Retinal Hemorrhages in Severe Non-cerebral Plasmodium vivax Malaria in an Adult
Manoj Lakhotia1, Jagdish Singh2, Hans Raj Pahadiya3, Harish Kumar4, Prakash K. Choudhary5
1 Senior Professor, Department of Medicine, Dr. SNMCJodhpur, Rajasthan, India.
2 Senior Resident, Department of Medicine, Dr. SNMCJodhpur, Rajasthan, India.
3 Senior Resident, Department of Medicine, Dr. SNMCJodhpur, Rajasthan, India.
4 Senior Resident, Department of Medicine, Dr. SNMCJodhpur, Rajasthan, India.
5 Resident, Department of Medicine, Dr. SNMCJodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jagdish Singh, Room No. 15, PG Hostel, Olympic Circle, MG Hospital, Jodhpur, Rajasthan-342001, India.
E-mail: kaswan.mbbs@gmail.com
Malaria is the most important parasitic diseases of humans and one of the leading causes of morbidity and mortality in tropical countries. Earlier Plasmodium vivax was considered as a benign infection, but now it is recognized as a cause of severe malarial disease. It causes severe malarial disease similar to those as Plasmodium falciparum including cerebral malaria, severe anaemia, severe thrombocytopenia, hepatic dysfunction, shock, acute respiratory distress syndrome (ARDS), acute renal failure, and pulmonary oedema. Malarial retinopathy includes retinal whitening, vessel changes, retinal hemorrhages and papilledema. However, retinal hemorrhages are very rare in Plasmodium vivax infestation. Hereby, we report a case of 30-year-old man, who presented with fever with chills and diminution of vision. He was found to have Plasmodium vivax infection with retinal hemorrhages. He was treated successfully with artisunate, primaquine and doxycycline, completely recovered after one month.
Adult, Non-cerebral malaria, Retinopathy
Case Report
A 30-year-male admitted with seven days history of intermittent fever with chills. He had history of Plasmodium vivax malaria two months back and incompletely treated with chloroquine. Patient was not suffering from any chronic illness and had no addiction. He had no history of seizures or altered sensorium. On examination his temperature was 38.5°C by axilla. The blood pressure was 120/80 mmHg, pulse rate 110 beats/min, regular and respiratory rate was 18 breaths/min. He had severe pallor, icterus, conjuctival hemorrhage and splenomegaly. Signs of meningeal irritation were absent. Cardiovascular and respiratory system revealed no significant abnormality.
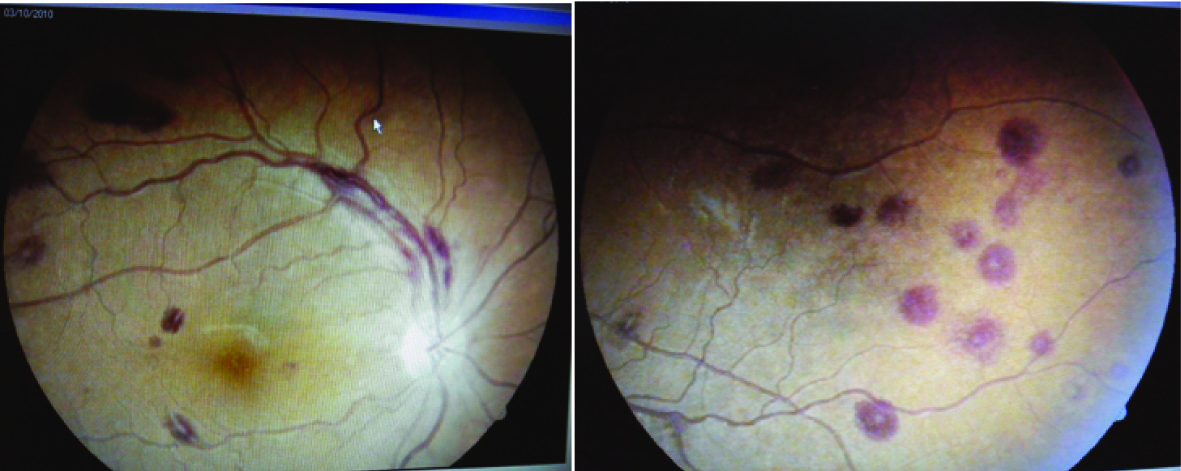
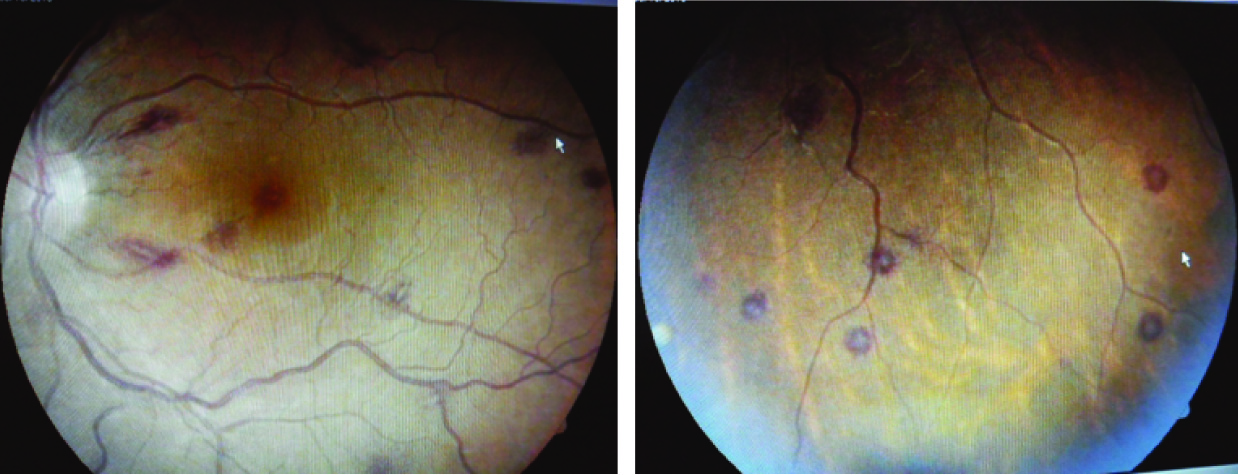
Two days after admission in the hospital he had history of sudden painless decrease in the vision from both eyes. His visual acuity in left eye was 6/9 and 9/12 in right eye. External ocular muscle movements were normal. Both pupils were round, equal, regular and reacting to direct and consensual light stimulus. Fundus examination revealed multiple retinal hemorrhages with white center and roth spots in all quadrants of fundus of both eyes. Retinal vessels were found tortuous. Papilledema, retinal whitening and exudates were absent [Table/Fig-1,2].
Laboratory investigations are mentioned in [Table/Fig-3]. Hemogram on the day of admission revealed anaemia and thrombocytopenia. The peripheral blood film showed trophozoite ring of Plasmodium vivax. RBCs were normocytic normochromic with polychromasia and platelets were reduced. The antigen testing including parasite lactate dehydrogenase (LDH) tested positive for Plasmodium vivax and negative for Plasmodium falciparum. Confirmation of Plasmodium vivax and exclusion of Plasmodium falciparum was done by PCR. NS1 antigen and IgM antibodies were negative for dengue virus. The Chest X-ray and ECG were normal. Ultrasonography of abdomen showed mild hepatosplenomegaly. CT scan of head was done which had no significant abnormality. CSF examination and coagulation profile was normal. Urinanalysis was normal and blood culture was sterile. He was tested negative for HBsAg, Anti- HCV and HIV 1&2. In a case of Plasmodium vivax malaria these finding were suggestive of severe vivax disease. He treated with 120 mg Artisunate iv injections at 0, 12 and 24 h and then OD for seven days with 100 mg doxycycline orally for seven days. Two units of packed cell were transfused. After seven days CBC was repeated which revealed Hb 7.1gm/dl, total leukocyte count 7800/mm3 and platelet 128000/mm3. CRP was <6 mg/dL. He was discharged on primaquine 15 mg OD for 14 days. On follow up after 30 days, patient was asymptomatic with normal hematological parameters and normal vision. Retinal hemorrhages had absorbed completely.
Laboratory Investigations at the time of admission.
| Parameters | Values | Reference value |
|---|
| Hb | 3.6 g/dL | 13.3-16.2 g/dL |
| TLC | 9,240/mm3 | 3.54-9.06×103/mm3 |
| DLC | N- 64%, L- 33%, E- 3% | N-40-70%, L20-50%, E-0-6% |
| Platelets | 30,000/mm3 | 165-415×103/mm3 |
| Blood sugar | 110 mg/dL | 65-95 mg/dL |
| Blood urea | 90 mg/dL | 7-20 mg/dL |
| Serum creatinine | 1.5 mg/dL | 06-1.2 mg/dL |
| S. Bilirubin-Total | 2.54 mg/dL | 0.3-1.3 mg/dL |
| Direct | 0.52 mg/dL | 0.1-0.4 mg/dL |
| AST | 55 IU/L | 12-38 IU/L |
| ALT | 54 IU/L | 7-41 IU/L |
| Total protein | 6.7 g/dL | 6.7-8.6 g/dL |
| S. Albumin | 3.7 g/dL | 3.5-5.5 g/dL |
| S. LDH | 3886 IU/L | 115-221 IU/L |
| S. Iron | 140 μg/dL | 70-140 μg/dL |
| TIBC | 327 μg/dL | 250-406 μg/dL |
| % Saturation | 42.5.0%, | 16-35% |
| S. Sodium | 142 meq/L | 136-146 meq/L |
| S. Potassium | 4.5 meq/L | 3.5-5 meq/L |
| S. Phosphorus | 4.6 mg/dL | 2.5-5.5 mg/dL |
| S. Calcium | 8.8 mg/dL | 8.5-10.5 mg/dL |
| S. alkaline phosphatase | 125 IU/L | 44-147 IU/L |
| C-reactive protein | >6 mg/dL | (0-6 mg/dL) |
| BT | 1 min 30 sec | (normal up to 5 min) |
| CT | 3 min | (normal up to 8 min) |
| PT | PT 13 sec | (control 13) |
| APTT | 34.6 sec | ( control 32.2) min |
| CSF | Sugar 56 mg/dL, Protein 35 mg/dL, RBC 0 cell/ml, WBC 02 cells/μL | Sugar (40-60) mg/dL, Protein (20-40) mg/dL, RBC 0 cell/ml, WBC (0-5) cells/μL |
Hb-Hemoglobin, TLC-Total Leukocytes count, DLC-Differential Leukocytes count, N-Neutrophils, L-Lymphocytes, E-Eosinophils, MCV-Mean Corpuscular Volume, MCH- Mean Corpuscular Hemoglobin, AST-Aspartate aminotransferase, ALT-Alanine aminotransferase, LDH- Lectate Dehydrogenase, TIBC-Total Iron Binding Capacity, BT- bleeding time, CT- clotting time, PT- prothrombin time, APTT- activated prothrombin time, CSF- Cerebrospinal fliud.
Discussion
Chloroquine, resistance relapses and greater transmission potential of Plasmodium vivax at low parasite densities may be responsible for severe and fatal complication of vivax malaria [1].
Retinal hemorrhages are frequently observed in Plasmodium falciparum infection, particularly with cerebral malaria in children but uncommon in non-cerebral malaria [2]. Malarial retinopathy includes various retinal changes and retinal signs in patients suffering from malaria. It includes retinal whitening, vessel changes, retinal hemorrhages and papilloedema. Retinal hemorrhages are very rare in Plasmodium vivax infestation [3–5]. The visual defects are usually reversible with complete recovery after treatment but rarely may be irreversible [6].
Malarial retinopathy is predominantly found in patients suffering from Plasmodium falciparum infestation with cerebral malaria in children but it can also be found in other form of malaria. Malarial retinopathy has also been found in adults with severe malaria and rare in Plasmodium vivax infestation [7]. It is characterized by retinal whitening (macular or perimacular), vessel changes (white or orange), retinal hemorrhage (particularly with white centres) and papilledema. Among these four changes, retinal whitening and vessel changes are specific and diagnostic of severe malarial disease [8]. The incidence of retinal haemorrhages was found in 46% cases of cerebral malaria [9]. This incidence was around 60% in children with cerebral malaria and was lower in less severe malarial disease [2].
Lewallen et al., [10] observed that the sequestration of many de-hemoglobinized late stage parasitized erythrocytes via cyto-adherence in the retinal microvasculature is considered as a cause of characteristic white and orange appearances of retinal vessels in severe malaria. This pattern of de-hemoglobinization is consistent with the clinical findings. Beare et al., [11] explained retinal whitening because of loss of retinal transparency. Retinal whitening appears as discrete areas of pale discolouration of the retina due to capillary non-perfusion on fluorescein angiogram. Micro vascular occlusion due to sequestration of infected erythrocytes leads to reduced perfusion, hypoxia and oncotic cell swelling which is responsible for retinal whitening.
Plasmodium falciparum is responsible for most cases of severe malarial disease with retinal hemorrhages because of sequestration, cytoadherence and rosseting phenomenon [12]. In Plasmodium vivax malaria the mechanisms of development of retinal hemorrhage and severe diseases are not well defined. In vivo Plasmodium vivax infected RBCs are known to cause cytoadherence on human lining endothelial cells and placental tissue, though this phenomenon is lower than that with Plasmodium falciparum infected RBC [13]. Apart from these, accompanied thrombocytopenia and anaemia may be responsible for retinal hemorrhage as a confounding or even a sole cause. Retinal haemorrhage may be due to causes other than malaria in endemic areas where incidental asymptomatic parasitemia may be found [7].
Systemic inflammatory response is also increased in patient with severe Plasmodium vivax disease. There is increase in the C reactive protein, plasma tumor necrosis factor and interferon gamma levels [14].
Retinal hemorrhages in these patients usually absorbed spontaneously over the period of one to four weeks without retinal sequelae [9] and visual defect improved completely after successful treatment of malaria. Few cases have been reported with irreversible visual defects [7]. Our patient had peripheral parasitemia, severe anaemia, thrombocytopenia, hepatic dysfunction, mild renal dysfunction, raised CRP level and multiple retinal hemorrhages with white center. After successful treatment of malaria, he gained normal vision with normal visual acuity after one month. Thus we assume that severe vivax disease was responsible for retinal hemorrhages.
Conclusion
Characteristic features of Malarial retinopathy including number of retinal hemorrhages could be useful tool in the diagnosis of severe malaria, and these factors directly correlates with the severity and prognosis of malarial disease. Thus every patient of severe malaria should be checked for presence of retinal hemorrhages, even in adult patients with non-cerebral Plasmodium vivax disease and the patient who presented with unexplained retinal hemorrhage and fever should be evaluated for malaria.
Hb-Hemoglobin, TLC-Total Leukocytes count, DLC-Differential Leukocytes count, N-Neutrophils, L-Lymphocytes, E-Eosinophils, MCV-Mean Corpuscular Volume, MCH- Mean Corpuscular Hemoglobin, AST-Aspartate aminotransferase, ALT-Alanine aminotransferase, LDH- Lectate Dehydrogenase, TIBC-Total Iron Binding Capacity, BT- bleeding time, CT- clotting time, PT- prothrombin time, APTT- activated prothrombin time, CSF- Cerebrospinal fliud.
[1]. Kochar DK, Das A, Kochar SK, Severe Plasmodium vivax malaria: a report on serial cases from Bikaner in northwestern IndiaAm J Trop Med Hyg 2009 80:194-98. [Google Scholar]
[2]. Lewallen S, Bronzan RN, Beare NA, Harding SP, Molyneux ME, Taylor T.E, Using malarial retinopathy to improve the classification of children with cerebral malariaTrans R Soc Trop Med Hyg 2008 102:1089-109. [Google Scholar]
[3]. Choi HJ, Lee SY, Yang H, Bang JK, Retinal haemorrhage in vivax malariaTrans R Soc Trop Med Hyg 2004 98:387-89. [Google Scholar]
[4]. Lee JH, Chin HS, Chung MH, Moon YS, Case Report: Retinal hemorrhage in Plasmodium vivax malariaAm J Trop Med Hyg 2010 82:219-22. [Google Scholar]
[5]. Kochar A, Kalra P, Kochar S, Kochar SK, Kochar DK, Retinal haemorrhage: An unusual presentation of vivax malariaJ Vector Borne Dis 2013 50:321-22. [Google Scholar]
[6]. Runyan TE, Ostberg RC, An unusual macular lesion associated with malariaAnn Ophthalmol 1977 9:1521-25. [Google Scholar]
[7]. Maude RJ, Beare NA, Abu Sayeed A, Chang CC, Charunwatthana P, Faiz MA, The spectrum of retinopathy in adults with Plasmodium falciparum malariaTrans R Soc Trop Med Hyg 2009 103:665-71. [Google Scholar]
[8]. Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME, Malarial retinopathy: a newly established diagnostic sign in severe malariaAm J Trop Med Hyg 2006 75:790-97. [Google Scholar]
[9]. Beare NA, Southern C, Chalira C, Taylor TE, Molyneux ME, Harding SP, Prognostic significance and course of retinopathy in children with severe malariaArch Opthalmol 2004 122:1141-47. [Google Scholar]
[10]. Lewallen S, Whitten RO, Gardiner J, Hoar B, Lindley J, Lochhead J, Clinical-histopathological correlation of the abnormal retinal vessels in cerebral malariaArch Ophthalmol 2000 118:924-28. [Google Scholar]
[11]. Beare NA, Harding SP, Taylor TE, Lewallen S, Molyneux ME, Perfusion abnormalities in children with cerebral malaria and malarial retinopathyJ Infect Dis 2009 199:263-71. [Google Scholar]
[12]. Mackintosh CL, Beeson JG, Marsh K, Clinical features and pathogenesis of severe malariaTrends Parasitol 2004 20:597-603. [Google Scholar]
[13]. Lacerda MVG, Mourao MPG, Alexandre MAA, Understanding the clinical spectrum of complicated Plasmodium vivax malaria: a systematic review on the contributions of the Brazilian literatureMalar J 2012 11:12 [Google Scholar]
[14]. Andrade BB, Reis-Filho A, Souzu-Neto SM, Severe Plasmodium vivax malaria exhibits marked inflammatory imbalanceMalar J 2010 9:13 [Google Scholar]