Odontogenic Myxoma of the Maxilla- A Rare case Report
Ramkumar Subramaiam1, Sangeetha Narashiman2, Malathi Narasimhan3, Veda Giri4, Santhosh Kumar5
1 Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, Sri Ramachandra University, Ramachandra Nagar, Porur- Chennai, Tamilnadu, India.
2 Senior Lecturer, Department of Oral and Maxillofacial Pathology, Faculty of Dental Sciences, Sri Ramachandra University, Porur- Chennai, Tamilnadu, India.
3 Professor and Head, Department of Oral and Maxillofacial Pathology, Faculty of Dental Sciences, Sri Ramachandra University, Porur- Chennai, Tamilnadu, India.
4 Associate Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, Sri Ramachandra University, Porur- Chennai, Tamilnadu, India.
5 Reader, Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, Sri Ramachandra University, Porur- Chennai, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. N. Sangeetha, Senior Lecturer, Department of Oral and Maxillofacial Pathology, Faculty of Dental Sciences, Sri Ramachandra University, No 1, Ramachandra Nagar, Porur- Chennai-600116, Tamilnadu, India. E-mail : sangeetha_narashiman@yahoo.co.in
Odontogenic myxoma (OM) is an uncommon, benign, locally invasive, non-metastasizing neoplasm arising from the odontogenic ectomesenchyme that usually occurs in the tooth bearing areas of the jaws. These lesions arouse special interest as they pose high diagnostic challenge. Here, we present a rare case of OM of the maxilla in an 18-year-old male. The clinical, radiographic and histopathological features of the lesion are discussed in this paper.
Ectomesenchyme, Myxoid stroma, Neoplasm
Case Report
An 18-year-old male patient reported to the outpatient department of oral and maxillofacial surgery three years ago with a painless swelling in the left side of the face for the past four years which gradually increased in size. Nasal obstruction was the only presenting symptom. His past medical history and family history were not significant. On extra oral examination a diffuse bony hard, non-tender swelling measuring 8 x 7 cms in the left side of the face extending supero-inferiorly from the infraorbital ridge to the corner of the mouth and anterioposteriorly from the midline to 2cm anterior to the tragus was noted. The nasobuccal fold was obliterated [Table/Fig-1]. The skin over the swelling was normal in colour and the left lower eyelid was pushed upwards. Intraoral examination revealed a 5x4 cm swelling of the left maxillary alveolus extending from 24 to 28 regions. The upper left second premolar (25) was missing [Table/Fig-2]. The teeth associated with the swelling- 26, 27 & 28 were mobile.
Photograph showing a diffuse extra oral swelling over the left maxilla obliterating the nasobuccal fold and pushing the lower lid upwards

Photograph showing the intra oral mass extending from the left upper first premolar to the maxillary tuberosity

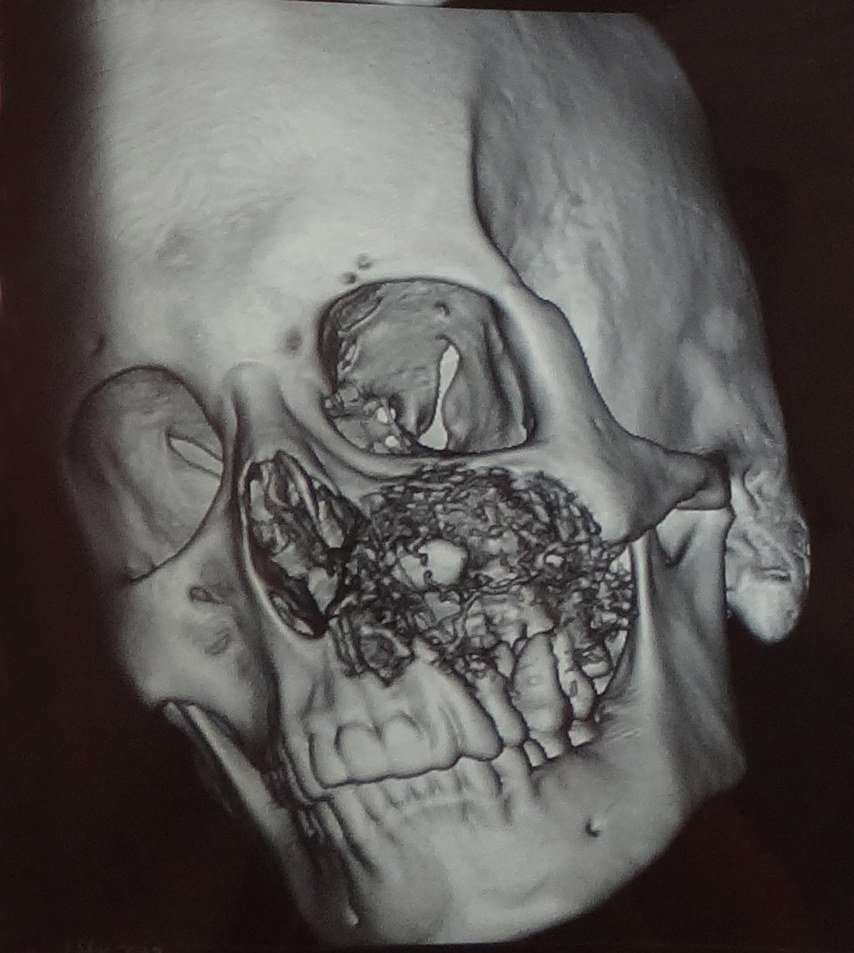
Investigations: Orthopanthomogram of the jaws revealed mixed radiolucency and radio opacity associated with impacted 25 within the maxillary sinus [Table/Fig-3]. Computed tomography of the region showed a hypodense lesion with irregular sclerotic thinned out margins extending from the maxillary left alveolus to the infraorbital rim obliterating the entire maxillary sinus. Destruction of the medial and lateral margins of the maxillary antrum along with partial occlusion of the nasal passage was also evident [Table/Fig-4]. Erosion of the medial and anteriolateral wall of the maxillary sinus was evident in the 3D reconstruction model of the CT images [Table/Fig-5]. Blood investigations showed serum calcium, phosphorus, magnesium and alkaline phosphatase within normal limits with a clinical differential diagnosis of AOT, ossifying fibroma, fibrous dysplasia and peripheral gaint cell granuloma an incisional biopsy was performed. Histopathological examination of the tissue showed spindle shaped cells in a loose myxomatous background suggestive of odontogenic myxoma [Table/Fig-6].
Orthopanthomograph showing haziness of the left maxillary sinus with imapacted 25

Computed tomographic image showing obliteration of the maxillary sinus with thinning out of the margins

3D reconstruction of the computed tomogram depicting the erosions of the medial and anterolateral wall of the maxillary sinus
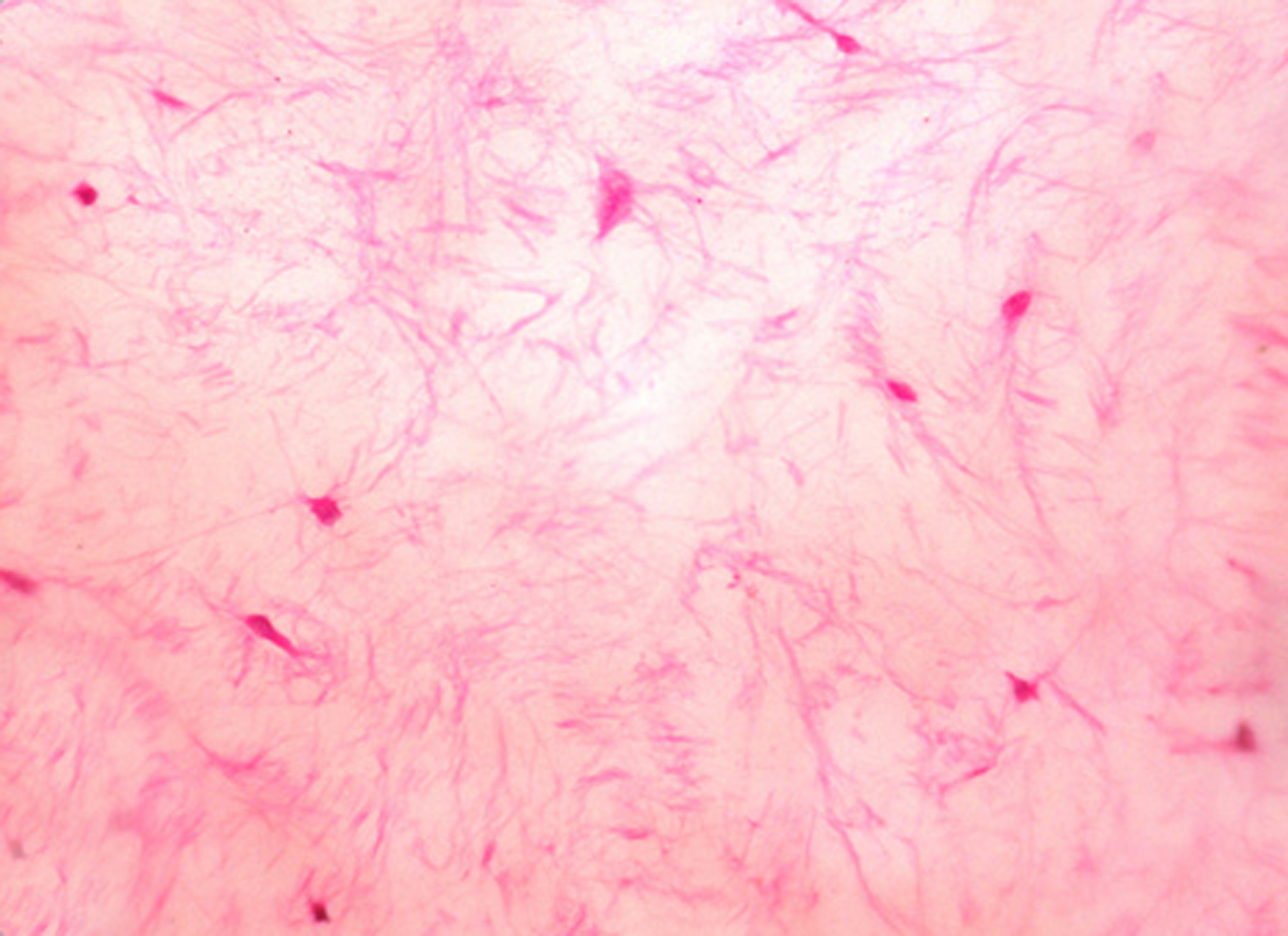
Loosely arranged spindle shaped and stellate cells in a myxoid stroma. H and E X40
Left maxillectomy was planned for the patient and under general anesthesia the tumour was exposed through a Weber Ferguson incision extraorally and left intra oral upper vestibular incision from 21 to 26 region. Osteotomy was performed around the encapsulated mass with a 1centimeter clearance. Left maxillectomy was done and hemostasis achieved [Table/Fig-7]. The residual defect on the left side of the maxillary region was covered with a prefabricated obturator and wound was closed. Postoperatively the healing was uneventful and under regular follow ups of every 3 months no recurrence has been noted in two and half years [Table/Fig-8].
Intra operative photograph showing the well encapsulated tumor mass

Extraoral view one month post surgery

Histopathology: The excised specimen was greyish white lobulated mass measuring 7 x 8cms in dimension. The impacted 25 was projecting out from the excised mass [Table/Fig-9]. On gross examination the cut surface of the specimen was glistening with a gelatinous substance oozing out.
Gross specimen showing a greyish white lobulated mass with impacted 25 projecting out. Glistening cut surface of the specimen with a gelatinous substance oozing out

The hematoxylin and eosin stained sections of the excised specimen showed classic features of odontogenic myxoma consisting of loosely arranged spindle shaped and stellate cells with long fibrillar processes in a background of myxomatous stromal tissue. Occasional islands of odontogenic islands were appreciated [Table/Fig-10a&b]. Mixed areas of prominent collagen component and myxoid stroma were appreciated. However, a clear demarcation was noted between the collagenous and myxoid stroma [Table/Fig-11]. Occasional Islands of odontogenic epithelial cells, few areas of lipomatous differentiation and osteoid formation were also noted. [Table/Fig-12].
Loosely arranged spindle shaped and stellate cells with long fibrillar processes in a background of myxomatous stromal tissue H and E X40

Occasional presence of Odontogenic rests. H and E X10

Mixed areas of prominent collagen and myxoid areas with clear demarcation H and E X40

Well demarcated lesion with areas of osteoid formation and overlying peripheral epithelium. H and E X4

Discussion
Myxomas of the jaws are relatively uncommon benign odontogenic neoplasms which are locally destructive [1]. In 1863, Virchow coined the term which he later in 1871 defined as “Schleimgesch-Wulste” meaning ‘Myxomata” as he considered only about soft tissue myxomas. Odontogenic myxoma (OM) of the jaws was first described by Thoma and Goldman in 1947 [2]. OM is classified as a tumour of odontogenic mesenchyme with or without the presence of odontogenic epithelium (Latest WHO classification) [3]. Head and neck Myxomas are classified into facial bone derived and soft tissue derived myxomas. OM falls under the first category and exclusively occurs in the maxilla mandibular complex [4].
The histogenesis of this tumour is controversial, however the WHO have postulated that myxomas occurring in the jaws originate from the odontogenic apparatus owing to the following reasons: 1) The site of occurrence, which is commonly the tooth bearing areas of the jaws. 2) Its occurrence in young adults and association with unerupted or missing teeth. 3) The occasional presence of odontogenic epithelial islands in the tumour and the histopathological appearance of the tumour wherein it resembles the dental mesenchyme [5]. An alternate hypothesis stating the origin of OM from modified fibroblasts of the tooth germ has been suggested by Moshiri et al., [6].
These lesions most frequently occur in the second and third decade of life. Mandible is slightly affected more than maxilla. Lesions involving the maxilla are very aggressive and usually involve the maxillary sinus. This case is much rarer because maxillary OMs in men are the least prevalent accounting for 29.2%. Though these lesions are asymptomatic nasal obstruction, exopthalmus and occasional perforation of the medial and lateral walls of the sinus may be noted in lesions of longer duration [7].
Though the radiological picture of OMs widely varies among lesions from purely radiolucent to mixed lucent and opaque to complete radiopacity, almost all the lesions involving the maxillary sinus were radiopaque. A CT scan or a MRI is often advised to learn the extent of involvement of the lesions and to assist in diagnosis. Zhang et al., reviewed conventional radiographs of 41 cases of OM and divided its radiographic features into 6 types [Table/Fig-13]. OMs are usually associated with a missing or unerupted tooth; however our case exhibited an impacted first premolar within the maxillary sinus. The radiological differential diagnoses of these lesions include odontogenic fibroma, ameloblastoma, ameloblatic fibroma, fibrous dysplasia, dentigerous cyst, central gaint cell granuloma, intraosseous hemangioma, odontogenic keratocyst and dentigerous cyst [8].
Radiographic classification of Odontogenic Myxoma. Zhang et al., 8]
| Type | Radiographic Pattern | Percentage of Occurence |
|---|
| Type I | Unilocular Radiolucency | 17% |
| Type II | Multilocular Radiolucency | 29% |
| Type III | Lesion involving the alveolar bone | 5% |
| Type IV | Lesion involving the maxillary sinus | 22% |
| Type V | Osteolytic destruction | 7% |
| Type VI | Mixed areas of osteolytic destruction and osteogenesis | 20% |
Histologically, OMs comprise of spindle cells in a highly myxomatous background. The undifferentiated mesenchymal cells from which the tumour originates, is capable of differentiating into spindle cells, fibroblasts, lipocytes and osteocytes thereby accounting to the presence of collagen, fat and ostoid within the tumour component. The propotion of these components in the neoplasm depend upon the differentiation pattern of the mesenchymal cells [9]. Microscopically these lesions should be differentiated from chondromyxoid fibroma and myxoid nerve sheath tumour [10]. At times areas of myxoid degeneration in fibrosarcoma, chondrosarcoma and liposarcoma can also be mistaken for OM [11]. Our case had equal proportions of well demarcated myxoid and collagenous areas along with lipomatous and osteoid differentiation. Histochemically the ground substance of OMs comprises 80% of hyaluronic acid and 20% of Chondroitin sulfate [4].
The treatment of OMs depends on the size, nature and behaviour of these lesions and varies from simple surgical curettage, peripheral ostectomy to segmental resection of the involved bones. Radical resection is the treatment of choice for the most aggressive tumours. Lack of encapsulation and Infiitration of myxomas into adjacent tissues and marrow spaces makes complete surgical curettage of these lesions a highly difficult task. The lesion in the reported case was considerably large and involved the maxillary sinus and thus partial maxillectomy was the preferred treatment. The recurrence rate of these lesions is very high (25%) especially in the first two years after surgical curettage and reconstruction of the surgical defect in these cases should be delayed for the same reason [11].
According to English literature OMs represents 3 to 6% of all odontogenic tumours. The rarity of these lesions along with its resemblance to various other odontogenic and non odontogenic pathology both clinically and radiographically has resulted in high diagnostic dilemmas [12]. Final diagnosis is usually made by histopathological evaluation. In our case the diagnosis was arrived with the incisional biopsy specimen that aided in planning the treatment appropriately.
Conclusion
We have reported a rare case of maxillary Odontogenic myxoma in an 18-year-old male. These lesions are usually slow growing benign neoplasms. But OMs can turn out to be aggressive and locally invasive. Due to its unspecific nature, a sound knowledge of this lesion with proper correlation of clinical, radiological and histopthological findings is a prerequisite to prevent over diagnosis and to treat these patients appropriately. Resection with wide margins is the treatment of choice and follow-up during the first two years postoperatively is highly recommended as this is the period of highest reported recurrences
[1]. Rajendran R, Sivapathasundaram B, Shafer’s Textbook of Oral Pathology 2006 5th edNew DelhiElsevier [Google Scholar]
[2]. Vijeev V, Usha MD, Manjunath V, Odontogenic myxoma of the maxilla: A report of unusual pediatric caseInt Journal of Clinical Pediatric Dentistry 2011 4(3):264-68. [Google Scholar]
[3]. Reichart PA, Philipsen HP, Odontogenic Tumours and Allied Lesions 2004 LondonQuintessence Publishing Co Ltd:188-19. [Google Scholar]
[4]. Sasidhar S, Sangeetha PW, Rajkumar N P, Odontogenic myxoma of the maxilla: A report of a rare case and review of the literatureJ Oral Maxillofac Pathol 2010 14(1):19-23. [Google Scholar]
[5]. Allan UC, Sérgio B, Paulo H, Maxillary odontogenic myxoma involving the maxillary sinus - Case reportRev Bras Otorrinolaringol 2008 74(3):472-75. [Google Scholar]
[6]. Moshiri S, Oda D, Worthington P, Myall R, Odontogenic myxoma: Histochemical and ultrastructural studyJ Oral Pathol Med 1992 21:401-43. [Google Scholar]
[7]. Sivakumar G, Kavitha B, Saraswathi TR, Sivapathasundharam B, Odontogenic myxoma of the maxillaIndian J Dent Res 2008 19:62-65. [Google Scholar]
[8]. Zhang J, Wang H, He X, Radiographic examination of 41 cases of odontogenic myxomas on the basis of conventional radiographsDentomaxillofacial Radiology 2007 36:160-67. [Google Scholar]
[9]. Rakesh KM, Venkata SK, Venkata S, OdontogenicMyxoma of the MandibleCase Reports in Dentistry 2012 2012Article ID 214704, 4 pages [Google Scholar]
[10]. Arul AJ, Verma S, Arul AJ, Verma R, Infiltrative odontogenic myxoma of the posterior maxilla: Report of a caseJ Nat Sc Biol Med 2013 4:484-87. [Google Scholar]
[11]. Ajaz S, Parveen L, Suhail L, Odontogenic myxoma of the maxilla: A report of a rare case and review on histogenetic and diagnostic conceptsNatl J Maxillofac Surg 2011 2(2):189-95. [Google Scholar]
[12]. Reddy SP, Naag A, Kashyap B, Odontogenic myxoma: Report of 2 casesNatl J Maxillofac Surg 2010 1:183-86. [Google Scholar]