Spontaneous Resolution of Non Traumatic Chronic Subdural Haematoma Despite Continued Antiplatelet Therapy: A Case Report
Ajeet Ramamani Tiwari1, Shradha Maheshwari2, Srikant Balasubramaniam3, Tyagi Devendra4, Hemantkumar Savant5
1 Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai Central, India.
2 Assistant Professor, Department of Neurosurgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai Central, India.
3 Assistant Professor, Department of Neurosurgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai Central, India.
4 Associate Professor, Department of Neurosurgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai Central, India.
5 Professor and Head of Department, Department of Neurosurgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai Central, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajeet Ramamani Tiwari, Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman, Nair Charitable Hospital, Mumbai Central-400008, India. E-mail : drajeetramantiwari@gmail.com
Spontaneous resolution of traumatic chronic subdural haematoma (CSDH) has been reported in literature. However, those with non traumatic CSDH are exceedingly rare and none reported with continued antiplatelet therapy where it itself is an aetiological agent for development of non traumatic CSDH. A 50-year-old male presented to us with a non haemorrhagic cerebellar infarct with a concomitant CSDH without history of any trauma. Patient’s PT/INR, Bleeding time and Clotting time were normal. Patient was started on antiplatelet therapy (Tablet Aspirin 150 mg OD) for the acute infarct. MR Brain at 1 month showed an increased size of CSDH. However patient denied surgical evacuation hence we continued conservative line of management, however we continued anti-platelet therapy with close neurological and coagulation profile monitoring that remained within normal range throughout the period of observation. CT at 5th month showed complete resolution of CSDH. Patient was on antiplatelet drugs throughout the period of observation. Our case argues about the role of antiplatelet therapy in patients with CSDH with contrary lesions requiring anticoagulation.
Anticoagulation, Haemorrhagic, Ischemic heart disease
Case Report
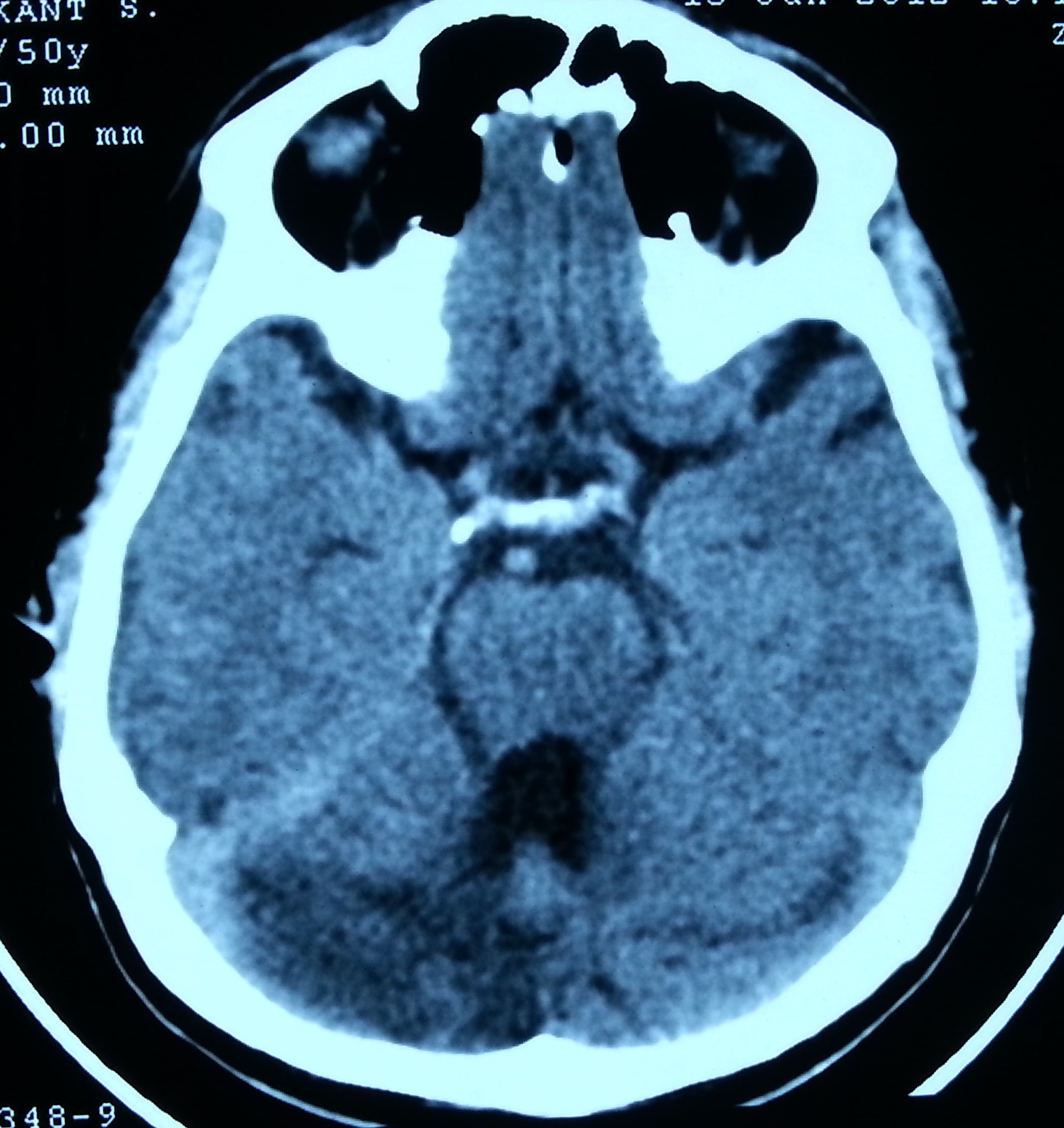
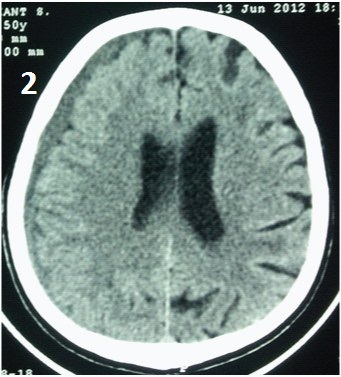
A 50-year-old male right handed known case of essential hypertension and ischemic heart disease presented to our Neurosurgery OPD with complains of slurring of speech and focal convulsions of tongue and face. There was no history of trauma, alcoholism or anti coagulants. We performed CT Brain that revealed two contrary lesions, an acute right cerebellar hemisphere non hemorrhagic infarct with CSDH of 6 mm width and mild effacement of right ventricle without any evidence of midline shift [Table/Fig-1,2]. Patient’s PT/INR, bleeding time and clotting time were within normal range. Patient was managed conservatively with anti-hypertensives and anti-platelet (Tablet Aspirin 150 mg OD) along with close neurological monitoring. Over a period of two weeks patient improved in slurring of speech with no fresh episode of convulsion.
CT Brain showing acute non haemorrhagic infarct of right cerebellar hemisphere
CT Brain showing CSDH of 6 mm width and mild effacement of right ventricle without any evidence of midline shift
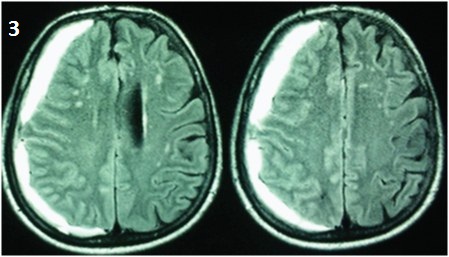
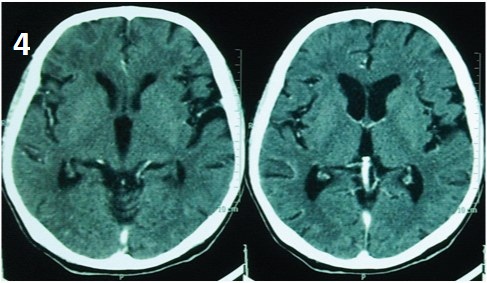
After a month patient complained of headache that was persistent with no relief on taking pain medications. MRI with MR Angiography was advised for further evaluation of stroke which revealed areas of altered signal intensity in right cerebellar hemisphere suggestive of old ischemic etiology and an increase in size of CSDH with midline shift of 4.1 mm towards left. MR Angiography was within normal limits [Table/Fig-3]. In view of increase in size of CSDH and persistent headache patient was advised surgical evacuation of CSDH but patient did not consent for the surgery and was hence conserved with close neurological and coagulation profile monitoring that remained normal throughout the period of observation. Anti-platelet therapy was continued in view of stroke complicated with ischemic heart disease. At subsequent follow up at 5thmonth, CT Brain was done that showed complete resolution of CSDH and gliotic areas in right cerebellar Hemisphere [Table/Fig-4].
MRI 4 weeks later shows increase in size of CSDH (14 mm) with midline shift of 4.1 mm towards left
CT Brain after 5 months shows complete resolution of CSDH
Discussion
Chronic subdural haematoma (CSDH) is associated most of the times with head injury. Most common age groups being elderly and infancy [1,2]. However, other causes of non traumatic CSDH include coagulopathy, anticoagulant therapy, vascular malformations, metastatic cancer, alcoholism, CSF shunt procedures and seizure disorders [3,4]. Traditionally treatment of CSDH has been surgical evacuation with dramatic improvement in the clinical condition [5]. However, spontaneous resolution have been reported in literature by few authors especially in elderly population with Ethem et al., reporting it in traumatic SDH in a 35-year-old male [3,4] [Table/Fig-5].
Showing reported cases of spontaneous resolution of traumatic and non traumatic CSDH
| Author | Year | Cases | Age (years) | Traumatic/ Non traumatic |
|---|
| Nagnuma et al., [6] | 1986 | 4 | 21-79 | Traumatic |
| Horikoshi [7] | 1998 | 4 | 68-75 | Traumatic |
| Parlato [4] | 2000 | 5 | 68-79 | Traumatic |
| Göksu et al., [3] | 2009 | 1 | 35 | Traumatic |
| Jukovie [8] | 2012 | 1 | 65 | Non traumatic |
| Yang et al., [9] | 2014 | 1 | 70 | Non traumatic |
| Our case | 2014 | 1 | 50 | Non traumatic |
Various theories and mechanisms of resolution of CSDH have been postulated. Yamashima et al., proposed that the platelet plug formation in the microcapillaries reduced microhaemorrhages and hence the size of SDH [5]. In those associated with anti coagulation therapy stopping of the same might help in reduction of CSDH as aspirin and clopidogrel antagonize the aggregation of platelets. When anticoagulants are withdrawn the platelet aggregation increases, resulting in the increase of bridge of endothelial gap junctions and thus reducing the volume of microbleeds [9]. This promotes the spontaneous resolution of subdural haematoma seconding the mechanism proposed by Yamashima et al., [5]. Surgical evacuation has been the treatment modality of choice ever since however conservative management have been described by various authors especially in elderly (> 70 years) with brain atrophy with minimal symptoms and mass effect. However, our case of 50-year-old male (relatively younger age) with non traumatic CSDH did not have significant brain atrophy and despite increase in size and symptoms of CSDH with continued anticoagulation therapy for cerebellar infarct there was spontaneous resolution of CSDH. Due to concomitant acute cerebellar infarct we had to continue with anti-platelet therapy with close neurological and coagulation profile monitoring as patient denied surgical evacuation of CSDH. This throws some light towards management of such patients with incidentally noted non traumatic CSDH along with another contrary lesion of the brain i.e. non haemorrhagic infarct. Though there is high risk of developing subdural haematoma with simultaneous use of aspirin and clopidogrel the absolute risk is low [10]. Probably the resolution of CSDH would take its normal course as stated by Yamashima et al., if the coagulation profile is monitored strictly for this group of patients who would require aspirin and clopidogrel for another contrary lesion [5].
Conclusion
The case highlights that certain selected cases of CSDH can be conserved if situation demands without compromising on anti-platelet therapy especially when associated with ischemic heart disease wherein stopping anti-platelet therapy might be detrimental. However, further studies will be required to affirm the role of anti-platelet agents in patients of non traumatic CSDH with contrary lesions of the brain.
[1]. Kudo H, Kuwamura K, Izawa I, Sawa H, Tamaki N, Chronic subdural haematoma in elderly people: present status on Awaji Island and epidemiological prospectNeurol Med Chir (Tokyo) 1992 32(4):207-09.PubMed PMID: 1378564 [Google Scholar]
[2]. Fogelholm R, Heiskanen O, Waltimo O, Chronic subdural haematoma in adults. Influence of patient's age on symptoms, signs, and thickness of haematomaJ Neurosurg 1975 42(1):43-46.PubMed PMID: 1167376 [Google Scholar]
[3]. Göksu E, Akyüz M, Uçar T, Kazan S, Spontaneous resolution of a large chronic subdural haematoma: a case report and review of the literatureUlus Travma Acil Cerrahi Derg 2009 15(1):95-98.Review. PubMed PMID: 19130348 [Google Scholar]
[4]. Parlato C, Guarracino A, Moraci A, Spontaneous resolution of chronic subdural haematomaSurg Neurol 2000 53(4):312-5.discussion 315-17. PubMed PMID:10825513 [Google Scholar]
[5]. Yamashima T, Yamamoto S, Friede RL, The role of endothelial gap junctions in the enlargement of chronic subdural haematomasJ Neurosurg 1983 59(2):298-303.PubMed PMID: 6864298 [Google Scholar]
[6]. Naganuma H, Fukamachi A, Kawakami M, Misumi S, Nakajima H, Wakao T, Spontaneous resolution of chronic subdural haematomasNeurosurgery 1986 19(5):794-98.PubMed PMID: 3785628 [Google Scholar]
[7]. Horikoshi T, Naganuma H, Fukasawa I, Uchida M, Nukui H, Computed tomography characteristics suggestive of spontaneous resolution of chronic subdural haematomaNeurol Med Chir (Tokyo) 1998 38(9):527-32.discussion 532-33. PubMed PMID: 9805896 [Google Scholar]
[8]. Jukovic M, Kojadinovic Z, Popovska B, Till V, Complete spontaneous resolution of compressive chronic subdural haematoma in a patient with liver failureMed Glas (Zenica) 2012 9(2):417-20.PubMed PMID: 22926390 [Google Scholar]
[9]. Yang S, Zhang X, Jin Y, Spontaneous resolution of nontraumatic chronic subdural haematoma associated with anti-aggregation therapyJ Craniofac Surg 2014 25(4):e363-65.doi: 10.1097/SCS.0000000000000814. PubMed PMID: 25006949 [Google Scholar]
[10]. Bakheet MF, Pearce LA, Hart RG, Effect of addition of clopidogrel to aspirin on subdural haematoma: meta-analysis of randomized clinical trialsInt J Stroke 2014 doi: 10.1111/ijs.12419. [Epub ahead of print] PubMed PMID: 25472690 [Google Scholar]