Introduction
Though measles is a vaccine preventable disease, outbreaks still continue to occur because of poor immunization coverage rate at the national level.
Objective
To report the survey results of an outbreak of measles in Puraini village of Madhepura district in Bihar, India.
Materials and Methods
This cross-sectional survey was conducted among children aged 6 months to 12 years during an outbreak of measles in December 2008. WHO case definition criteria was used to define active measles cases. Demographic data, immunization status, and disease outcome among the cases was obtained by pre-structured questionnaires. Blood samples from 5 cases were sent for laboratory confirmation.
Results
A total of 52 cases and 8 deaths were reported with an attack rate of 28% and case fatality rate of 15.4%. Out of 35% cases of post-measles complications, dysentery with pneumonia was the most common. Anti-measles IgM antibody tested positive in all the 5 serum samples sent for confirmation. No child had received measles vaccination in the past, and the reasons were lack of awareness, lack of faith on vaccination, and unavailability of health workers.
Conclusion
This survey calls for strengthening of disease surveillance and routine immunization coverage to achieve measles control in these communities. This has important public health implication for the whole country regarding measles elimination in near-future.
Case fatality rate, Immunization, Morbillivirus, Secondary attack rate, Vitamin A
Introduction
Measles is one of the leading causes of childhood morbidity and mortality in the world despite the availability of a safe, effective, and relatively inexpensive vaccine [1,2]. The incidence varies from 10 to 15%, with a marked increase in the incidence (>50%) during an outbreak [3,4]. Malnutrition, poverty, overcrowding, poor hygiene, vitamin A deficiency, improper immunization and decreased immunity are the factors associated with an increased risk of the disease [5]. Studies from the rural, semi-urban, slum, and community settings has shown poor immunization coverage rate leaving some high risk pockets of population in which outbreak occurs [6,7].
A measles outbreak was reported among children of Mushar community of Puraini village in the Madhepura district of Bihar in December 2008. Immediately after the report, the district medical team and central team (including ours) visited the area and reviewed the situation. The same area had reported three measles outbreaks during the months of October to December 2007. NFHS-3 (National Family Health Survey-3) data published in the year 2005-2006 shows, the immunization coverage of the whole district to be of 33% (measles vaccine = 40%, and vitamin A = 29.4%) [8]. Only a few children probably had received the measles immunization during the catch-up round after the outbreaks in the year 2007. Therefore, this survey was carried out to investigate the extent of problem, to study the underlying factors responsible for its occurrence, to institute immediate control measures, and to prevent future outbreaks.
Objective
To report the survey results of an outbreak of measles in Puraini village of Madhepura district in Bihar, India.
Materials and Methods
The study area consisted of about 50 families with a population of nearly 375. Most of the inhabitants are from Musahar Community who are underprivileged group belonging to the lowest socio economic strata with a high fertility rate and illiteracy with a very low immunization coverage rate. These inhabitants resided in the village Chandi ashtan Musahari tola situated in Puraini block on Madhepura – Purnea Border {about 8 km from block primary health centre (PHC), 2 km from the nearest sub-centre, and about 60 km from the district headquarter}.
Since the district was under disease surveillance reporting system, in December 2008, block medical officers reported cluster of measles cases in the affected area. A cross-sectional survey was conducted by our team from 28th to 31st December 2008 among the children aged 6 months to 12 years. The World Health Organization (WHO) case definition “fever and maculopapular rash with any one of cough, coryza or conjunctivitis” was used for active search of cases [9]. House to house visits and enquiries about measles cases were made from the mothers or any responsible person of the family. Data was collected through structured questionnaires in an interview mode [9]. Information on demographic details, date of onset of rash, immunization status, and reasons for non-vaccination and disease outcome among cases was obtained. To serologically confirm the outbreak, blood samples from 5 suspected cases were collected and sent for laboratory confirmation for presence of anti-measles specific IgM antibodies. Consent from parents was taken for blood sample collection. The outbreak was described in terms of time, place and person. Simple statistical tools such as proportion, and percentage were used to report the data.
Results
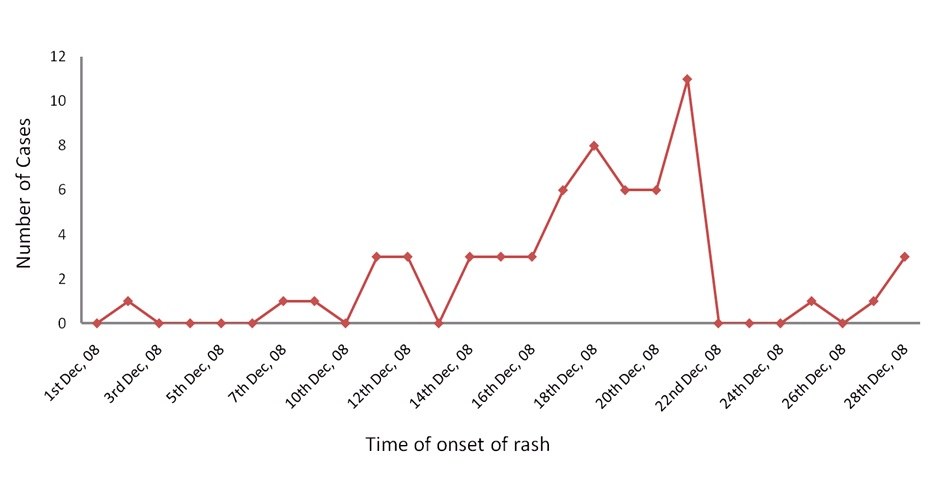
Musahar community of Puraini village was an underprivileged illiterate nomadic group belonging to lowest socio-economic strata with high fertility rate. The community population was about 375. Total child population aged between 6 months to 12 years in the community was 185. The index case was recorded on 1st December 2008, but was reported to district health authorities on 27th December 2008. Cases peaked on 21st December 2008, and all of them were reported within a radius of 40 meters only. [Table/Fig-1] shows the measles cases by date of onset of rash in form of epidemic curve.
The attack rate (AR) by age and sex has been described in [Table/Fig-2]. With a total of 52 cases with 8 deaths, the attack rate (AR) was 28% and the case fatality rate (CFR) was 15.4%. Eighteen (35%) cases reported post-measles complications (diarrhoea = 10, pneumonia = 5, and otitis media =3). Eight children died due to post-measles complications (diarrhoea and pneumonia). The detection of anti-measles specific IgM antibodies in blood samples of 5 suspected cases confirmed the diagnosis through IgM capture ELISA test. It was also observed that none of the children had any immunization card and none were given any immunization. Hence the routine immunization system did not exist in the community. Therefore, it was considered that children belonging to Musahar community had no vaccination history including measles vaccination and vitamin A supplementation, leading to frequent outbreaks. [Table/Fig-3] shows responses of Musahar community for the reason of non-immunization of their children.
Discussion
The present study revealed the overall attack rate (AR) of measles to be around 28%. It was somewhat higher than that reported in most of the published studies from India [3,5,10-20], baring a few [4,21]. So, the possible reason could be because of an increase rate in the immunization in recent years leading to a decrease in the susceptible population.
The case fatality rate (CFR) in the present survey was around 15%. A study conducted in tribal hamlet of Thane district, Maharashtra reported a similar CFR of around 15% [21]. Various community based studies have estimated CFR in developing countries as 3 to 15% [3-5,10-21]. The CFR may increase up to 10 to 30% in situations like ‘outbreaks’. The three major causes of death in measles are pneumonia, diarrhoea and croup [9]. Similar finding was reported in our study, where 8 deaths had occurred due to diarrhoea and pneumonia. It was also observed that children in the age group of 10-12 months and 25-60 months had experienced a higher AR of 45% and 49% respectively. Studies carried out in developing countries have revealed a high AR among children <12 months of age [3-5.10-21]. This may be due to measles being more severe in malnourished children particularly those with vitamin A deficiency [3-5,14-16].
Majority of the cases (85%) had occurred among children <5 years of age compared to 15% children >5 years of age. Similar finding was reported from the study conducted in the tribal hamlet of Thane district of Maharashtra, where AR in the above respective age groups was 50% and 57% respectively, and 96% of the cases were <6 years of age [21]. A higher proportion of girls were affected in the present study as compared to the boys, similar to that reported in a study from West Bengal and Chandigarh [17,19]. Studies from India have reported measles cases in higher proportion either among the boys or with no gender difference [3-5,10-21]. The reason may be due to the differential attitude of parents towards the girl child, especially among lower strata and economically disadvantage communities.
Madhepura district had reported the occurrence of three outbreaks within a span of less than 2 years (from 2007 to 2008) in the same season and same population. During the period of 2008-2012, Bihar state has alone reported a high number (n = 97) of measles outbreaks [22]. This also correlates with some of the rural epidemics described earlier from India and Bangladesh [21,23,24]. These communities are migratory in nature and are coming from neighbouring states having poor health indicators which add to the pool of susceptible children. Lack of hygiene, lower immunization coverage, overcrowding and high illiteracy in the underprivileged population increases the risk of measles transmission. Thus it is presumed that the migrating population might have appeared to import measles which flared up resulting in an outbreak among the susceptible. Prior immunization of the children of remote isolated populations may prevent such outbreaks [25]. Spread of measles from urban to rural areas has been described earlier from India and Africa [26].
Our survey reveals that none of the children had any immunization card nor given any immunization when enquired from the mothers/families. Hence the routine immunization system did not exist in the community. The immunization coverage of this community was considered nil. Therefore, reasons for not vaccinating the children were enquiredfrom the mother/family. It was found that majority had no faith in vaccination (42.2%) followed by lack of awareness for vaccination (28%), unavailability of health workers (19.6%) and fear of adverse reactions (9.8%). Similar findings have been reported previously from the districts of Purulia in West Bengal and Surat in Gujarat [3]. [Table/Fig-4] shows characteristics of studies which have reported measles outbreaks in the last twenty years from India.
Though the findings of the present survey are important, and provide direction for regulatory measures to be undertaken for control or elimination measles in high risk areas, there are few limitations that need to be mentioned. First, the survey was conducted few years back, and the same scenario might not exist presently. Second, a cause-effect relationship was not established with various risk factors, though the study design was not suitable for the same.
Time of onset of measles by onset of rash during the study period
Rate (AR) of measles by age and sex in Madhepura district, Bihar
| | Cases | Population | AR (%) |
|---|
| Age (months) | 6-9 | 2 | 6 | 33 |
| 10-12 | 15 | 33 | 45 |
| 13-24 | 4 | 28 | 14 |
| 25-60 | 23 | 47 | 49 |
| 61-144 | 8 | 71 | 11 |
| Sex | Male | 22 | 112 | 19.6 |
| Female | 30 | 73 | 41 |
| Overall | | 52 | 185 | 28 |
Reason for non-vaccination among Musahar Community (N=102)
| Reasons for non-vaccination | No of people | Percentage (%) |
|---|
| Lack of awareness | 29 | 28 |
| Fear of adverse reactions | 10 | 9.8 |
| Unavailability of Health workers | 20 | 19.6 |
| Lack of faith in vaccination | 43 | 42.2 |
Shows characteristics of studies which have reported measles outbreaks in the last twenty years from India
| Study ID [Ref] | Geographical region, Sample size (N) | Design; study period | Parameters studied | Results |
|---|
| Risbud et al., 1994 [21] | Thane district of Maharashtra; N= 176 | Cross-sectional study; March 1992 | Most common age group affected, attack rate (AR), case fatality rate (CFR), post-measles complication | Most common age group affected was <6 years (no sex difference), AR = 51.4% to 52.7%, CFR = 15.6% to 31.2%, post-measles complication in 60%. |
| Singh et al., 1999 [14] | Whole of Uttar Pradesh; N= 6922 | Cross-sectional study; 1991 to 1996 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was <5 years (higher number of boys, but increased mortality in girls), AR = 6.7%, CFR = 4.1%, immunization rate 26% (year 1991) to 36% (year 1996). |
| Bharti et al., 2002 [4] | Village Astani in Himachal Pradesh; N=48 | Questionnaire based; 27th July 1997 | Symptoms, and post-measles complications, immunization rate | Children studied were <12 years, AR = 58%, CFR = 2.1%, post-measles complication in 59%, immunization rate 33%. |
| Thakur et al., 2002 [11] | Periurban areas of UT, Chandigarh; N= 283 | Cross-sectional study; December 1998 to February 1999 | Attack rate (AR), case fatality rate (CFR), post-measles complication, immunization rate | Children studied were <12 years (higher proportion among boys), AR = 4.5%, CFR = 0, post-measles complication in 31%, immunization rate 51%. |
| Sharma et al., 2004 [5] | Slums of UT, Chandigarh; N= 1130 | Cross-sectional study; April 22 to May 10, 2003. | Most common age group affected, attack rate (AR), case fatality rate (CFR), post-measles complication, immunization rate | Most common age group affected was <5 years, AR = 5.13%, CFR = 0, post-measles complication in 20%, immunization rate 33%. |
| Ray et al., 2004 [12] | Slum areas of Kolkata; N= 290 | Cross-sectional study; 25th March to 5th April 2000 | Attack rate (AR), case fatality rate (CFR), post-measles complication, immunization rate | Children studied were <5 years (no sex difference), AR = 5.76%, CFR = 0, post-measles complication in 50%, immunization rate 19.7%. |
| Ratho et al., 2005 [15] | Panchkula district of Haryana; N= 12 | Cross-sectional study; late September to mid October 2003. | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was <5 years (higher number of boys, but increased mortality in girls), AR = 7.7%, CFR = 16.7%, immunization rate 2.5%. |
| Kumar et al., 2008 [13] | Urban slums of inter-state border districts of West Bengal; N= 290 | Cross-sectional study; 2005 to 2006 | Attack rate (AR), case fatality rate (CFR), post-measles complication, immunization rate | Children studied were <5 years (no sex difference), AR = 4.8%, CFR = 0, post-measles complication in 50%, immunization rate 20%. |
| Mishra et al., 2009 [3] | Shivpuri district of Madhya Pradesh; N= 1204 | Cross-sectional study; 12-19 May 2004 | Common age group affected, attack rate (AR), case fatality rate (CFR), post-measles complication, immunization rate | Common age group affected was <5 years (higher proportion among boys or no gender difference), AR = 6.2%, CFR = 1.2%, post-measles complication in 17.7%, immunization rate <30%. |
| Gupta et al., 2009 [20] | Kangra district of Himachal Pradesh; N= 69 | Cross-sectional study (two outbreaks reported); 3rd September to 23rd November 2006 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was 11-17 years (no sex difference), AR = 4.2% to 6%, CFR = 0, immunization rate 69% to 78%. |
| Mishra et al., 2012 [18] | Bhavnagar District, Gujarat; N= 105 | Cross-sectional study (two outbreaks reported); December 2010 to April 2011 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was 5-9 years (no sex difference), AR = 2.7% to 4.4%, CFR = 0, immunization rate 38%. |
| Patro et al., 2012 [19] | Urban resettlement colony of Chandigarh; N= 14 | Cross-sectional study; 22 November 2010 | Most common age group affected, case fatality rate (CFR), immunization rate | Most common age group affected was >5 years (girls commonly affected), CFR = 0, immunization rate 100%. |
| Bhuniya et al., 2013 [17] | Jalpaiguri district of West Bengal; N= 113 | Cross-sectional study; April to June 2011 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was <5 years (girls commonly affected), AR = 14.3%, CFR = 0, immunization rate 16%. |
| Murhekar et al., 2014 [16] | Various districts of Bihar; N= 3988 | Cross-sectional study; 1 October 2011 to 30 April 2012 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was ≥5 years, AR = 7.3%, CFR = 0.78%, immunization rate 27%. |
| Present study | Madhepura district Bihar; N= 185 | Cross-sectional study; 1 December 2008 to 28 December 2008 | Most common age group affected, attack rate (AR), case fatality rate (CFR), immunization rate | Most common age group affected was <5 years, AR = 28%, CFR = 15.4%, immunization rate 0%. |
Conclusion
This study reveals that the measles outbreak occurred among the children of Musahar community because of lack of immunization. The outbreak was reported long time after the index case in the area, thus reflecting inefficient surveillance that failed to generate early warning signals. This study calls for strengthening of delivering health care services (routine immunization, surveillance system and awareness).
Acknowledgement
We extend with gratitude our sincere thanks with profound grief to Late Dr J A Khan, Ex-Deputy Director, NCDC, Delhi who guided and supervised us throughout the outbreak investigation and had encouraged to write for publication, and Dr. B.N.Singh, Civil Surgeon, District Hospital, Madhepura and his team for their immense support & help.
[1]. World Health Organisation. Progress in reducing global measles deaths: 1999-20022004 Weekly Epidemiological Record 1977 79:20-21. [Google Scholar]
[2]. K Park, The Textbook of Preventive and Social Medicine 2007 19th EditionJabalpurBanarsidas Bhanot Publishers:124-27. [Google Scholar]
[3]. A Mishra, S Mishra, C Lahariya, P Jain, RS Bhadoriya, D Shrivastava, Practical Observations from an Epidemiological Investigation of a Measles Outbreak in a District of IndiaIndian Journal of Community Medicine 2009 34:117-21. [Google Scholar]
[4]. B Bharti, S Bharti, Measles in a hilly Hamlet of Northern IndiaIndian Journal of Pediatrics 2002 69:1033-35. [Google Scholar]
[5]. MK Sharma, V Bhatia, HM Swami, Outbreak of measles amongst vaccinated children in a slum of ChandigarhIndian Journal of Medical Sciences 2004 58:47-53. [Google Scholar]
[6]. V Bhatia, HM Swami, SR Rai, S Gulati, A Verma, A Parasher, Immunization status in childrenIndian Pediatrics 2004 71:313-15. [Google Scholar]
[7]. A Puri, VK Gupta, A Chakravarti, M Mehra, Measles vaccine efficacy evaluated by case reference techniqueIndian Pediatrics 2002 39:556-60. [Google Scholar]
[8]. Indicators for Bihar, 2005-06, India. http://www.rchiips.org/nfhs/nfhs3.shtml [Accessed on 20th August 2014] [Google Scholar]
[9]. Manual for investigation and control of outbreak of Measles. Director General of Health Services, Govt. of India, National Institute of Communicable Diseases, Delhi’s 2006 http://www.ncdc.gov.in/ [Accessed on 25th December 2008] [Google Scholar]
[10]. A Mishra, S Mishra, P Jain, RS Bhadoriya, R Mishra, C Lahariya, Measles related complications and the role of Vitamin A supplementationIndian Journal of Pediatrics 2008 75:887-90. [Google Scholar]
[11]. JS Thakur, RK Ratho, SP Bhatia, R Grover, M Issaivanan, B Ahmed, Measles outbreak in a Periurban area of Chandigarh: need for improving vaccine coverage and strengthening surveillance Indian Journal of Pediatrics 2002 69:33-37. [Google Scholar]
[12]. SK Ray, S Mallik, AK Munsi, SP Mitra, B Baur, S Kumar, Epidemiological study of measles in slum areas of KolkataIndian Journal of Pediatrics 2004 71:583-86. [Google Scholar]
[13]. RS Kumar, M Sarmila, MS Prasad, M Pankaj, K Satish, An epidemiological study on incidence, symptoms and complications of measles in bordering districts of West Bengal The Journal of Communicable Diseases 2008 40:59-64. [Google Scholar]
[14]. J Singh, A Kumar, RN Rai, S Khare, DC Jain, R Bhatia, Widespread outbreaks of measles in rural Uttar Pradesh, India, 1996: high risk areas and groupsIndian Pediatrics 1999 36:249-56. [Google Scholar]
[15]. RK Ratho, B Mishra, T Singh, P Rao, R Kumar, Measles outbreak in a migrant populationIndian Journal of Pediatrics 2005 72:893-94. [Google Scholar]
[16]. MV Murhekar, M Ahmad, H Shukla, K Abhishek, RT Perry, AS Bose, Measles case fatality rate in Bihar, India, 2011-12PLoS One 2014 9(1):e96668 [Google Scholar]
[17]. S Bhuniya, D Maji, D Mandal, N Mondal, Measles outbreak among the Dukpa tribe of Buxa hills in West Bengal, India: epidemiology and vaccine efficacyIndian Journal of Public Health 2013 57:272-75. [Google Scholar]
[18]. PP Mishra, NT Chauhan, Double outbreak of measles in the talaja block of bhavnagar district, gujarat, India 2011: a need for improving the vaccine coverage and the community participationJournal of Clinical & Diagnostic Research 2012 6:1713-17. [Google Scholar]
[19]. BK Patro, HD Shewade, S Kathirvel, SS Senjam, MP Singh, RK Ratho, Outbreak of "modified measles" in an urban resettlement colony of North IndiaIndian Journal of Public Health 2012 56:168-69. [Google Scholar]
[20]. SN Gupta, N Gupta, Two Highly Immunized Hilly Areas versus Double Measles Outbreak Investigations in District Kangra, Himachal Pradesh, India, in 2006Journal of Global Infectious Diseases 2009 1:14-20. [Google Scholar]
[21]. AR Risbud, SR Prasad, SM Mehendale, Measles outbreak in a tribal population of Thane district, MaharashtraIndian Pediatrics 1994 31:543-51. [Google Scholar]
[22]. NCDC Quarterly Newsletter: Outbreak Update. Volume 2, Issue 3, July- September 2013 [Accessed on 15th September 2014] [Google Scholar]
[23]. CD Mitchell, HH Balfour, Measles control: so near and yet so farProg Med Virol 1985 31:1-42. [Google Scholar]
[24]. V Fauveau, J Chakraborty, RO Sarder, AM Khan, MA Koenig, Measles among under-9-months-olds in rural Bangladesh: its significance for age at immunizationBulletin of the World Health Organization 1991 69:67-72. [Google Scholar]
[25]. VK Desai, SJ Kapadia, P Kumar, S Nirupam, Impact assessment of mass measles vaccinationIndian Journal of Pediatrics 2002 69:1037-40. [Google Scholar]
[26]. WHO UNICEF. Measles mortality reduction and regional elimination: Strategic plan. 2001-2005. WHO/VandB/01.2003. [Google Scholar]