Spontaneous Tracheal Rupture in a Case of Interstitial Lung Disease (ILD): A Case Report
Saurabh Kumar1, Sandeep Goel2, Ashu Seith Bhalla3
1Senior Resident, Department of Radiology, AIIMS, New Delhi, India.
2Senior Resident, Department of Radiology, AIIMS, New Delhi, India.
3Additional Professor, Department of Radiology, AIIMS, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saurabh Kumar, F-7 Bali Nagar, New Delhi-110015, India.
E-mail: sunny_mamc911@yahoo.com
Spontaneous tracheal rupture is one of the rare life threatening conditions. Tracheal lacerations are generally secondary to cervical or chest trauma or occurring as a complication of endotracheal intubation. Only two cases of spontaneous tracheal rupture are reported, in adults, one due to acquired tracheobronchomalacia and other due to long term steroid use. We hereby report a very rare case of spontaneous tracheal rupture in young male patient of interstitial lung disease (ILD) who was on steroids for two months and developed spontaneous subcutaneous emphysema and pneumomediastinum. Tracheal rupture was diagnosed on unenhanced computed tomography (CT) and reconstructed virtual bronchoscopic images. Patient subsequently died due to cardiac arrest.
Fulminant hepatic failure, Hepatotoxic, Poisoning
Case Report
A 32-year-old male non smoker, non alcoholic recently diagnosed to be as a case of ILD on basis of CT was admitted to our institute with rapid progression of dyspnoea and cough for last two month. There was no history of fever or chest pain. Examination revealed cyanosis, tachypnoea, with normal vital signs. Chest examination revealed bilateral basal crepitations with occasional rhonchi. Rest of the systemic examination was unremarkable. He was on oral wysolone 40 mg for last two months.
Laboratory parameters showed raised total leukocytes count and severe type 1 Respiratory failure. He was started on oxygen inhalation, intravenous antibiotics, intravenous steroids, bronchodilator and N-acetyl cysteine. Despite our treatment patient continued to be hypoxemic but was able to maintain saturation on high flow oxygen.
On Day five of admission patient suddenly deteriorated over a period of 4-6 h with severe tachypnoea and cough not responding to anti-tussives. He was not able to maintain saturation even on high flow oxygen. Clinical examination revealed subcutaneous emphysema of the neck and on right side of the chest.
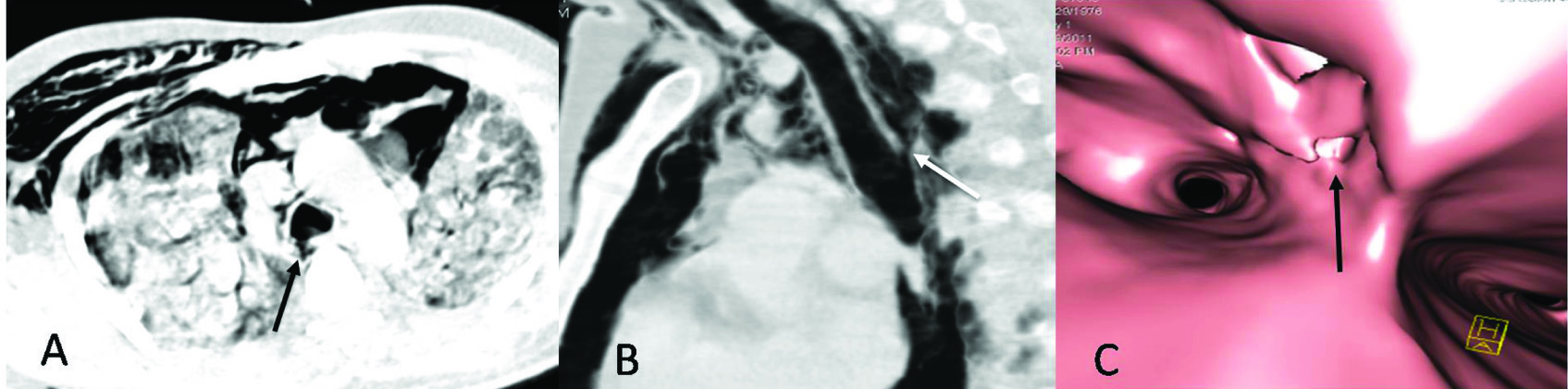
An urgent chest radiograph confirmed the findings of marked subcutaneous emphysema and pneumomediastinum with a small right sided pneumothorax. Bilateral lung fields showed ground glass opacities with reticulation consistent with ILD. Unenhanced CT of thorax revealed a defect in right posterolateral wall of trachea (6 mm tear), just 1 cm proximal to carina [Table/Fig-1a&b]. Defect in tracheal wall was also well demonstrated on virtual bronchoschopy [Table/Fig-1c]. There were diffuse ground glass opacities with interstitial septal thickening in bilateral lung fields suggestive of ReportNon-specific interstitial pneumonia (NSIP) pattern of ILD [Table/Fig-2]. There was pneumomediastinum with minimal right sided pneumothorax, subcutaneous emphysema and extension of air along great vessels into soft tissue of neck [Table/Fig-2].
Patient deteriorated within half an hour of CT scan and before he could be shifted for a surgical intervention he died due to cardio pulmonary arrest.
Discussion
Spontaneous tracheal rupture is one of the rare life threatening conditions. Tracheal lacerations are generally secondary to cervical or chest trauma or occur as a complication of endotracheal intubation. There is single case report of tracheal rupture in paediatric patients due to forceful coughing [1]. Only two cases of spontaneous tracheal rupture are reported, in adults, one due to acquired tracheobronchomalacia [2] and other associated with long term steroid use [3].
The causes [3] of tracheal rupture are broadly divided as post traumatic, post intubation and spontaneous. Spontaneous rupture of the trachea generally occurs as a result of sudden rise of intratracheal pressure. Factors which predispose to spontaneous rupture of tracheal wall include tracheal wall connective tissue weakness, which may result from prolonged corticosteroid intake, and severe coughing [4]. Tracheobronchomalacia, increasing age and Chronic obstructive pulmonary disease (COPD) are other risk factors [1].
Previously there have been isolated reports of spontaneous tracheal rupture associated with acquired tracheobronchomalacia [2], tracheal rupture in a patient of giant cell arteritis with long history of steroid intake and chronic cough [3], spontaneous tracheal rupture in paediatric patient following coughing due to tracheobronchitis [1]. To the best of our knowledge no such case has been reported in literature, of tracheal rupture in known case of ILD.
The pathophysiology of spontaneous tracheal rupture in our case is likely to be a result of severe coughing, due to underlying ILD leading to sudden rise in intratracheal pressure. The patient also had a history of prolonged steroid intake which may further have contributed to connective tissue weakness of tracheal wall.
Besides tracheal wall rupture, spontaneous pneumomediastinum and pneumothorax can be seen in patients of ILD as a result of alveolar rupture [5] due to presence of interstitial fibrosis and pulmonary vasculitis in these cases. These patients also have reduced lung compliance which leads to negative pleural and interstitial pressure leading to pneumomediastinum [5].
Spontaneous development of mediastinal and subcutaneous emphysema following episodes of coughing should raise the suspicion of tracheal rupture. Though initial investigations include soft tissue neck and chest radiographs, CT chest should be performed in such cases to localize and define the extent of tracheal tear which has important implications in management of patient. CT can show the focal defect in tracheal wall or deformity of contour or can show herniation of endotracheal tube beyond tracheal lumen [6]. CT scan, in our case, well demonstrated tracheal laceration. Tracheal laceration can also be well demonstrated on virtual bronchoscopic images reconstructed through base images. Determination of exact location of tracheal injury can help in planning further course of management. The laceration is commonly longitudinal and involves posterior membranous tracheal wall or occurs at junction of cartilaginous ring with posterior tracheal wall [1].
Besides the above mentioned imaging modalities the fibreoptic bronchoscopy also delineates the extent of tracheal injury [2] and is very useful in cases in which CT fails to demonstrate the tear in tracheal wall.
Failure to make diagnosis of tracheal rupture can prove to be fatal for patient and can result in death or severe complications including mediastinitis, stenosis of airways and permanent pulmonary function impairment [6].
Traumatic injury [3] to trachea is generally secondary to crushing chest trauma or secondary to penetrating injury to cervical trachea. Iatrogenic tracheal injury is a rare (less than 0.01%) [3] complication of endotracheal intubation. Prolonged endotracheal intubation [7] can cause pressure necrosis or erosion of the lower cervical trachea.
Surgery is the main stay of treatment, but a short laceration less than two cm length [8] and not involving the whole tracheal wall thickness can be managed conservatively. Presence of severe dyspnoea, severe pneumomediastinum, unilateral or bilateral pneumothorax and presence of deep cervical air prompts for surgical intervention.
Axial (A), reformatted sagittal (B) CT chest (lung window) and virtual bronchoscopic (C) images showing defect in right posterolateral wall of trachea proximal to carina (arrows)
Axial HRCT lung at level of upper (A) and lower lobe (B) showing bilateral ground glass opacities with areas of consolidation and septal thickening consistent with NSIP pattern. Pneumomediastinum (long white arrow) and subcutaneous emphysema (short white arrow) are also present

Conclusion
In conclusion, tracheal rupture must be carefully considered in patients of ILD having chronic cough and prolonged usage of corticosteroids and present with spontaneous subcutaneous emphysema and pneumomediastinum. If this rare entity is clinically suspected and early diagnosis using CT scan including virtual bronchoscopy and fibreoptic bronchoscopic should be performed and patients should be managed appropriately to prevent fatal outcome.
[1]. JL Roh, JH Lee, Spontaneous Tracheal Rupture after Severe Coughing in a 7-Year-Old BoyPaediatrics 2006 118(1):224-29. [Google Scholar]
[2]. Y Tsunezuka, H Sato, C Hiranuma, N Ishikawa, M Oda, G Watanabe, Spontaneous tracheal rupture associated with acquired tracheobronchomalaciaAnn Thorac Cardiovasc Surg 2003 9:394-96. [Google Scholar]
[3]. C Rousié, HV Damme, MA Radermecker, P Reginster, C Tecqmenne, R Limet, Spontaneous Tracheal Rupture: a Case ReportActa chir belg 2004 104:204-08. [Google Scholar]
[4]. JM VanDer Klooster, AF Grootendorst, PJ Ophof, JW Brouwers, Pneumomediastinum: an unusual complication of bronchial asthma in a young manNeth J Med 1998 52:150-54. [Google Scholar]
[5]. A Patel, B Kesler, AW Robert, Persistent Pneumomediastinum in Interstitial Fibrosis Associated With Rheumatoid Arthritis: Treatment With High- Concentration OxygenChest 2000 117:1809-13. [Google Scholar]
[6]. JD Chen, K Shanmuganathan, SE Mirvis, KL Killeen, RP Dutton, Using CT to Diagnose Tracheal RuptureAJR 2001 176:1273-80. [Google Scholar]
[7]. HS Hofmann, G Rettig, J Radke, H Neef, RE Silber, Iatrogenic ruptures of the tracheobronchial treeEur J Cardio- Thor Surg 2002 21:649-52. [Google Scholar]
[8]. S Gabor, H Renner, H Pinter, Indications for surgery intracheobronchial rupturesEur J Cardiothorac Surg 2001 20:399-404. [Google Scholar]