Focal Choroidal Excavation in Best Vitelliform Macular Dystrophy: Case Report
Mohammad Riazi Esfahani1, Hamid Riazi Esfahani2, Alireza Mahmoudi3, Mohammad Karim Johari4, Karim Hemati5
1Professor, Department of Ophthalmology, Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran.
2Resident, Department of Ophthalmology, Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran.
3Resident, Department of Ophthalmology, Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran.
4Resident, Department of Ophthalmology, Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran.
5Associate Professor, Department of Anesthesiology, Emam Khomieni Hospital, Ilam University of Medical Sciences, Ilam, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Karim Hemati, Associate Professor, Department of Anesthesiology, Emam Khomieni Hospital, Ilam University of Medical Sciences, Ilam, Iran.
E-mail: Khematy@gmail.com
Focal choroidal excavation (FCE) was first reported as a choroidal posteriorly excavated zone without any scleral change. Choroidal excavation also divided into conforming and nonconforming type. Numerous reports demonstrated association between FCE and other disease such as choroidal neovascularization and central serous choroidoretinopathy. Here, we report a rare case of FCE in a patient with Best disease. The patient was diagnosed by spectoral domain optical coherence tomography (SD-OCT). To the best of our knowledge, our patient is the second report of choroidal excavation in Best vitelliform macular dystrophy.
Best dystrophy, Fluorescein angiography, OCT
Case Report
A 35-year-old woman presented to Retina clinic at Farabi Eye Hospital in September 2011, with complaint of blurred vision from several years ago. She did not have any history of trauma, retinal or choroidal vascular disease, or prior retinal or choroidal inflammation. Her best-corrected visual acuity was 20/25 in her right eye and 20/20 in her left eye with no significant refractive error.
Slit lamp examination of anterior segment was unremarkable. Dilated fundus examination of both eyes revealed RPE mottling changes with subretinal yellowish white plaque in macular area. Intraocular pressures (IOP) were measured 14 mmHg and 16 mmHg in the right and left eye, respectively, using Goldmann applantation tonometer.
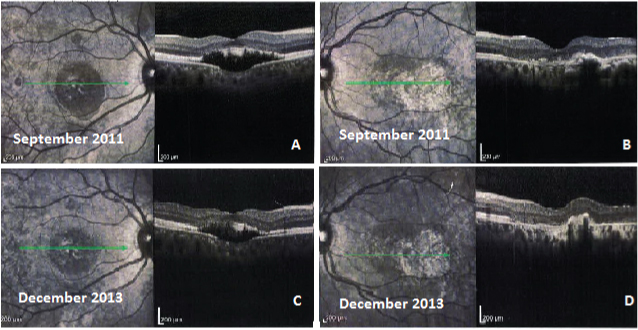
SD-OCT of the right eye revealed a cup-shaped focal choroidal excavation in the macula with detachment between retinal pigment epithelium (RPE) and sensory retina layers. Disturbances of the outer retinal layers within the choroidal excavation area were obvious. SD-OCT also showed subretinal hyper reflective material. The retinal layers from the retinal nerve fiber layer to the outer plexiform layer were essentially intact [Table/Fig-1]. SD-OCT of the left eye revealed disturbance of the RPE and photoreceptors layers and small subretinal fluid without obvious excavation [Table/Fig-1].
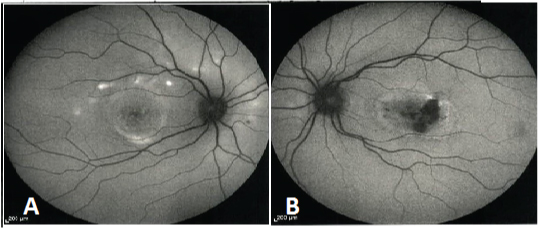
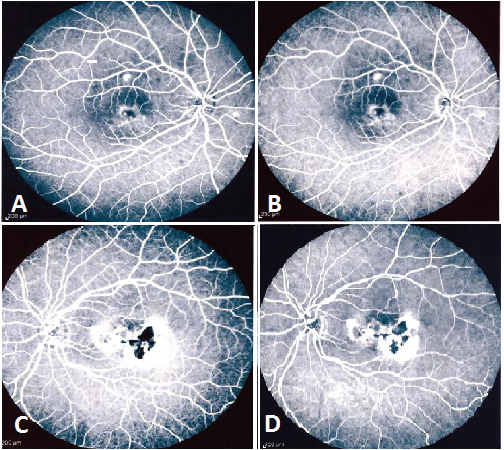
Fundus autoflourecence images of the both macular region showed an outer circumferential ring of hyperfluorescence. Moreover in the left eye, central hypofluorescent areas were seen [Table/Fig-2]. Fluorescein angiography (FA) of the right eye revealed irregular hyperfluorescence in early phase corresponding to the RPE attenuation over the macular area that remained without change until late phases. In the left eye, there were hyperfluorescence areas in early phases. During mid to late phases, more hyperfluorescent areas in consistent with staining of materials were obvious. No leakage was observed in both eyes [Table/Fig-3].
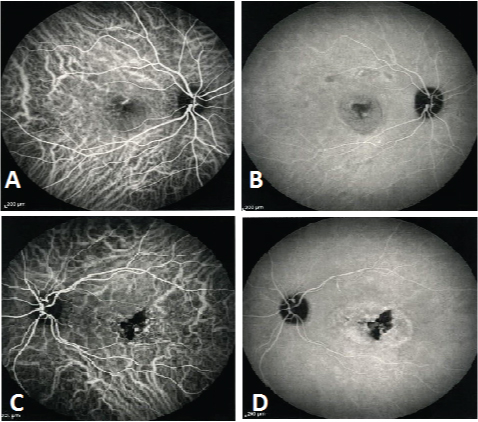
Indocyanine green angiography (ICG) of both eyes was near normal without any hyper-permeability in late stages, though mild dilation of submacular choroidal vessels was seen [Table/Fig-4]. Electroretinogram (ERG) was normal but Electrooculogram (EOG) was demonstrated a sever loss of the light response (low Arden ratio).The patient was followed up annually without any treatment, at each follow-up imaging was performed (OCT, FA). No change was observed in the course of the disease.
Discussion
Best vitelliform macular dystrophy (VMD) also known as best disease is an autosomal dominant retinal dystrophy caused by heterozygous mutations in the bestrophin 1 gene [1] . Affected individuals show a solitary or multifocal vitelliform lesion (yolk like) in the macula with good visual acuity in childhood [2] .
Histopathologic evaluations, Spectral domain Optical coherence tomography (SD-OCT) and fundus autofluorescense (FAF) indicated lipofuscin accumulations at the level of the Retinal pigment epithelium (RPE) and also revealed atrophy and disruption of the RPE/photoreceptor complex [1-3] .
In 2006, FCE was first reported as a peculiar OCT finding in otherwise healthy eye by Jampol et al., as a choroidal posteriorly excavated zone without evidence of staphyloma or any scleral changes at that area [4] . Since that time, numerous reports have been raised about the choroidal excavation and association between focal choroidal excavation (FCE) and Choroidal neovascularization [5,6] , Epstein–Barr virus infection [7] Best disease [3] Polypoidal choroidal vasculopathy [8] and Central Serous Chorioretinopathy [9,10] .
Margolis et al., demonstrated two type of choroidal excavation; excavations that involved the outer retina up to external limiting membrane without separation between RPE and photoreceptor (conforming type) and excavations that involved the RPE with separation between the outer retina and the RPE within it (nonconforming) [11] . The aetiology of FCE is still unknown, but it has been suggested that FCE is a congenital abnormality or may be multifactorial [12] . FCE have also divided in two patterns by Wakabayashi et al., one that involved the outer retinal layers up to the external limiting membrane (ELM), and other that involved only the retinal pigment epithelium (RPE) [13] .
Several theories have been postulated about the aetiology of FCE, including [7,10,11] : failure of the choroidal development in the embryonic stage, microstaphyloma, focal choroidal atrophy due to congenital or acquired choroiditis, EBV infection and contraction of focal choroidal scarring. Nevertheless the aetiology of afore mentioned disease is currently unknown and further prospective study on FCE is necessary to clarify its aetiology, clinical course, and visual prognosis. Ellaban et al., reported that FCE was seen in 7.8% of eyes with central serous chorioretinopathy (CSCR) [10] . Also, Lee et al., found that CSCR was present in 24.4% of FCE eyes [14] .
Suzuki et al., stated that an intervening hyporeflective space in the nonconforming FCE may represent serous retinal detachment (SRD) due to improper pumping action of RPE at the FCE [9] . They also stated that each of conforming or nonconforming FCE may be appeared after resolution of subretinal fluid.
Conforming FCE may progress to nonconforming FCE with separation of the photoreceptor tips from the apical surface of the RPE due to tension stress on outer retina, resulting in accumulation of fluid in subretinal space. These phenomena accompany with loss of vision due to shedding of photoreceptors in that space like a chronic CSR [11] . According to Margolis et al., classification, our patient had a nonconforming choroidal excavation. Given the our patient’s history, persistent metamorphopsia without significant change in vision over time, It seems that FCE in our case was nonconforming type from the long period of time and SRD in this case is not a secondary event. This may support this hypothesis that FCE size and shape would remain stable [14] .
(a) SD-OCT of the right eye showing focal nonconforming choroidal excavation (b) SD-OCT of the right eye about 20 months after first image
(c,d) SD-OCT of the left eye showing disturbance of the RPE and photoreceptors layers without obvious excavation
(a) FAF of the right eye showing circular hyperfluorescence ring around macular area that is related to residual vitelliform material
(b) FAF of the left eye revealing central hypofluorescence area surrounded by granular hyperflurecence circle
(a,c) Fluorescein angiography of the both eyes revealed irregular hyperfluorescence in early phase (b,d) That remained without change until late phases. No leakage was observed in both eyes
(a,c) Indocyanine green angiography (ICGA) of both eyes shows early-stage choroidal vascular dilation just superior to the macula (b,d) There is no leakage during late phases
Conclusion
To the best of our knowledge, our patient is the second report of choroidal excavation in Best vitelliform macular dystrophy. Finally there may also be an association or a Causal relationship between best disease and FCE, which requires further studies to confirm.
[1]. H Bitner, P Schatz, L Mizrahi-Meissonnier, D Sharon, T Rosenberg, Frequency, genotype, and clinical spectrum of best vitelliform macular dystrophy: data from a national center in DenmarkAmerican journal of ophthalmology 2012 154(2):403-12. [Google Scholar]
[2]. G Querques, M Regenbogen, G Soubrane, EH Souied, High-resolution spectral domain optical coherence tomography findings in multifocal vitelliform macular dystrophySurvey of ophthalmology. 2009 54(2):311-16. [Google Scholar]
[3]. MB Parodi, I Zucchiatti, F Fasce, F Bandello, Bilateral choroidal excavation in best vitelliform macular dystrophyOphthalmic surgery, lasers & imaging retina 2014 45:e8-e10. [Google Scholar]
[4]. LM Jampol, J Shankle, R Schroeder, P Tornambe, RF Spaide, MR Hee, Diagnostic and therapeutic challengesRetina 2006 26(9):1072-76. [Google Scholar]
[5]. JH Lee, WK Lee, Choroidal neovascularization associated with focal choroidal excavation.American journal of ophthalmology 2014 157(3):710-8. [Google Scholar]
[6]. H Xu, F Zeng, D Shi, X Sun, X Chen, Y Bai, Focal choroidal excavation complicated by choroidal neovascularizationOphthalmology 2014 121(1):246-50. [Google Scholar]
[7]. MC Savastano, M Rispoli, L Di Antonio, L Mastropasqua, B Lumbroso, Observed positive correlation between Epstein-Barr virus infection and focal choroidal excavationInternational ophthalmology 2014 34(4):927-32. [Google Scholar]
[8]. EA Say, PD Jani, MF Appenzeller, OM Houghton, Focal choroidal excavation associated with polypoidal choroidal vasculopathyOphthalmic surgery, lasers & imaging retina 2013 44(4):409-11. [Google Scholar]
[9]. M Suzuki, F Gomi, C Hara, M Sawa, K Nishida, Characteristics of Central Serous Chorioretinopathy Complicated by Focal Choroidal ExcavationRetina 2014 34(6):1216-22. [Google Scholar]
[10]. AA Ellabban, A Tsujikawa, S Ooto, K Yamashiro, A Oishi, I Nakata, Focal choroidal excavation in eyes with central serous chorioretinopathy American journal of ophthalmology 2013 156(4):673-83. [Google Scholar]
[11]. R Margolis, SK Mukkamala, LM Jampol, RF Spaide, RF Spaide, JA Sorenson, The expanded spectrum of focal choroidal excavationArchives of ophthalmology 2011 129(10):1320-25. [Google Scholar]
[12]. R Obata, H Takahashi, T Ueta, K Yuda, K Kure, Y Yanagi, Tomographic and angiographic characteristics of eyes with macular focal choroidal excavationRetina 2013 33(6):1201-10. [Google Scholar]
[13]. Y Wakabayashi, A Nishimura, T Higashide, S Ijiri, K Sugiyama, Unilateral choroidal excavation in the macula detected by spectral-domain optical coherence tomographyActa ophthalmologica 2010 88(3):e87-91. [Google Scholar]
[14]. CS Lee, SJ Woo, YK Kim, DJ Hwang, HM Kang, H Kim, Clinical and Spectral-Domain Optical Coherence Tomography Findings in Patients with Focal Choroidal ExcavationOphthalmology 2014 121(5):1029-35. [Google Scholar]