Novel Use of PRF and PDT in the Management of Trauma Induced Root Resorption and Infrabony Defect
Preeti Jain Pruthi1, Neha Yadav2, Ruchika Roongta Nawal3, Sangeeta Talwar4, Arundeep Kaur Lamba5
1 Senior Resident, Department of Conservative Dentistry & Endodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
2 Senior Resident, Department of Periodontics and Oral Implantology, Maulana Azad Institute of Dental Sciences, Delhi, India.
3 Associate Professor, Department of Conservative Dentistry & Endodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
4 Professor and Head, Department of Conservative Dentistry & Endodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
5 Professor and Head, Department of Periodontics and Oral Implantology, Maulana Azad Institute of Dental Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Preeti Jain, Senior Resident, Department of Conservative Dentistry & Endodontics, 3rd Floor, Maulana Azad Institute of Dental Sciences, MAMC complex, Bahadur Shah Zafar Marg, Delhi- 110002, India. Email: drpreetijain82@gmail.com
Root resorption is a common squeal of traumatic injury to the dentition. Its progression can be minimized by early diagnosis and appropriate treatment. This case report presents the diagnosis and management of a case of trauma induced trio of apical root resorption, intraradicular root resorption and infrabony defect in maxillary central incisor. The main aim in treating such cases of resorption is to limit the inflammatory response at the periapical region so as to halt the resorptive process. To allow faster regeneration of the periodontal tissues, Platelet rich fibrin (PRF), a second generation platelet concentrate was used as an apical matrix over which MTA plug was given. The periodontal defect was managed with the help of localized antimicrobial photodynamic therapy (aPDT).
Cone beam computed tomography, MTA, Resorptive defect
Case Report
An 18-year-old male patient reported to the Department of Conservative dentistry, Maulana Azad Institute of Dental Sciences, New Delhi, India with a chief complaint of fractured and mobile upper left central incisor. Medical history was noncontributory but there was a history of trauma to maxillary anterior region 6 months back and a subsequent visit to a local dentist for the same. Clinical examination revealed a grade 1 mobile maxillary left central incisor with an open access to the root canal and an infrabony defect on the mesiopalatal aspect. Radiographic examination showed an irregular radiolucent lesion in the apical third of the root canal of maxillary left central incisor [Table/Fig-1]. The lesion gave a classical appearance of internal resorption but due to its irregular shape and questionable involvement of the external root surface, a confirmatory diagnosis was necessary for which a CBCT scan was done. The scan revealed a periapical lesion and an internal resorptive defect in the apical third of the canal [Table/Fig-2]. A separate resorption area on the distal external surface of the root in the apical region was also present [Table/Fig-2]. Based on these findings; endodontic treatment (for the intracanal and periradicular pathosis) along with periodontal therapy (for the infrabony defect) was planned. The distal external surface resorption was kept under observation.
Pre-operative intraoral periapical radiograph showing an irregular radiolucent lesion in the apical third of the root canal of maxillary left central incisor

Cone beam computed tomography scan showing the defect in three dimensions (defect marked)

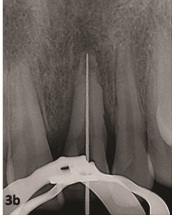
After applying rubber dam, access to the root canal system was gained and working length was determined under operating microscope [Table/Fig-3a&b]. The canal was thoroughly cleaned and prepared along with copious irrigation using sodium hypochlorite and calcium hydroxide paste dressing was placed in the canal for one week.
Access opening in maxillary left central incisor under operating microscope

Working length determination
In tandem with the endodontic treatment periodontal therapy was also initiated. A probing depth of 8 mm and 6mm were present on the mesiopalatal and distopalatal aspect respectively, along with bleeding on probing [Table//Fig-4&b].The periodontal therapy rendered was mechanical non surgical pocket therapy comprising of supragingival and subgingival scaling and root planning performed by hand instruments and ultrasonic instruments. The patient was placed on self-performed supragingival plaque-control measures, and advised to brush twice daily for 3 min using modified Bass technique and instructed to rinse twice daily for 1 min with10 ml of 0.2% chlorhexidine solution for 4 wk.
Measurement of probing depth at Mesiopalatal aspect

Measurement of probing depth at Distopalatal aspect

Antimicrobial photodynamic therapy (aPDT) was done 2 wk after periodontal therapy by injecting photo sensitizer dye (Helbo-Blue, Helbo Photodynamic Systems, Austria) in the pocket using a syringe.The dye was left for 3 min and then irrigated with normal saline to wash off the excess. All four surfaces; facial, palatal, mesial and distal were irradiated with diode laser with fiber optic tip with wavelength of 670 nm with a power density of 75mW/cm2 for 1 min each [Table/Fig-5a,b].
Introduction of the photo sensitizer dye in the defect

Application of the beam of light with diode laser

In the subsequent visit, the PDT was repeated using the same method amounting to a total of PDT being performed twice. The intracanal dressing was replaced with triple antibiotic paste and the patient was recalled after four weeks.
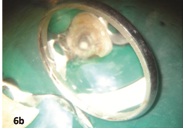
On the recall appointment the canal was rinsed and cleaned of all the contents.For accelerated healing of the periapical lesion; PRF in the apical area through the root canal was planned. Immediately before obturation, PRF was freshly prepared. Eight ml of intravenous blood was drawn in a 10-ml sterile tube without anticoagulant and centrifuged at 2700 revolutions per minute for 12 min. PRF, which lies as a structured fibrin clot in the middle of the tube, just between the red corpuscles at the bottom and acellular plasma at the top, was collected from the tube using a sterile tweezer and scissors and then introduced in the canal. With the help of a finger plugger, it was pushed into the periapical region [Table//Fig-6a]. The apical plug of MTA was placed in the apical third of the root to completely fill the resorptive defect [Table//Fig-6b]. A cotton pellet and intermediate restorative material were used to close the access opening and the patient was recalled after 2 days. Next visit included complete backfilling of the root canal using GuttaFlow (Coltene/Whaledent, Langenau, Germany) and sealing of the coronal access using a light cure composite restoration. Postoperative radiograph was taken to check the obturation [Table/Fig-7]. The patient was advised to visit after a month for follow up.
Introduction of platelet rich fibrin through the root canal (appreciable at the apex when compared to [Table/Fig-3a]).

Formation of mineral trioxide aggregate plug
Immediate post-obturation radiograph showing the complete obturation of the resorptive defect and the rest of the canal

In the recall visit, pocket probing depth (PPD) was found to be reduced to 4 mm and 3 mm at mesiopalatal and distopalatal aspect of the tooth respectively and there was absence of bleeding on probing. The follow up radiographs after 6, 12 and 18 months revealed progressive healing as compared to preoperative radiograph and significantly reduced tooth mobility [Table/Fig-8,9,10].
Follow up radiograph at 6 months

Follow up radiograph at 12 months

Follow up radiograph at 18 months

Discussion
Tooth resorption is one of those evasive, nebulous, poorly-understood processes that can cause a lot of frustration and confusion amongst both patients and providers. In the cases of trauma induced external resorption, the root cementum and dentin are resorbed, and bone resorption follows. There is crater formation on the resorbed apex, deforming the root apex surface, and consequently, loss of apical constriction.
Successful management of the root resorption involves an accurate diagnosis and insight knowledge of the various etiological factors [1]. Conventional intraoral radiography produces images that have objects superimposed upon each other. Cone beam computed tomography (CBCT) is a new and innovative technology that provides us with the relevant information that cannot be obtained from conventional radiography especially in the detection of resorption lesions [2,3].
Management of internal root resorption defects places a great emphasis on the chemical dissolution of the vital and necrotic pulp tissue. Thorough irrigation using sodium hypochlorite followed by calcium hydroxide dressing has been shown to have an additive effect in completely cleaning the canal [4]. Moreover, triple antibiotic paste helps in sterilization of canals and healing of periapical pathology [5].
PRF is a fibrin matrix in which platelet cytokines, growth factors, and cells are embedded.The rationale behind the use of this platelet concentrate was to provide an accelerated healing and an internal matrix against which, MTA could be condensed which is the material of choice to seal such defects as it is biocompatible, bioactive, and well tolerated by periradicular tissues [6].
In a similar case of a maxillary lateral incisor with advanced perforating internal root resorption in the middle third of the root, Eduardo N et al., used MTA to fill the resorption area after conventional root canal therapy of the apical segment. They found that at the follow-up after 11 years and 8 months, the patient was clinically asymptomatic and the radiographic examination and computerized tomography indicated periodontal bone repair [7].
To achieve a three dimensional filling of the resorption defect, MTA plug was used in the apical area [8] and the rest of the canal was backfilled using GuttaFlow which is non-heated, flowable gutta-percha that, unlike heated gutta-percha, does not shrink [9].
PDT was used as an adjuvant for its anti microbial effect. The photo-sensitizer used links to the pathogens. Under a light of appropriate wavelength,it reacts with oxygen to produce highly reactive singlet oxygen. The singlet oxygen interacts with biological substrates causing oxidative damage and lethal effects on the bacterial cell. It has short life and short radius of action, thus minimizing the damage to adjacent tissues [10]. BOP along with PPD has the greatest accuracy to predict future attachment loss [11]. In this case there was a gain in attachment level with reduction in PPD and absence of BOP.
Conclusion
Though many conventional methods of treating root resorption are available, the advantage of using the present approach has been that PRF and MTA are excellent healing biomaterial allowing faster healing and similarly a PDT significantly promoted bony healing.
[1]. Heithersay GS, Management of tooth resorptionAust Dent J Supplement 2007 52(Suppl 1):S105-21. [Google Scholar]
[2]. Ozer SY, Diagnosis and Treatment Modalities of Internal and External Cervical Root Resorptions: Review of the Literature with Case ReportsInt Dent Res 2011 1:32-37. [Google Scholar]
[3]. Leung SF, Cone Beam Computed Tomography in Endodontics. Dental bulletinThe Hong Kong Medical diary 2010 15(3):16-19. [Google Scholar]
[4]. Taneja S, Mishra N, Malik S, Comparative evaluation of human pulp tissue dissolution by different concentrations of chlorine dioxide, calcium hypochlorite and sodium hypochlorite: An in vitro studyJ Conservative Dent 2014 17:541-45. [Google Scholar]
[5]. Vijayaraghavan R, Mathian VM, Sundaram AM, Karunakaran R, Vinodh S, Triple antibiotic paste in root canal therapyJ Pharma Bio allied Sci 2012 4(suppl2):S230-33. [Google Scholar]
[6]. Nilsson E, Bonte E, Bayet F, Lasfargues JJ, Management of internal root resorption on permanent teethInt J Dent 2013 2013Article ID 929486 [Google Scholar]
[7]. Nunes E, Silveria FF, Soares JA, Duate MAH, Soares SMCS, Treatment of perforating internal root resorption with MTA: a case reportJ Oral Sci 2012 54:127-31. [Google Scholar]
[8]. Sari S, Sönmez D, Internal resorption treated with mineral trioxide aggregate ina primary molar tooth: 18-month follow-upJ Endod 2006 32:69-71. [Google Scholar]
[9]. Monticelli F, Sword J, Martin RL, Schuster GS, Weller RN, Ferrari M, Sealing properties of two contemporary single-cone obturation systemsInt Endo J 2007 40:374-85. [Google Scholar]
[10]. Polansky R, Haas M, Helschl A, Wimmer G, Clinical effectivenessof photodynamic therapy in the treatment of periodontitisJ ClinPeriodontol 2009 36:575-80. [Google Scholar]
[11]. Vanooteghem R, Hutchens LH, Garret S, Kiger R, Egelberg J, Bleeding on probing and probing depth as indicators ofthe response to plaque control and root debridementJ ClinPeriodontol 1987 14:226-30. [Google Scholar]