4100/cmm (Neutrophil-76%; lymphocyte-9%) and platelet 88000/cmm. Liver and renal function tests as well as serum electrolytes revealed normal results except hypo-albuminemia (2 g/dl; normal: 3.5-5 g/dl). He was found to be sero-positive for HIV-I. However, serology for hepatitis virus and HIV 2 was negative. CD4 cell count was 221 /cmm (normal: 500-1500/cmm). Abdominal ultrasound scan showed an enlarged liver with multiple, irregular, hypoechoic foci of varying size (largest one being 7.5 mmx6.5 mm) suggestive of multiple abscesses but normal biliary tracts and gall bladder. The most accessible abscess cavity was drained percutaneously under ultrasound guidance and the pus was sent for microscopy and culture-sensitivity tests. Simultaneously blood cultures (aerobic and anaerobic) were sent. The patient was empirically started on intravenous Ceftriaxone and Metronidazole. Contrast-enhanced CT scan of the abdomen confirmed the presence of multiple irregular hypo-dense lesions, varying in size with ring enhancement, predominantly in the right lobe of the liver suggestive of abscesses [Table/Fig-1]. Microscopy of the aspirate showed blood stained purulent material, clusters of hepatocytes, kupffer cells, polymorphs and degenerated cells. No malignant cell was seen. Trophozoites of Entamoeba histolytica in fluid were obtained from the abscess. The liver aspirate culture and sensitivity showed no bacterial growth after 7 days of incubation. Blood cultures were also negative for any growth. Indirect hemagglutination assay (IHA) for E. histolytica was positive (>1:128 titre). Stool microscopy showed numerous red blood cells but no trophozoites were isolated. The isolated organisms were sensitive to the already administered metronidazole. He responded to a two week course of intravenous antibiotics (metronidazole 750 mg). He was commenced on highly active antiretroviral therapy (HAART) comprising of Zidovudine, Stavudine and Nevirapine before discharge and also administered luminal amoebicides (Iodoquinol 650 mg for 20 days). He was discharged after 22 days of admission and a repeat abdominal USG at the time of discharge revealed a decrease both in the number of abscesses and size of the remaining ones.
Discussion
Amoebic liver abscess (ALA) develops in around 5% to 10% of patients who develop amoebic infestation of the gastrointestinal tract. It is more common in adults than children and is often associated with severe morbidity and mortality [1]. The clinical presentation of ALA is variable and unpredictable which may lead to delay in diagnosis. ALA usually presents as an acute illness, with right upper quadrant pain, fever, and tender hepatomegaly. A past history of dysentery is occasionally absent. Malnutrition, poor socioeconomic status, anaemia, diabetes mellitus or steroid overuse, chronic alcoholism are some known predisposing factors for the development of ALA. Naturally, conditions of immunosuppression (including HIV infection) should be a risk factor in its genesis [2].
ALA is usually solitary and pyogenic liver abscess is usually multiple [3]. Multiple ALA, although rare, are frequently confused with pyogenic liver abscess. However, Tayal et al., from India showed that existence of multiple ALA are not uncommon as previously thought and superinfection or co-infection with pyogenic organisms is common in such cases [4]. Gram negative rods (Escherichia coli and Klebsiella pneumoniae) are the most common organisms isolated from such abscesses [3]. Thus, presence of bacteria in multiple ALA does not always imply a primary pyogenic source and underlying amoebic aetiology must be excluded. These mixed abscesses are also larger in size. This distinction is important for management purposes as pyogenic abscesses almost always require some drainage procedure whereas amoebic abscesses even when multiple do not usually require therapeutic aspiration except in some special situations [2,3]. However, Soentjens et al., reported a case of a Belgian female with multiple ALA who did not respond to conservative treatment and showed clinical improvement only after percutaneous drainage of the largest abscess [5]. Also, care must be exercised during work-up of multiple liver abscesses as multiple ALA are known to often masquerade as pyogenic abscess.
Multiple ALA present with fever, toxaemia, deep jaundice, and encephalopathy. Toxaemia is often due to an added bacterial infection leading to a more severe disease. These patients present with a clinical picture indistinguishable from hepatic encephalopathy due to acute hepatocellular failure. Hepatic encephalopathy in ALA patients possibly results from combination of right hepatic vein occlusion, pyelophlebitis, and occlusion of several portal vein radicles [6].
Epidemiologically, ALA is commonly seen in young males in developing countries where the organism Entamoeba histolytica is endemic. A notable feature is its increased prevalence in individuals with depressed immunity, especially cell mediated immunity. This is biologically plausible as cell mediated killing is mainly responsible in eliminating amoebic infection and antibodies play limited role both in controlling acute infection and in preventing re-infection [1,3]. Not surprisingly a major fraction of the reported cases of ALA are seen in immunocompromised patients (including HIV sero-positives) and in persons exercising high risk behaviour specially Men having sex with men (MSM) [7]. Capote et al., from Spain reported a case of ALA in a sero-positive male [8]. However, an extensive review of the literature shows that the association of multiple liver abscess and HIV/AIDS is not very common. Few case reports are reported world-wide. Brindicci et al., described a case of a HIV-positive Italian patient who was hospitalized due to fever and recurring abdominal pain. Abdominal ultrasonography revealed six hepatic hypoechoic lesions suggestive of abscesses. Serum antibodies for E. histolytica were positive and E. histolytica was identified in drainage fluid with polymerase chain reaction (PCR). Therapy with metronidazole followed by paromomycin produced improvement, both symptomatically and radiographically [9].
Although, amoebic liver abscess is the most common extra-intestinal complication of amoebic infection, ALA in HIV-infected patients has not been well characterized. In a study conducted by Park et al., on amoebic liver abscess in Taiwan, the study group noted an increased prevalence of HIV seropositivity among the patients. Median age of the HIV-positive patients with liver abscess was 34.5 y and male sex outnumbered females [10]. The proportion of HIV-infected patients among patients with ALA increased significantly with time. Clinical presentation of invasive amoebiasis in HIV seropositive persons is similar to that in the normal host. High fever, leukocytosis and high C Reactive Protein (CRP) are associated with extra-luminal amoebic diseases in both HIV seropositive and seronegative patients. The outcome of metronidazole as well as tinidazole treatment of uncomplicated amoebiasisis favourable in HIV-1- infected individuals and comparable to that in immunocompetent persons [11]. However, it should be noted that luminal treatment following metronidazole or tinidazole treatment does not eliminate the possibility of recurrence of amoebiasis in high risk populations probably due to the risk of re-infection [12]. HIV-infected MSM are at especially higher risk of amoebiasis than patients from other risk groups [13]. However, according to a study by Wiwanitkit in Thailand, Gram-negative aerobes and not Entamoeba histolytica were the major common pathogens causing liver abscess in HIV seropositive patients. Among Gram-negative aerobes, Klebsiella pneumoniae was the most significant microorganism, followed by Escherichia coli and Pseudomonas aeruginosa [14].
Although, Jessurun et al., found no association between HIV and ALA [15], suppressed cellular immunity caused by use of steroids and malnourishment is an established risk factor to predispose to fatal amoebiasis and it can be safely considered that HIV seropositive patients with low CD4 cunts are vulnerable to develop amoebic liver abscesses.
Showing multiple hypodense lesions, with varying size and ring enhancement in the liver suggestive of abscesses in Contrast-enhanced CT scan of the abdomen
Conclusion
This case report highlights the fact that HIV sero-positivity status must be excluded during work-up of amoebic liver abscess. All patients with amoebic liver abscess, particularly if multiple abscesses are present, should be screened for immuno-suppression especially HIV even in absence of established risk factors for HIV.
[1]. MA Hughe, WA Petri, Amebic liver abscessInfect Dis Clin North Am 2000 14:565-82. [Google Scholar]
[2]. JM Salles, LA Morales, MC Salles, Hepatic amebiasisBraz J Infect Dis 2003 7(2):96-110. [Google Scholar]
[3]. JE Kurland, OS Brann, Pyogenic and amebic liver abscessesCurr Gastroenterol Rep 2004 6(4):273-79. [Google Scholar]
[4]. A Tayal, P Lal, B Uppal, Single and multiple liver abscesses in adults in Delhi are amoebic in origin: a clinical and microbiological studyTrop Doct 2013 43(2):77-79. [Google Scholar]
[5]. P Soentjens, B Ostyn, J Clerinx, A van Gompel, R Colebunders, A case of multiple liver abscesses: clinical improvement after percutaneous aspirationActa Clinica Belgica 2005 60(1):28-32. [Google Scholar]
[6]. OP Kapoor, R Joshi, Multiple amoebic liver abscess. A study of 56 casesJ Trop Med Hyg 1992 75(1):4-6. [Google Scholar]
[7]. CJ Liu, CC Hung, MY Chen, YP Lai, PJ Chen, SH Huang, Amebic liver abscess and human immunodeficiency virus infection: a report of three casesJ Clin Gastroenterol 2001 33:64-68. [Google Scholar]
[8]. RM Capote, DP Ramírez, JF Tirado, Liver abscess and HIV: report of a caseRev Cubana Med Trop 2003 55(1):47-49. [Google Scholar]
[9]. G Brindicci, C Picciarelli, L Fumarola, S Carbonara, F Stano, E Ciracì, Amoebic hepatic abscesses in an HIV-positive patientAIDS Patient Care STDS. 2006 20(1):606-11. [Google Scholar]
[10]. WB Park, PG Choe, JH Jo, SH Kim, JH Bang, Amebic liver abscess in HIV-infected patients, Republic of KoreaEmerg Infect Dis 2007 13:516-17. [Google Scholar]
[11]. K Watanabe, H Gatanaga, A Escueta-de Cadiz, J Tanuma, T Nozaki, S Oka, Amebiasis in HIV-1-infected Japanese men: clinical features and response to therapyPLoSNegl Trop Dis 2011 5:e1318 [Google Scholar]
[12]. CC Hung, PJ Chen, SM Hsieh, JM Wong, CT Fang, SC Chang, Invasive amoebiasis: an emerging parasitic disease in patients infected with HIV in an area endemic for amoebic infectionAIDS 1999 13:2421-28. [Google Scholar]
[13]. MD Oh, K Lee, E Lee, S Kim, N Kim, H Choi, Amoebic liver abscess in HIVinfected patientsAIDS 2000 14:1872-73. [Google Scholar]
[14]. V Wiwanitkit, Causative agents of liver abscess in HIV-seropositive patients a 10 year case series in Thai hospitalized patientsTropical Doctor 2005 35(2):112-15. [Google Scholar]
[15]. J Jessurun, LP Barron-Rodriguez, G Fernandez-Tinoco, M Hernandez-Avila, The prevalence of invasive amebiasis is not increased in patients with AIDSAIDS 1992 6:307-09. [Google Scholar]