Multiple Adverse Effects of Systemic Corticosteroids: A Case Report
Divya Satyanarayanasetty1, Kavitha Pawar2, Pratibha Nadig3, Almelu Haran4
1Post Graduate, Department of Pharmacology, Vydehi Institute of Medical Sciences & Research Centre, Bangalore, India.
2Technical Associate, Pharmacovigilance Unit, Vydehi Institute of Medical Sciences & Research Centre, Bangalore, India.
3Professor, Department of Pharmacology, Head, Pharmacovigilance Unit, Vydehi Institute of Medical Sciences & Research Centre, Bangalore, India.
4Professor and Head, Department of Pulmonary Medicine, Vydehi Institute of Medical Sciences & Research Centre, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratibha Nadig, 224, 4th Main, BEL 6th Block, Vidyaranyapura, Bangalore-560097, India.
E-mail: drpratibhanadig@yahoo.co.in
Corticosteroids are among the effective treatments available for many medical conditions. Adverse effects such as osteoporosis, cataract and muscle weakness are widely recognized on long term administration and have considerable public health implications. Many reports are available that have dealt with individual adverse effects.Here, we report a case of a 55-year-old female, with systemic glucocorticoid induced bilateral cataract, osteoporosis, diabetes mellitus and hypothalamic pituitary axis (HPA) suppression. These were induced through self –medication. She presented to the hospital for the treatment of acute exacerbation of bronchial asthma.
Diabetes mellitus, Hypothalamic pituitary axis (HPA), Osteoporosis, Self–medication
Case Report
A 55-year-old female patient presented to the emergency unit with a history of severe breathlessness, productive cough with scanty white sputum and early morning wheeze since two days.
Patient was a known asthmatic since 30 years. Past history revealed that eight years back she was prescribed tablet betamethasone, 10 mg once a day for an attack of severe asthma, for 10 days. Since she had recovered with the treatment, she continued with the same medication without a prescription for eight years, as and when required.
She was diagnosed of diabetes mellitus seven years back and was on oral hypoglycemic medications. She was a non-alcoholic and non-smoker, working in a flour mill. The patient was hospitalized on the same day. The general physical examination revealed bilateral cataract which the physician diagnosed as steroid-induced cataract.The respiratory system examination showed airway restriction. All other systems were normal.
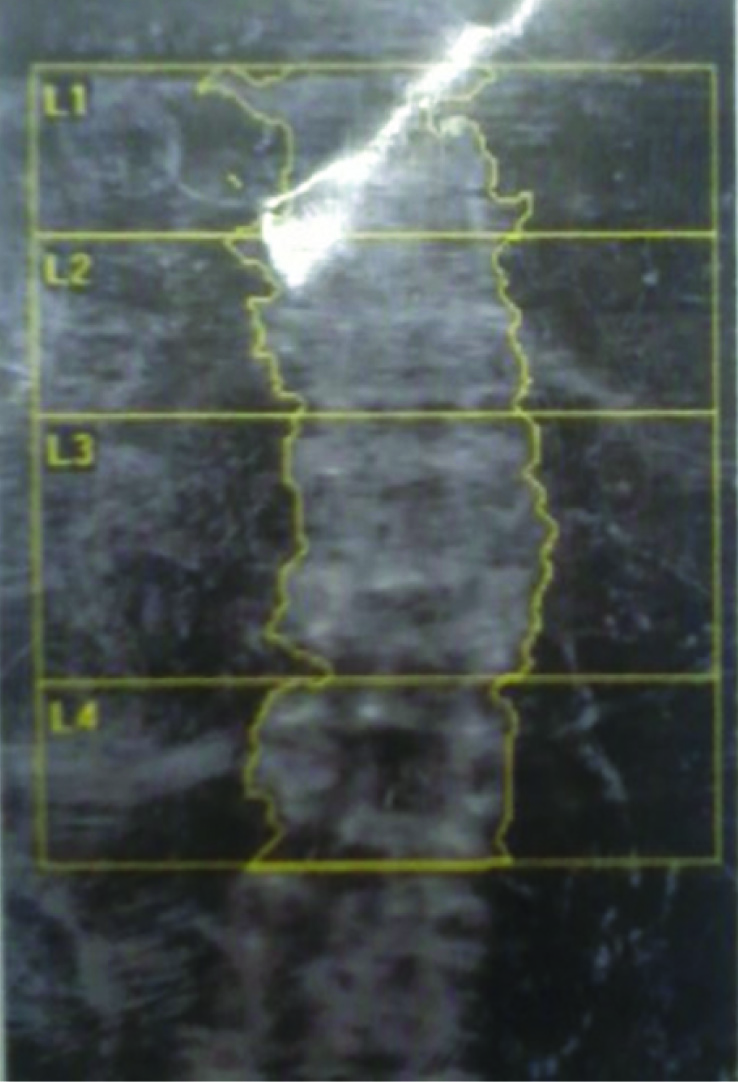
Laboratory investigations were done as shown in [Table/Fig-1]. A 2D echo showed ejection fraction as 65%. Pulmonary function test showed moderate restriction and small airway narrowing. Osteoporosis was seen on dexa bone scan as shown in [Table/Fig-2]. After all the above investigations, the patient was found to have uncontrolled diabetes mellitus, low serum cortisol levels, osteoporosis on bone mineral density scan. Physician concluded the condition as steroid induced -diabetes mellitus, osteoporosis, HPA axis suppression and cataract.
The following treatment was initiated: Salbutamol+Budesonide nebulization 8th hourly, single intravenous injection of Zolindronate 5mg/100ml, tab Calcium and Vitamin D twice daily, inj. regular Human Insulin 16U-18U-8U, inj. Glargine 0-0-14U, inj. Hydrocortisone 100mg twice daily, capsule Acebrofylline 100mg, capsule Pantoprazole 40 mg once a day.
On the 8th day patient was discharged as she was stable. All the vitals were within normal limits and the investigations were in the normal range. She was advised salt restriction, diabetic diet, and continued the ongoing treatment except for nebulization and injection hydrocortisone. Instead, metered dose inhaler Fluticasone propionate 250 mcg with spacer two puffs-twice daily and Tab Prednisolone 10mg on tapering dose for 40 days was advised. She was instructed to strictly follow the prescription and not to self-medicate in any situation. It was highlighted during counselling that her present condition was mainly because of self-medication. She was asked to come for follow up after 10 days. However, patient did not come for follow up.
Discussion
A wide range of adverse effects of oral corticosteroids have been documented. Increased risk of fracture, cataract, suppression of the hypothalamo- pituitary-adrenal (HPA) axis, diabetes, flaring up of latent infections such as tuberculosis, peptic ulcer are some of the reported complications of long term use of glucocorticoids in various publications [1].
As per GINA guidelines, oral corticosteroids are recommended only in moderate or severe attack of asthma to reverse the inflammation and for early recovery [2]. When used for a limited duration the adverse effects are minimal. Long term control is brought about by inhaled steroids and beta two agonists. The ease of administration, cost and easy accessibility of oral corticosteroids has probably prompted the patient to self- medicate that resulted in multiple adverse effects.
Of the four adverse effects HPA suppression as diagnosed by low serum cortisol was definitely related to the long term use of medication. HPA suppression is reported with inhaled, topical as well as oral. The literature search revealed very few reports of HPA suppression with oral use. A case control study, by Mortier et al., has shown that people prescribed an oral or inhaled corticosteroid are at a dose related increased risk of adrenal insufficiency [3]. A prospective study after oral corticosteroid therapy in patients with rheumatoid arthritis, by Jasani et al., showed a significant suppression of HPA axis as manifested by diminished plasma 11- OH-CS responses to insulin induced hypoglycemia [4]. It has been reported that administration of 7.5 mg of prednisolone or more for three weeks results in decreased CRH, ACTH and Cortisol secretion. Exogenous glucocorticoids exert negative feedback in the same manner as endogenous cortisol, leading to the suppression of cortisol production and, subsequently, adrenal insufficiency.The serum cortisol levels were significantly low, in the indexed patient, indicating the suppression of adrenal secretion.
Steroids can induce cortical and posterior sub capsular cataract. The incidence of steroid induced cataract is estimated to be 22% [5]. The mechanism of corticosteroid-induced cataract is not fully established. However, some probable mechanisms proposed include osmotic imbalance, oxidative damage, disrupted lens growth factors [6,7].
Osteoporosis is a commonly reported complication on long term steroid use. The patient, being an elderly post-menopausal female, osteoporosis is a common finding. Steroid must have further aggravated the disease. The bone densitometry demonstrated osteoporosis with high risk factor for fracture. The probable mechanisms explained for glucocorticoid induced osteoporosis are inhibition of calcium absorption from the gastrointestinal tract, the renal tubular Calcium reabsorption and the replication of osteoblasts in the bone [8,9].
Chronic metabolic effects of corticosteroids of increased gluconeogenesis & glycogen synthesis eventually lead to the development of diabetes [10]. Considering the rising prevalence of diabetes in India, once again it appears that both age and steroids must have contributed in the development of diabetes.
Laboratory parameters on chronic use of corticosteroids
| Serial No. | Investigations | Values |
|---|
| 1 | Haemoglobin | 13.20 g/dL |
| 2 | White blood cells | 7370cells/μL |
| 3 | Thyroid stimulating hormone | 2.64 mU/L |
| 4 | Blood urea | 17.1 mg/dl |
| 5 | Blood creatinine | 0.45mg/dL |
| 6 | IgE | 235 IU/mL |
| 7 | Alkaline phosphatase | 70IU/L |
| 8 | Serum cortisol | 0.13 nmol/L |
| 9 | Sputum AFB | Negative |
| 10 | Serum Calcium | 9.4mg/dL |
| 11 | Serum Phosphorus | 3.4 mg/dL |
Vertebral bone dexascan showing osteoporosis
Conclusion
We would like to conclude that, while HPA suppression was a direct adverse reaction to corticosteroid, the development of cataract, diabetes and osteoporosis might have been either a direct toxic effect or indirect effects where the drug must have accelerated their development as a risk factor.
This case report warns us the need for accurate dosing and tapering while administering oral corticosteroids. Patient education addressing the adverse effects and importance of follow up plays a vital role in minimizing such adverse effects. Lack of awareness about hazards of Self-medication lead to serious adverse reactions as seen in this patient.
[1]. Boushey Homer A, Drugs used in Bronchial Asthma. In: Laurence LB, Bruce AC, Bjornn CK, editors. Basic and clinical Pharmacology 2009 11th EditionUSAMcGraw Hill:339-55. [Google Scholar]
[2]. Global initiative for asthma (Internet).2011(updated 2011;cited 2014 March 14). Available from http://www.ginasthma.org/local/uploads/files/GINA_Pocket_April20_1.pdf Accessed on 30th May 2014 [Google Scholar]
[3]. KJ Mortier, LJ Tata, CJ Smith, J West, TW Harrison, AE Tattersfield, Oral and Inhaled corticosteroids and adrenal insuffiency: a case-control studyThorax 2006 61(5):405-08. [Google Scholar]
[4]. KM Jasani, JA Boyle, J Williamson, AK Taylor, WW Buchanan, Corticosteroiinduced hypothalamo-pituitary-adrenal axis suppression.Prospective study using two regimens of corticosteroid therapyAnn Rheum Dis 1968 27(4):352-59. [Google Scholar]
[5]. L David, DL Veenstra, HJ Best, SD Sullivan, DE Hricik, Incidence and long-term cost of steroid-related side effects after renal transplantationAmerican Journal of Kidney Diseases 1999 33(5):829-39. [Google Scholar]
[6]. R Viviane, MP Adriana, RA Cristiane, D Adriana, AA Fernando, Posterior subcapsular cataract in patients with pemphigus and pemphegoid using oral corticosteroidAn bras Dermatol 2004 79(5):539-45. [Google Scholar]
[7]. AI Jobling, RC Augusteyn, What causes steroid cataracts? A review of steroidinduced posteriorsubcapsular cataractsClin Exp Optom 2002 85:61-75. [Google Scholar]
[8]. S Huybers, TH Naber, RJ Bindels, JG Hoenderop, Prednisolone-induced Ca2+ malabsorption is caused by diminished expression of the epithelial Ca2+ channel TRPV6Am J Physiol Gastrointest Liver Physiol 2007 292:G92-97. [Google Scholar]
[9]. G Mazziotti, A Angeli, JP Bilezikian, E Canalis, A Giustina, Glucocorticoid induced osteoporosis: an updateTrends Endocrino Metab 2006 7:144-49. [Google Scholar]
[10]. KD Tripathi, Insulin, Oral Hypoglycemic Drugs and Glucagon. In: M Tripathi, editor. Essentials of Medical Pharmaclogy 2013 7th EditionNew DelhiJaypee Publishersl:258-81. [Google Scholar]