Introduction
In obstetrical practice induction of labour (IOL) is aimed at stimulation of uterine contractions after period of viability before the onset of spontaneous labour irrespective of status of membranes [1]. Presently, IOL is done for approximately 20% of pregnancies for various maternal and fetal indications [2,3] and nearly 20% of labour inductions end up in caesarean deliveries [4]. Successful induction depends largely on cervical characteristics or simply referred to as “readiness of cervix or cervical ripening” and Bishop Score is the gold standard traditional method of assessing favourability of the cervix in predicting whether an induced labour will result in successful vaginal delivery [5]. However, this assessment is subjective, biased by inter observer variations and studies have shown poor predictive value [6-8]. Digital examination may not measure the length of the cervix very precisely [9]. Other parameters of the score, such as consistency and position of the cervix are to some extent subjective and imprecise [10]. Effacement of the cervix is highly subjective and varies considerably among examiners [11]. Assessment of cervix digitally is also reported to be associated with fear of examination, pain, anxiety and discomfort [12]. Supravaginal portion of cervix comprises about half the length of cervix which is difficult to assess digitally and this is highly variable among subjects [13]. Transvaginal ultrasound (TVS) is an objective and well tolerated method not only to assess cervical length but also to detect changes at the internal os [14]. TVS can represent more accurate measurement of cervical length (including supravaginal portion), and these measurements are quantitative and easily reproducible hence can ar5remove interobserver variations [15]. Evaluation of cervixby TVS can be useful in predicting successful labour induction i.e., initiation of active labour represented by cervical dilatation >4 cm in the presence of uterine contractions [16]. The purpose of present work is to study the sonographic equivalent components of Bishop Score and to formulate an ultrasound (TVS) scoring system and compare its performance with Bishop Score in predicting successful labour induction.
Materials and Methods
This was a prospective observational study of pregnant women who underwent labour induction between August 2009 to July 2012 in a university hospital setting. Sample size was determined according to the method described in the next paragraph. Written and informed consent was taken from all patients who were included in the study. All patients with singleton gestation at 37 completed weeks up to 42 weeks with vertex presentation, longitudinal lie, live fetus, intact membranes and no vaginal bleeding were included in the study. Patients with previous cesarean delivery, antepartum haemorrhage and cephalopelvic disproportion were excluded and finally a total of 107 subjects were available for analysis. The study received approval of the Ethics committee of the hospital. Patients were asked to empty bladder. Cervical assessment by TVS was done by using TOSHIBA Nemo machine (TVS probe-5 Hz). The probe was gently placed in the vagina just below the cervix avoiding undue pressure which otherwise would distort the cervical configuration. All the measurements were taken in sagittal view which included presence of both internal and external os, cervical canal and its gland area. Following parameters were assessed: length of the cervix from the internal to external os, presence or absence of funneling and if present width and length of funnelling at internal os were measured. Distance between presenting part to external os was measured and position of the cervix i.e. whether curved or straight was also noted. For measuring cervical length and distance between presenting part to external os, minimum of three measurements were taken and the shortest and technically appropriate measurements were recorded. Following the TVS examination, digital examination was done to by the person who was blinded to the TVS findings. We have used Burnett modified bishop Score [Table/Fig-1] with a scale of zero to maximum ten [17]. These parameters were carefully selected to match the components of modified Bishop Score, like cervical length was comparable to effacement of cervix. Funneling depicted by ultrasound was comparable to cervical dilatation and distance between presenting part to external os was the counterpart of station in Bishop Score. Ultrasound (TVS) scoring system was formulated with the above mentioned parameters [Table/Fig-2]. Each parameter was Scored from 0-2, maximum TVS Score was 10.
Sample Size Calculation
Radeka et al conducted a prospective, blind, observational study on Bishop Score to evaluate successful induction of with endovaginal prostaglandins. Induction was successful in 74% and unsuccessful in 26% [18]. They found that Bishop Score has sensitivity of 65.5%, specificity of 95%. Based on this information, we calculated minimum required sample size according to method described by Jone et al., [19].
Sample size based on sensitivity
N = {Z21-α/2 × Sn × (1-Sn)} / {L2 × Pα}
Sample size based on specificity
N = {Z21-α/2 × Sp × (1-Sp)} / {L2 × Pß}
wherein
N = number of patients
Z1-α/2 = 1.96 (standard normal deviate value that divides the central 95% of z distribution from 5% in the tails)
Sn = reported sensitivity (65.5%, i.e., 0.655),
Sp = reported specificity (95%, i.e., 0.95)
L = absolute precision desired on either side (half width of the confidence interval of the confidence interval) of sensitivity/specificity (10% i.e., 0.1)
Pα = Prevalence of successful induction (74%, i.e., 0.74),
Pß = Prevalence of failure of induction (26%, i.e., 0.26)
The sample size calculation based on sensitivity was 114 and based on specificity was 76. Thus any sample size above 114 is more than adequate with respect to both required sensitivity and specificity.
Induction was carried out within one hour of cervical assessment, as per protocol of labour ward. In case of unfavourable cervix, labour induction was done by intracervical instillation of Dinoprostone (PGE2) gel, 0.5 mg in 3 gm of gel, if the patient did not exhibit regular uterine contractions and cervical changes after eight hours, induction was repeated. Maximum of three inductions were done over 24 hours. If the Bishop Score was found to be favourable, amniotomy was done followed by 2 units of intravenous oxytocin at the rate of 2mIU/min (8 drops/min) and gradually increased exponentially till maximum of 16mIU/ min (60 drops/min). Primary outcome of this study was the onset of active labour i.e. onset of regular uterine contractions (at interval of 2-3 minutes) and cervical dilatation of 4 cm or greater within 24 hours of induction.
There were 131 patients who were initially enrolled in the study. The mean age of the patients was 26.4 years (SD 3.55, range 21-35). The BMI (kg/m2) ranged from 17.8 to 34.6 (Mean 23.9 ± SD 3.6). The majority of patients were primigravidae (89 ie, 67.6%). All 131 patients underwent induction of labour as per said protocol. Twenty four of them could not continue in the study they were taken up for operative delivery (foetal distress 21, appearance of vaginal bleeding 3). The remaining 107 patients (these patients represent the actual research population of present study) could complete the induction protocol and 14 of them did not respond to induction and were taken up for operative delivery with the indication as “failed induction”. Of remaining 93 patients, 86 delivered vaginally and of them went into active phase of labour. The 86 of them delivered vaginally successfully and 7 of them had caesarean delivery for indications which occurred in active phase of labour (non progress of labour, foetal distress) [Table/Fig-3]. Non progress of labour in active phase was defined according to modified WHO partograph (all our patients had partographic management of labour and foetal heart was monitored by cardiotocography in all patients) and included any of following conditions; protracted active phase of labour (cervical dilatation crossing alert line), secondary arrest of cervical dilatation (< 1cm / hour) and absence of descent of fetal head despite good uterine contractions. Consortium statement is given pictorially.
Statistical Analysis
The values of various variables were entered into computer software (SPSS software, version 16, Chicago II, USA). The various means and standard deviations were calculated using descriptive statistics. Kolmogorov-Smirnov test was used to test the normality of observed measurements. Categorical variables were analysed using cross tabulation feature of the software and to determine the statistical significance. Pearson Chi-Square test (with Yate’s correction) was applied. The best cut off values for Bishop Score and ultrasound Score were computed using Receiver Operator Characteristic (ROC) analysis. The diagnostic characteristics of these cut off points were assessed using sensitivity, specificity, positive and negative likelihood ratio with their 95% confidence intervals and area under the curve (AUC) reflected the true abilities of these two Scores. Logistic regression analysis was used to determine the relationship between success of induction and various components of Bishop Score and Ultrasound Score. Kaplan-Meier analysis was done to study the relationship between duration of labour at two cut offs of these two Scores as determined by ROC analysis. Log Rank (Mantel-Cox) test was used to find statistical differences in mean duration of labour in these groups. The hazard ratios were calculated for various covariates using the Cox proportional hazards model. The results were considered significant at two tailed p-value less than 0.05.
Results
The maternal characteristics of 107 patients who completed the induction protocol are given in the [Table/Fig-4]. Increasing maternal age (>30 years) and higher BMI (≥30) appeared to be significantly associated with higher percentage of failed induction. Though failed induction rates were more in primigravida (16% vs. 6.3%), the difference was not statistically significant.
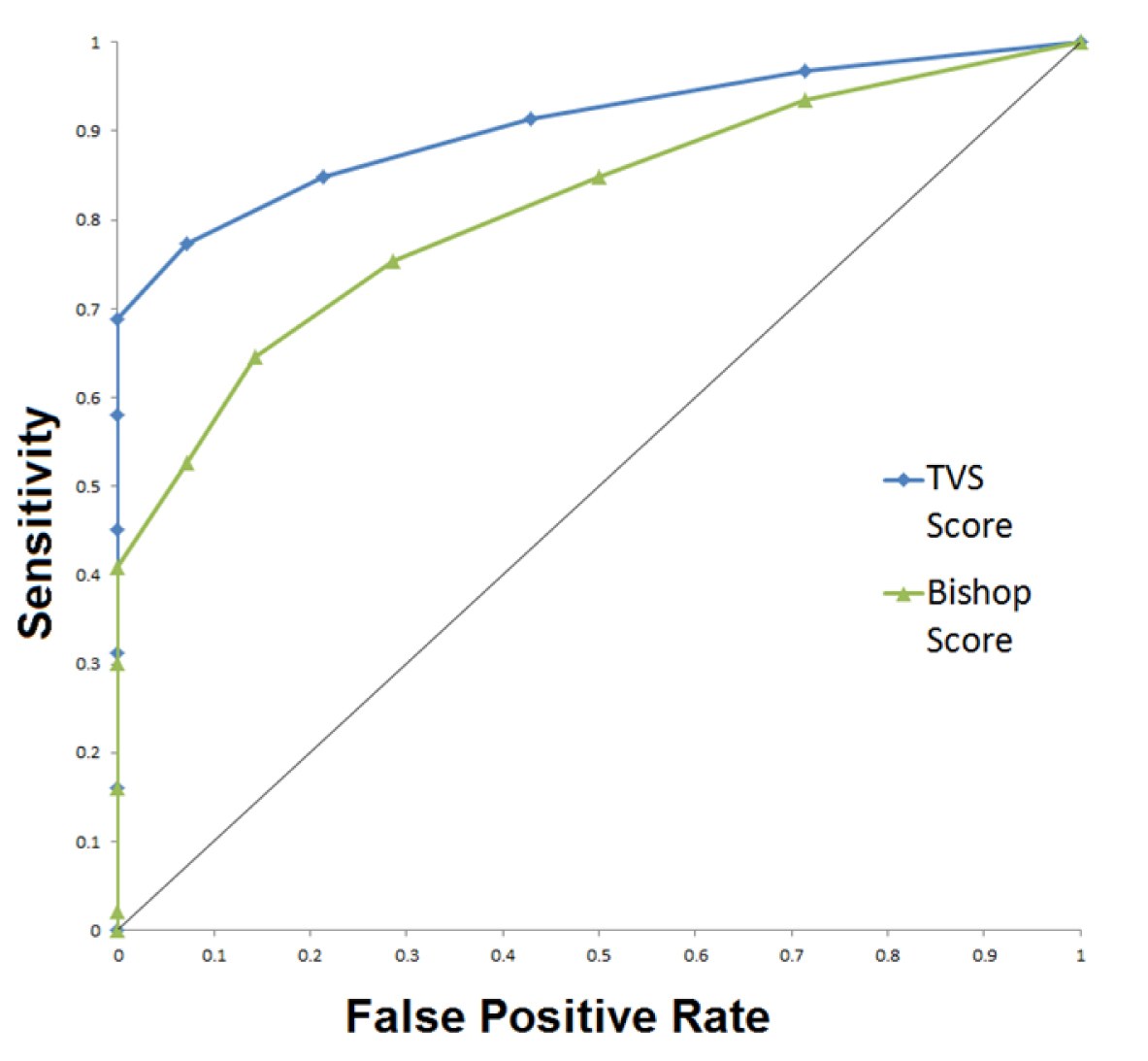
[Table/Fig-5] represents sensitivity, specificity and other diagnostic parameters as indicated by ROC analysis. We have truncated wide range of cut points to few cut off values for Bishop Score and Ultrasound Score (three each) which have shown acceptable sensitivity and specificity. It is well known that in ROC analysis, with incremental increase in cut off value, the sensitivity and specificity 6values show reciprocal relationship and the best cutoff value would be one that produces a combination of maximum sensitivity and specificity. From [Table/Fig-5] it can be seen that at cut of values of Score of ≥ 4 produces best of the combinations for both Bishop Score and Ultrasound Score, and among the two ultrasound Score performs better than Bishop Score in all aspects. [Table/Fig-6] shows comparison of AUC for these two methods of cervical assessment to predict successful active phase of labour. The correct classification rate {CCR, i.e., (True Positives + True Negatives)/N} was 67.3% for Bishop Score and 79.4% for Ultrasound Score.
We performed multiple logistic regression analysis to examine the relationship between successful induction of labour and various components of two scoring systems. The five variables of Bishop Score and Ultrasound Score were entered in SPSS program as predictor variables and the outcome of induction (success or failure) as outcome variables and stepwise regression analysis was carried out to find the association between individual components of these two scoring methods and successful induction. The strength of the association was determined by p-value for the odd’s ratio [Table/Fig-7]. Odd’s ratio of more than one, indicates positive correlation (increase in the value of parameter results in higher success), whereas ratio less than one indicates negative correlation (increased measurement results in lower success). It was found that dilatation of the cervix was the single most predictor of successful induction with respect to Bishop Score, whereas cervical length and distance from presenting part to external os predicted success in ultrasound Score. Statistical derivations showed that an increase of 1 mm in cervical length (from mean cervical length of 2.54 cm) increased the odds of failure of induction by 6.5% and similarly 1 mm increase in head distance from external os (from mean distance of 2.79 mm) increased the odd of failure by 11%.
[Table/Fig-8] explains the survival curves (Kaplan Meier) for Bishop Score and USG Score at two cut off values (<4 & ≥ 4). We have defined “vaginal delivery” as desired “event” (instrumental deliveries also included). Women experiencing caesarean deliveries (for various indications as mentioned in [Table/Fig-4] ) were censored. It can be seen that women with USG Score ≥ 4 progressed well in labour and delivered in a shorter time than those with Score <4 (mean duration of labour 14.07 hours vs. 18.45 hours) and this was statistically significant (p<0.0001, Mantel-Cox log rank test). [Table/Fig-9] explains the statistical results related to survival analysis. The life table analysis further indicated that at the end of 16 hours of labour, only 10% of women with USG Score ≥ 4, whereas more than 90% of women with USG Score < 4 had not yet delivered. This means that ultrasound not only differentiates those women with favourable cervix from those without and also shorter duration of labour, though this phenomenon may be attributed to the fact that women with good Score would have already achieved significant amount of progress with regard to initial dilatation and foetal head descent.
We have used Cox proportional regression model for calculating hazard ratio [Table/Fig-10] for Bishop Score and Ultrasound Score. We defined occurrence of vaginal delivery as completion of the event and this was technically considered as hazard, meaning parameter having higher hazard ratio (HR) literally meant achieving successful vaginal birth. Ultrasound scoring of cervix was significantly associated with higher hazard function for Score ≥ 4 (6.96, p<0.001) compared to Bishop Score ≥ 4 (1.32, p=0.23, N.S. - statistically not significant), indicating faster progression to vaginal delivery. Again further statistical analysis (not shown) indicated that transvaginally measured cervical length and foetal head distance were significantly contributing to hazard ratio in USG Score group.
In our series, there were no complications (for example uterine hyper stimulation, amniotic fluid embolism etc.) related to intracervical PGE2 instillation. We had three cases of sudden vaginal bleeding and were immediately taken up for caesarean section. There were no maternal and perinatal mortality in our study.
Discussion
In modern obstetrical practice induction of labour has been tried in one of every five deliveries for various maternal and/or fetal indications and incidence is gradually rising [3]. In appropriate selection of cases results in failure of induction and raised rates of intrapartum caesarean sections, there by significantly increasing maternal and fetal morbidity associated with these interventions. Hence, pre-induction counseling and explaining the chances of successful inductions is of paramount importance and any tool that helps the physician in estimating favourable outcome will be indispensable. Few studies have indicated that inductions solely based upon bishop Scores have resulted in increased number of prostaglandin inductions and incorporating ultrasound in decision making have significantly reduced the need for prostaglandin usage from 75% to 36% [20].
Several studies in the past have evaluated the efficacy of ultrasound in prediction of successful labour induction and have reached some conclusion that ultrasound performs better than Bishop Score. However, these studies have focused mainly upon transvaginal measurement of cervical length and not on other equivalent ultrasound representatives of Bishop Score components. In this direction, the present study is the one of its kind to formulate a composite USG (TVS) scoring system that can be used to predict successful labour induction. The following table [Table/Fig-11] shows how ultrasound parameters were matched to components of Bishop Score.
Ultrasound has specific advantages over digital examination. It can assess full cervical length and status of internal os without invading endocervical canal and hence is less invasive, and more objective [9]. The ultrasound findings can be documented by taking pictures and is reproducible. Other co-existing findings like compound presentation and occult cord presentation if present can be documented, which can be easily missed by doing just a digital examination.
Earlier it was thought that there are certain advantages of Bishop Score over ultrasound assessment, for example, parameters such as cervical consistency and position could only be measured by pervaginal examination [4]. The results of this study shows that other parameters of Bishop Score such as cervical length, effacement and station of the head can be measured more accurately and objectively and one can add other parameters such as cervical canal configuration and funnel length to construct an ultrasound scoring system which can perform better than digital scoring.
In the past, many studies that have compared cervical length with Bishop Score have shown variable results [14]. GK Pandis et al., from Harris Birthright Research Centre for Fetal Medicine, London carried out a multicenter study on 240 women with singleton pregnancies at 37-42 weeks period of gestation and they found that cervical length alone appeared to be a better indicator of successful vaginal delivery within 24 hours compared to Bishop Score [21]. R Gabriel et al., from France too had similar observations and in their series of 179 patients, they observed that in women with poor Bishop Score, a cervical length of <26 mm, the caesarean rates were less and labour was not prolonged [6]. SM Rane et al., have too opined that cervical length estimation is better than Bishop Score in their series of 382 prolonged pregnancies [22]. Soon Ha Yang et al., from Seoul, South Korea, concluded that cervical length <3.1 cm by TVS was a better predictor of active phase of labour than Bishop Score of >4 [23]. In 2007 Ana M Gomez et al., also found that cervical length <2.4 cm by TVS was a better predictor of successful vaginal delivery than Bishop Score> 4 [24]. A meta-analysis published concluded that cervical length by USG was not an effective predictor of successful labour induction [25]. However, some studies have reported that ultrasound is no more than better than Bishop Score. In a study done by H Roman et al., concluded that Bishop Score is a better predictor than cervical length by USG in predicting successful labour induction [26].
JL Bartha et al., have opined that a combination of Bishop Score and ultrasonically measured cervical length and wedging predicts high success rates for induction of labour [27]. In their series of 85 patients they found that if Bishop Score <6, cervical length >3 cm and weding <30%, used as criterial for labour induction instead of Bishop Score alone, the need for intracervical prostaglandins reduced significantly by 35%. Studies from 2006 onwards have focussed on combinations of several other parameters such as history, clinical examination details and ultrasound findings. HP Dietz et al., from University of Sydney, Australia conducted a prospective observational study on 202 patients between 36 to 40 weeks of gestation [28]. They assessed maternal age, parity, previous operative delivery, Bishop Score and translabial ultrasound assessment of cervial length, bladder position on Valsalva and fetal head engagement. Multivariate logistic regression analysis indicaed that a model comprising of maternal age, BMI, previous operative delivery, Bishop Score, sonographic cervical length, bladder position and head engagement had the best discriminatory power to predict successful vaginal delivery. However a Dutch study which included above parameters reported only a moderate predictive capacity and they concluded that such prediction models should be used with caution in clinical practice [29]. Eggebo et al., from Norway constructed a validation model including three ultrasound parameters viz, tranperineally measured foetal head distance, transvaginally measured posterior cervical angle (angle between cervical canal and posterior uterine wall) and cervical length along with digitally measured cervical dilation on a 8 point scale, which could predict successful induction of labour as high as 71% of patients planned for delivery (95% CI 61-80%, p<0.01) [9]. The ultrasound scoring in our study is based upon 0 – 10 point scale and does not include any clinical examination parameter and we assume that such a scoring system can be highly objective, authentically documented and easily reproducible.
TVS was well tolerated by all patients in our study, so we propose that this scoring system can be used in clinical practice to evaluate and follow up the cervical Score in term patients once pelvis has been assessed by digital examination, this will help to reduce frequent digital examinations of cervix which can be associated with premature rupture of membranes. Other co-existing findings like compound presentation and occult cord presentation if present can be documented, which can be easily missed by doing just a digital examination.
Modified Bishop Score (Burnett)
| Score | 0 | 1 | 2 |
| Dilatation of cervix | < 1 cm | 1- 2 cm | >1 cm |
| Cervical length | >2 cm | 1- 2 cm | < 1 cm |
| Position of cervix | Posterior | Mid | Anterior |
| Consistency of cervix | Firm | Soft | Soft and stretchable |
| Station of Head | ≥ -2 | -1 | ≥0 |
(Score range: minimum 0, maximum 10)
Transvaginal Ultrasound (TVS) cervical Score.
| Score | 0 | 1 | 2 |
| Cervical length | >3 cm | 2-3 cm | < 2 cm |
| Funnel length | Absent | ≤ 0.5 cm | >0.5 cm |
| Funnel width | Absent | ≤ 0.5 cm | >0.5 cm |
| Position of cervix | Curved | - | Straight |
| Distance of presenting part to external os | >3 cm | 2-3 cm | < 2cm |
(Score range: minimum 0, maximum 10)

Demographic characteristics of 107 patients who completed induction protocol
| Parameters | Women who had active labour n (%) | Women who had failed inductions n (%) | p-value (Pearson Chi-Square) |
|---|
| Age ( years) |
| 20-25 | 44 (93.6) | 3 (6.4) | 0.039 |
| 26- 30 | 38 (86.4) | 6 (13.6) |
| 31-35 | 11 (68.7) | 5 (31.3) |
| Parity |
| Primi | 63 (84) | 12 (16) | 0.17 |
| Multi | 30 (93.7 ) | 2 (6.3) |
| BMI (kg/m2) |
| < 18.5 | 2 (66.7) | 1 (33.3) | 0.032 |
| 18.5- 24.9 | 60 (93.7) | 4 (6.3) |
| 25- 29.9 | 26 (81.3) | 6 (18.7) |
| ≥30 | 5 (62.5) | 3 (37.5) |
Diagnostic characteristics of Bishop Score and Ultrasound Score in predicting successful active phase of labour
| Scoring methods | Cut off Scores | Sensitivity (95% CI) | Specificity (95% CI) | Positive Likelihood ratio (95% CI) | Negative Likelihood ratio (95% CI) | AUC (95% CI) | p-value |
|---|
| Bishop Score | ≥ 2 | 84.95 (76.0 - 91.5) | 50 (23.1 - 76.9) | 1.7 (1.0 - 2.9) | 0.3 (0.1 - 0.6) | 0.815 (0.728 - 0.883) | 0.0001 |
| ≥ 3 | 75.27 (65.2 - 83.6) | 71.43 (41.9 - 91.4) | 2.63 (1.9 - 3.7) | 0.35 (0.1 - 0.9) |
| ≥ 4 | 64.52 (53.9 - 74.2) | 85.71 (57.2 - 97.8) | 4.52 (3.5 - 5.9) | 0.41 (0.1 - 1.5) |
| Ultrasound Score | ≥ 2 | 91.4 (83.7 - 96.2) | 57.14 (28.9 - 82.2) | 2.13 (1.3 - 3.4) | 0.15 (0.06 - 0.4) | 0.907 (0.835 - 0.955) | 0.0001 |
| ≥ 3 | 84.95 (76.0 - 91.5) | 78.57 (49.2 - 95.1) | 3.96 (3.0 - 5.3) | 0.19 (0.06 - 0.6) |
| ≥ 4 | 77.42 (67.6 - 85.4) | 92.86 (66.1 - 98.8) | 10.84 (9.0 - 13.0) | 0.24 (0.04 - 1.7) |
Comparison of ROC curves for TVS and Bishop Scores
Relationship between successful active phase and various components of Bishop and USG Scores according to multiple logistic regression analysis.
| Odd’s Ratio | 95% CI for odd’s ratio | p-value |
|---|
| Bishop Score |
| Dilatation of cervix | 7.6398 | 2.205 to 26.467 | 0.0013 |
| Cervical length | 0.9768 | 0.337 to 2.832 | 0.9656 |
| Station of head | 0.31405 | 0.082 to 1.203 | 0.0949 |
| Manipal USG Score |
| Cervical length | 0.1448 | 0.044 to 0.472 | 0.0014 |
| Funnel length | 1.1529 | 0.861 to 1.543 | 0.3391 |
| Funnel width | 0.9033 | 0.653 to 1.250 | 0.5398 |
| Distance of presenting part to external os | 0.0226 | 0.002 to 0.217 | 0.0012 |
2 components from Bishop Score (consistency and position) and one from USG Score (direction of cervical canal) were not analysed as they represented ordinal variables
Kaplan – Meir survival analysis for Bishop Score and USG Score
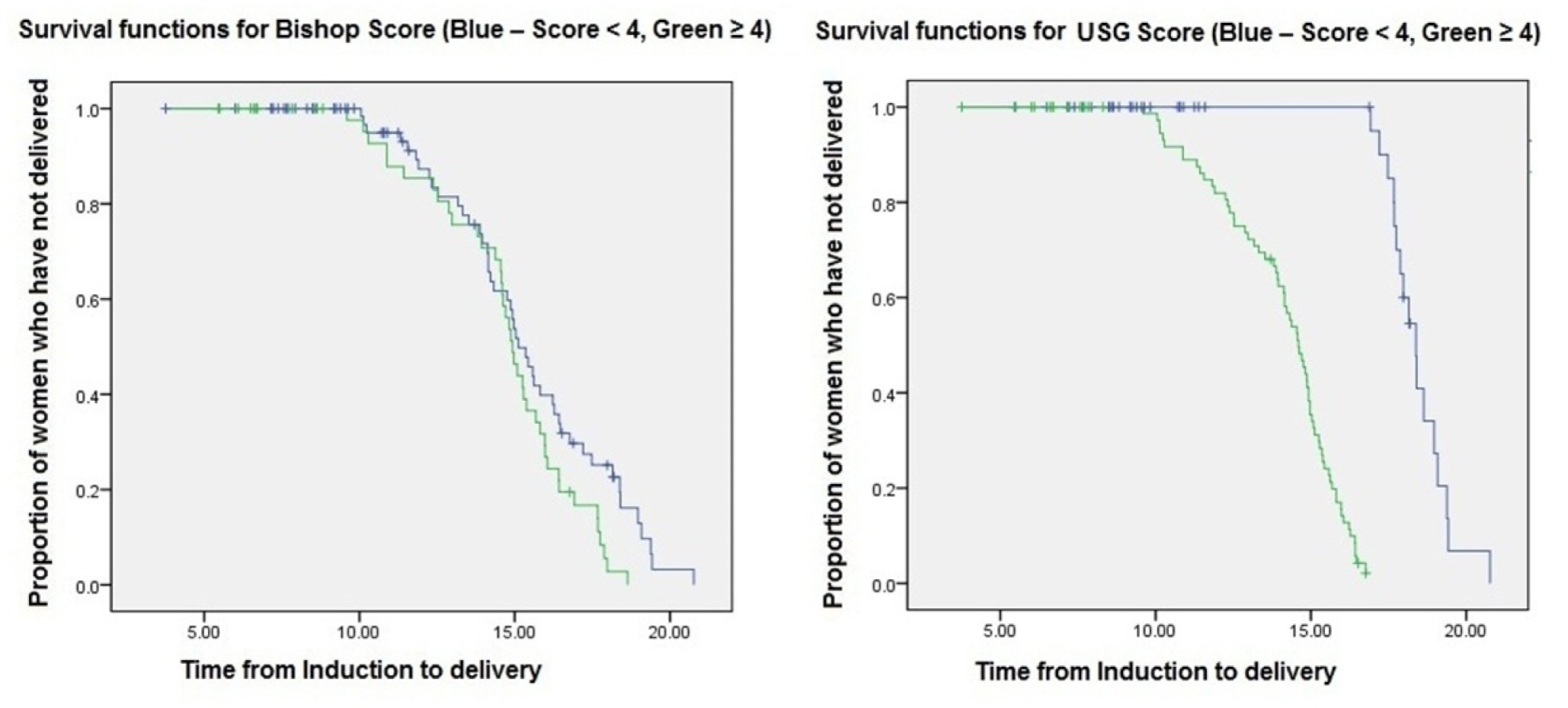
Kaplan – Meier Survival analysis showing mean duration of labour, 95% Confidential intervals for the mean and significance.
| >Mean | 95% CI | Log Rank (Mantel-Cox)chi square value | p-value |
|---|
| Bishop Score | | | 3.83 | 0.005 |
| < 4 | 15.45 | 14.7 - 16.2 |
| ≥ 4 | 14.74 | 14.03 - 15.45 |
| Manipal USG Score | | | 56.93 | <0.0001 |
| < 4 | 18.45 | 18 - 18.9 |
| ≥ 4 | 14.07 | 13.63 - 14.52 |
*Life tables are not shown, as they are lengthy and usually software generated lists
Hazard Ratio (HR) for vaginal delivery after induction of labour according to Bishop Score and USG Score using Cox proportional hazard model
| HR | 95% CI | Chi square value | p-value |
|---|
| Bishop Score | | - | | |
| < 4 | 1 | Reference | 1.45 | 0.23 |
| ≥ 4 | 1.32 | 0.84 - 2.06 |
| Manipal USG Score | | | 52.55 | <0.0001 |
| < 4 | 1 | Reference |
| ≥ 4 | 6.96 | 4.12to 11.77 |
Comparing individual ultrasound parameters to Bishop Score
| Bishop Score parameter | USG (TVS ) parameter |
| Effacement | Cervical length |
| Cervical dilatation | Funneling at internal os |
| Station | Distance of presenting part to external os |
| Position of cervix | Position ( curved / straight ) |
| Consistency | Not evaluated |
Limitations of Study
Recently many other parameters such as transperineal head distance, cervical gland area, posterior cervical angle and angle of head progression have been studied to determine successful labour. Further studies are required to know whether incorporation of these parameters in ultrasound scoring system improve the efficacy of intrapartum sonography in predicting successful induction.
Conclusion
The results of present study indicate that the use of Manipal ultrasound scoring system instead of Bishop Score for pre-induction cervical assessment is a useful tool in predicting labour outcome. Ultrasound Score of ≥ 4 demonstrates significantly higher diagnostic indices compared to Bishop Score of same magnitude.
Acknowledgement
Authors would like to thank Manipal University for the institutional grant to conduct the study.
(Score range: minimum 0, maximum 10)
(Score range: minimum 0, maximum 10)
2 components from Bishop Score (consistency and position) and one from USG Score (direction of cervical canal) were not analysed as they represented ordinal variables
*Life tables are not shown, as they are lengthy and usually software generated lists
[1]. FG Cunningham, KJ Leveno, SL Bloom, JC Hauth, DJ Rouse, CY Sponge, Labour induction. In: Cunningham FG, Williams JW, Editors. William’s Obstetrics 2010 23rd EditionNew York (NY)McGraw Hill:535-45. [Google Scholar]
[2]. PC Tan, S Suguna, N Vallikkannu, J Hassan, Ultrasound and clinical predictors for caesarean delivery after labour induction at termAust NZ J ObstetGynaecol 2006 46:505-09. [Google Scholar]
[3]. E Peregrine, P O’Brien, R Omar, E Jauniaux, Clinical and ultrasound parameters to predict the risk of caesarean delivery after induction of labourObstet Gynecol 2006 107:227-33. [Google Scholar]
[4]. Deepika G, Kumar A, Sood R, Sood A, “Prospective evaluation of clinical and ultrasonic feto-maternal parameters as predictors of caesarean delivery after induction of labour.”International Journal of Biomedical Research [Online] 2014 5(1):264-67. [Google Scholar]
[5]. EF Faltin-traub, M Boulvain, DL Faltin, P Extermann, O Irion, Reliability of the Bishop Score before labour induction at termEur J Obstet Gynecol Reprod Biol 2004 112(2):178-81. [Google Scholar]
[6]. R Gabriel, T Darnaud, N Gonzales, F Levmarie, C Quereux, Transvaginal ultrasonography of the uterine cervix before induction of labourGynecol Obstet Fertil 2001 29:919-23. [Google Scholar]
[7]. B Bueno, L San-Frutos, F Salazar, T Perez-Medina, V Engels, B Archilla, Variables that predict the success of labour inductionActa Obstet Gynecol Scand 2005 84:1093-97. [Google Scholar]
[8]. SM Rane, RR Guirgis, B Higgins, KH Nicolaides, Models for the prediction of successful induction of labour based on pre-induction sonographic measurement of cervical lengthJ Matern Fetal Neonatal Med 2005 17:315-22. [Google Scholar]
[9]. TM Eggebø, I Økland, LK Heien, P Gjessing, C Romundstad, KA Salvesen, Can ultrasound measurements replace digitally assessed elements of the Bishop Score?Acta Obstet Gynecol Scand 2009 88(3):325-31. [Google Scholar]
[10]. A Keepanasseril, V Suri, R Bagga, N Aggarwal, Pre-induction sonographic assessment of the cervix in the prediction of successful induction of labour in nulliparous womenAust N Z J Obstet Gynaecol 2007 47(5):389-93. [Google Scholar]
[11]. RK Edwards, DS Richards, Preinduction cervical assessmentClin Obstet Gynecol 2000 43(3):440-46. [Google Scholar]
[12]. PC Tan, N Vallikkannu, S Suguna, KF Quek, J Hassan, Transvaginal sonographic measurement of cervical length vs. Bishop Score in labour induction at term: tolerability and prediction of Cesarean deliveryUltrasound Obstet Gynecol 2007 29(5):568-73. [Google Scholar]
[13]. V Ware, D Raynor, Transvaginal ultrasonographic cervical measurement as a predictor of successful labour inductionAm J Obstet Gynecol 2000 182:1030-32. [Google Scholar]
[14]. S Chandra, JM Crane, D Hutchens, DC Young, Transvaginal ultrasound and digital examination in predicting successful labour inductionObstet Gynecol 2001 98(1):2-6. [Google Scholar]
[15]. L Valentin, I Bergelin, Intra- and interobserver reproducibility of ultrasound measurements of cervical length and width in the second and third trimesters of pregnancyUltrasound Obstet Gynecol 2002 20(3):256-62. [Google Scholar]
[16]. A Cubal, J Carvalho, MJ Ferreira, G Rodrigues, OD Carmo, Value of Bishop Score and ultrasound cervical length measurement in the prediction of cesarean deliveryJ Obstet Gynaecol Res 2013 39(9):1391-96. [Google Scholar]
[17]. JE Burnett, Preinduction scoring: an objective approach to induction of labourObstet Gynecol 1966 28:479-83. [Google Scholar]
[18]. G Radeka, A Novakov-miki, L Ivanovi, [The Bishop Score and induction of labour]Med Pregl 2002 55(5-6):189-94. [Google Scholar]
[19]. SR Jones, S Carley, M Harrison, An introduction to power and sample size estimationEmerg Med J 2003 20(5):453-58. [Google Scholar]
[20]. KH Park, SN Kim, SY Lee, EH Jeong, HJ Jung, KJ Oh, Comparison between sonographic cervical length and Bishop Score in preinduction cervical assessment: a randomized trialUltrasound Obstet Gynecol. 2011 38(2):198-204. [Google Scholar]
[21]. GK Pandis, AT Papageorghiou, VG Ramanathan, MO Thompson, KH Nicolaides, Preinduction sonographic measurement of cervical length in the prediction of successful induction of labourUltrasound Obstet Gynecol 2001 18(6):623-28. [Google Scholar]
[22]. SM Rane, GK Pandis, RR Guirgis, B Higgins, KH Nicolaides, Pre-induction sonographic measurement of cervical length in prolonged pregnancy: the effect of parity in the prediction of induction-to-delivery intervalUltrasound Obstet Gynecol 2003 22(1):40-44. [Google Scholar]
[23]. SH Yang, CR Roh, JH Kim, Transvaginal ultrasonography for cervical assessment before induction of labourJ Ultrasound Med 2004 23(3):375-82. [Google Scholar]
[24]. AM Gómez laencina, FG Sánchez, JH Gimenez, MS Martínez, JA Valverde martínez, VM Vizcaíno, Comparison of ultrasonographic cervical length and the Bishop Score in predicting successful labour inductionActa Obstet Gynecol Scand 2007 86(7):799-804. [Google Scholar]
[25]. AS Hatfield, L Sanchez-ramos, AM Kaunitz, Sonographic cervical assessment to predict the success of labour induction: a systematic review with metaanalysisAm J Obstet Gynecol 2007 197(2):186-92. [Google Scholar]
[26]. H Roman, E Verspyck, L Vercoustre, Does ultrasound examination when the cervix is unfavourable improve the prediction of failed labour induction?Ultrasound Obstet Gynecol 2004 23(4):357-62. [Google Scholar]
[27]. JL Bartha, R Romero-Carmona, P Martínez-del-fresno, R Comino-delgado, Bishop Score and transvaginal ultrasound for preinduction cervical assessment: a randomized clinical trialUltrasound Obstet Gynecol 2005 25:155-59. [Google Scholar]
[28]. HP Dietz, V Lanzarone, JM Simpson, Predicting operative deliveryUltrasound Obstet Gynecol 2006 27(4):409-15. [Google Scholar]
[29]. CJ Verhoeven, A Oudenaarden, MA Hermus, MM Oei, BW Mol, Validation of models that predict Cesarean section after induction of labourUltrasound Obstet Gynecol 2009 34(4):316-21. [Google Scholar]