Malignant Peripheral Nerve Sheath Tumour of Small Intestine Presenting as Ileo-Ileal Intussusception - A Rare Tumour with Unusual Complication
Diwakar Pandey1, Ankur Verma2, Azaz Akhtar3, Ashish Arsia4, Nain Singh5
1 Post Graduate Student, Department of Surgery, Lady Hardinge Medical CollegeNew Delhi, India.
2 Senior Resident, Department of Surgery, Lady Hardinge Medical CollegeNew Delhi, India.
3 Associate Professor, Department of Surgery, Lady Hardinge Medical CollegeNew Delhi, India.
4 Associate Professor, Department of Surgery, Lady Hardinge Medical CollegeNew Delhi, India.
5 Associate Professor, Department of Surgery, Lady Hardinge Medical CollegeNew Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ankur Verma, 134D Pocket F, GTB Enclave New Delhi-110093, India. E-mail : geniusav23@gmail.com
Malignant Peripheral Nerve Sheath Tumours (MPNST) arises from a peripheral nerve or exhibit nerve sheath differentiation on histology. Proximal portions of the upper and lower extremities and the trunk are the most common sites of occurrence. Around 50% are associated with Neurofibromatosis Type 1 (NF1) with incidence of two to five per cent in patients with NF1. The estimated incidence in general population without NF1 is 0.0001% of which gastrointestinal MPNST are extremely rare. A 45-year-old lady without pathological antecedent for NF1 was admitted with pain in right lower abdomen and multiple episodes of vomiting for 3 months. Preoperatively intussusception was diagnosed in the small bowel with USG and CECT abdomen showing characteristic target sign. On laparotomy Ileo-ileal intussusception (proximal ileum telescoping into distal ileum) was found 2 feet proximal to ileo-caecal junction with surrounding inflammed mesentery and presence of intraluminal tumour as lead point. Resection of involved segment of ileum along with its mesentery was done followed by ileo-ileal anastomosis. Histopathology was suggestive of high grade MPNST. Postoperative course and follow up for last 10 month is uneventful. This case is unique in terms of a rare tumour presenting with unusual complication and only one case had been reported so far in western literature.
Gastrointestinal MPNST, Ileum, Neurofibromatosis
Case Report
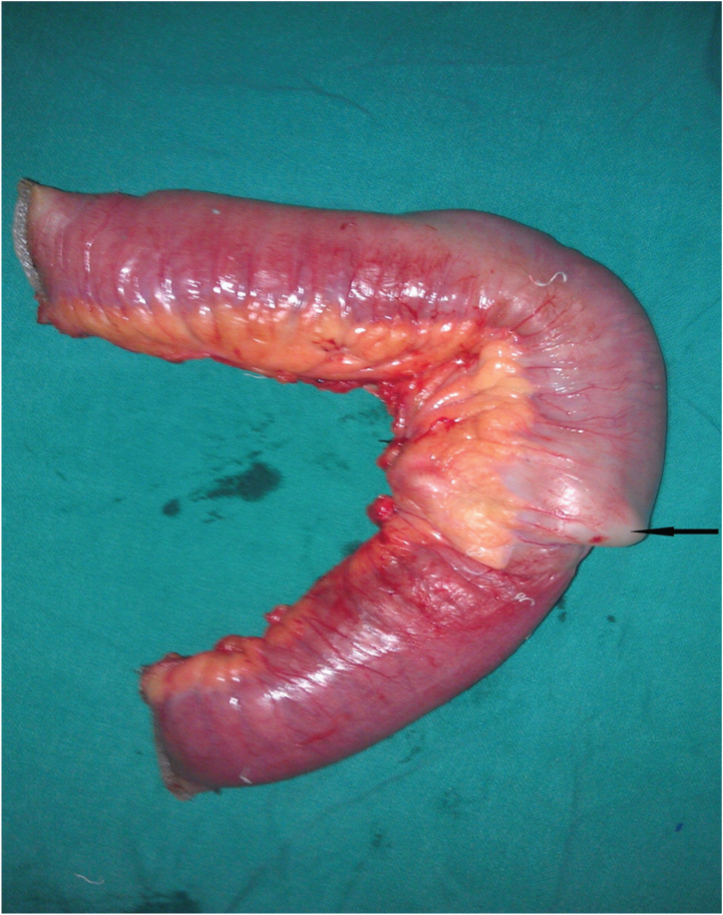
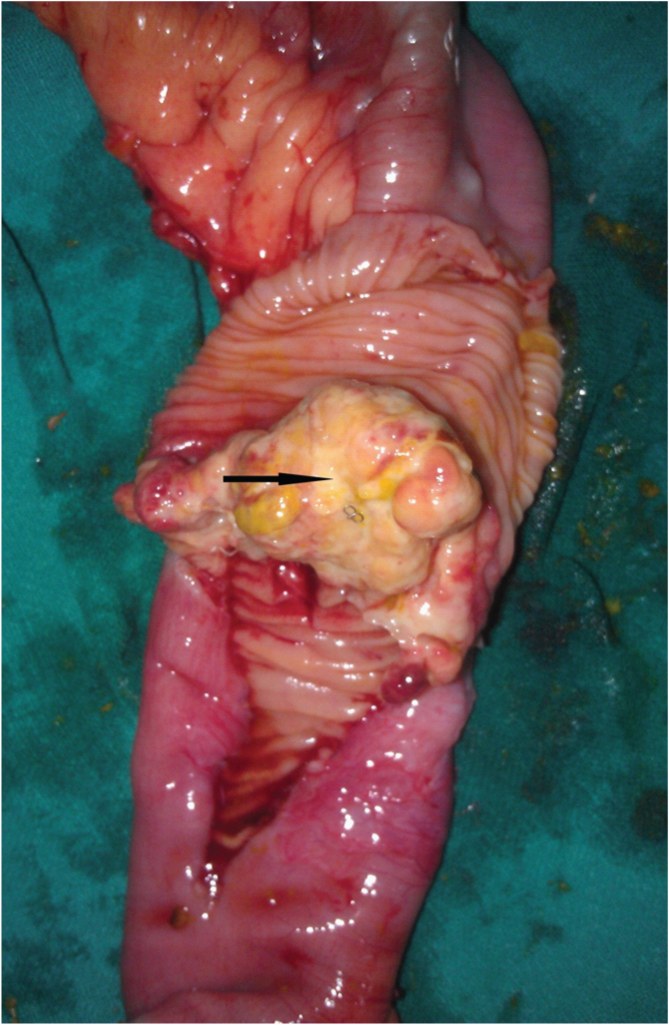
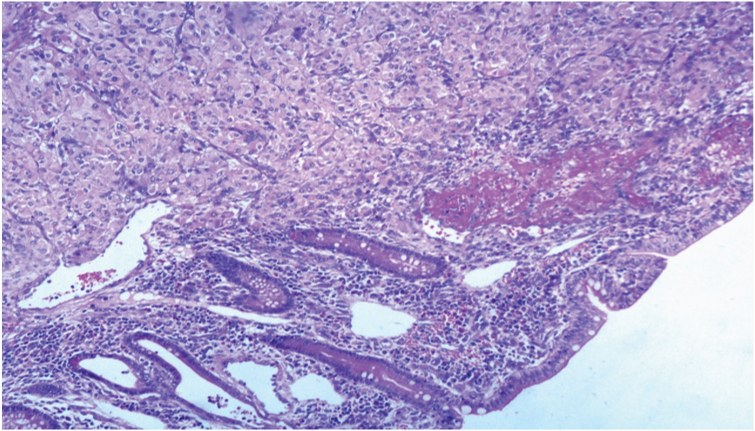
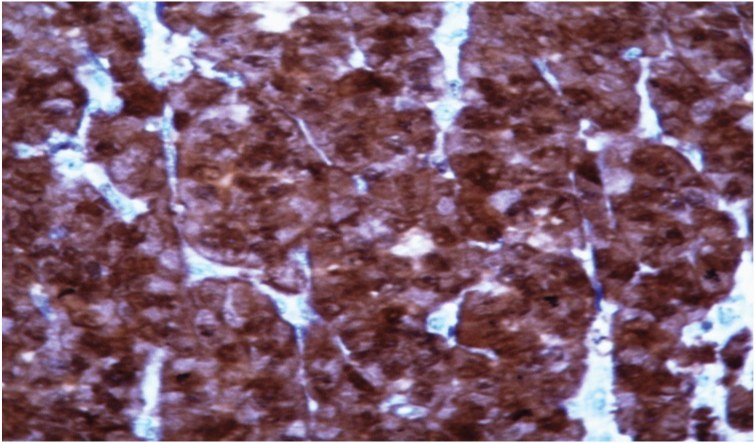
A 45-year-old lady without pathological antecedents for NF-1 was admitted with pain in right lower abdomen and multiple episodes of bilious vomiting on and off for three months. Past history was insignificant except for presence of controlled hypertension and Type 2 Diabetes Mellitus. On clinical examination, she had tender right iliac fossa with no palpable lump in abdomen. Preoperatively we diagnosed intussusception in the small bowel by USG and CECT abdomen-pelvis showing characteristic “Target sign” suggestive of intussusception [Table/Fig-1]. Patient underwent lower midline laparotomy under general anaesthesia. Operating surgeon discovered Ileo-Ileal Intussusception two feet proximal to Ileo-caecal junction with surrounding inflamed mesentery and presence of intraluminal tumour as lead point. Resection of involved segment of ileum along with its mesentery was done followed by Ileo-ileal anastomosis [Table/Fig-2,3]. Histopathology revealed malignant spindle cells with wavy, hyperchromatic nuclei and alternating hypercellularity with hypocellularity characteristically suggestive of MPNST. Mitotic index was 8 mitoses per 10 High power fields with all surgical margins free of tumour [Table/Fig-4]. On immunohistochemistry, tumour was positive for S-100 but negative for CD-34, smooth muscle actin, vimentin, desmin, c KIT and cytokeratin [Table/Fig-5]. Follow up for last 10 months is uneventful. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
CECT whole abdomen (axial view) suggestive of characteristic “target sign” in small bowel intussusception

Resected ileum along with growth acting as lead point
The intraluminal extension of growth on opening ileum
Malignant spindle cells with wavy, hyperchromatic nuclei and alternating hypercellularity with hypocellularity . (H and E, ×100)
Histopathology microphotograph (H and E,x400) tumour cells are S-100 positive
Discussion
Malignant peripheral nerve sheath tumour (MPNST) is defined as tumour arising from a peripheral nerve or exhibiting neural differentiation on histology [1]. Most common sites of occurrence are proximal portions of upper and lower extremities and the trunk. The overall incidence in general population is 1/100000 with 5 to 42 % of which are associated with NF-1 [2,3]. The MPNST of GI tract is extremely rare. The literature to date has fewer than 14 cases of MPNST arising in the gastrointestinal tract, and only three cases were ever reported in the small intestine of which one presented with small bowel intussusception [4–6]. The disease is thought to be arising from Aurbach plexus [7] generally remaining in submucosa but can grow exophytically or intraluminally. Majority of MPNST are high grade tumours with high likelihood of local recurrence and distant metastasis [8]. Clinical symptoms of GI MPNST are usually nonspecific, presenting as abdominal pain (63%), weight loss (44%), vomiting (43%) and GI bleed (23%) [9]. Intraoperatively Intussusception and obstruction is uncommon presentation of these tumours. On extensive literature search till date we could find only single reported case of MPNST of small bowel presenting as intussusception [7]. Imaging techniques used for evaluation includes ultrasonography, CT scan, MRI and FDG-PET contributing to easy detection, staging, therapy planning and follow up [10]. MPNST usually tends to be heterogeneous in CT attenuation and MRI signal intensity because of frequent necrosis within the mass [11]. When presented with Intussusception, characteristic “Target sign” is seen in ultrasonography and CT abdomen. It is quite impossible to predict the nature of tumour viz. benign or malignant on imaging, although in some studies Gallium citrate (67Ga) scintigraphy has been found to be helpful with tumour with malignant potential having increased Gallium citrate uptake but no uptake doesn’t rule out malignancy [12,13]. On histopathological analysis, MPNST usually show spindle cells with high mitotic index. Confirming diagnostic features include a) alternating hypocellular and hypercellular region, b) appearance of thin, wavy, comma or bullet shaped nuclei usually in hypocellular mass, c) presence of nuclear palisading, which may also be seen in leiomyosarcoma, d) presence of nerve like whorls or tactoid bodies resembling wagner-meissner corpuscles, e) prominent thick walled vasculature and presence of heterologous element. Immunohistochemistry markers for MPNST includes S-100 (in 50-90% of patients) characteristic of neural derived neoplasm, Leu 7 and Myelin base protein (in 50% and 40% of patients respectively) [14,15]. Desmin and α-SMA positivity exclude smooth muscle tumours whereas CD-34 and CD-117 (cKIT) positivity excludes GIST [16]. High levels of P53 and Ki67 may also be related to malignancy in a peripheral nerve sheath tumour according to a study [17].
Current protocols for treatment of MPNST arising from small bowel are still undefined. Current recommendation may be radical surgical treatment with wide excision as followed elsewhere. Poor prognostic factors which may entail patient to local recurrence and distant metastasis are Size 5cm or more, incomplete resection and association with NF-1. Most case series of such tumours with poor prognosis suggest limited benefit and high morbidity of using adjuvant radiotherapy and chemotherapy. Although No Phase II & III trials are available, Doxorubicine-ifosfamide based Chemotherapy has been found to be having better outcome than placebo in some series which warrants further consideration [18].
Conclusion
We report a rare case MPNST presenting as ileo-ileal intussusception. High index of suspicion along with multidisciplinary approach is essential for diagnosis and treatment of these tumours. There is no definitive guideline available for treatment of small bowel MPNST, although radical surgical treatment with wide excision is universally done. Role of adjuvant radiotherapy and chemotherapy is still under debate reserved only for advanced and recurrent tumours.
[1]. Weiss SW, Goldblum JR, Malignant TUMOURs of the peripheral nerves.In: Weiss SW, Goldblum JR editorsEnzinger and Weiss’s soft tissue TUMOURs 2001 4th edMosby:1209-63. [Google Scholar]
[2]. Kar M, Suryanarayana Deo SV, Shukla NK, Malignant peripheral nerve sheath TUMOURs (MPNST)—clinicopathological study and treatment outcome of twenty-four casesWorld Journal of Surgical Oncology 2006 4article 55 [Google Scholar]
[3]. Doorn PF, Molenaar WM, Buter J, Hoekstra HJ, Malignant peripheral nerve sheath TUMOURs in patients with and without neurofibromatosisEuropean Journal of Surgical Oncology 1995 21(1):78-82. [Google Scholar]
[4]. Nozu T, Takahashi A, Asakawa H, Malignant intestinal schwannoma: a case review and a review of the literature in JapanIntern Med 1995 34:1101-05. [Google Scholar]
[5]. Yilmaz F, Uzunlar AK, Bukte Y, Recurrent malignant schwannoma of the small intestineActa Med Austriaca 2004 31:58-60. [Google Scholar]
[6]. Dana A, Pertsemlidis D, Malignant Peripheral Nerve Sheath TUMOUR: An Unusual Cause of IntussusceptionJ Gastro intest Surg 2008 12:1609-11. [Google Scholar]
[7]. Mirowski GW, Mark LA, Oral disease and oral-cutaneous manifestations of gastrointestinal and liver diseaseIn: Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. Feldman M, Friedman LS, Brandt LJ (eds.) 2006 PhiladelphiaSaunders:443-63. [Google Scholar]
[8]. Enzinger FM, Weiss SW, Malignant TUMOURs of the peripheralnervesIn: Soft Tissue TUMOURs 1995 3rd editionSt LouisMosby-Year Book:889-928.Enzinger FM, WeissSW (Eds.) [Google Scholar]
[9]. Talamonti T, Goetz G, Joehl J, Rao R, Primary cancersof the small bowel: analysis of prognostic factors and results ofsurgical managementArchives of Surgery 2002 137(5):564-71. [Google Scholar]
[10]. Chander S, Westphal SM, Zak IT, Bloom DA, Zingas AP, Joyrich RN, Retroperitoneal MPNST: evaluation with serial FDG-PETClin Nucl Med 2004 29:415-18. [Google Scholar]
[11]. Fenton LZ, Foreman N, Wyatt-Ashmead J, Diffuse, retroperitoneal mesenteric and intrahepatic periportal plexiform neurofibroma in a 5-year-old boyPediatr Radiol 2001 31:637-39. [Google Scholar]
[12]. Levine E, Huntrakoon M, Wetzel LH, Malignant nerve-sheath neoplasms in neurofibromatosis: distinction from benign TUMOURs by using imaging techniquesAJR 1987 149:1059-64. [Google Scholar]
[13]. Hammond JA, Driedger AA, Detection of malignant change in neurofibromatosis (von Recklinghausen’s disease) by gallium-67scanningCan Med Assoc J 1978 119:352-53. [Google Scholar]
[14]. Matsunou H, Shimoda T, Kakimoto S, Yamashita H, Ishikawa E, Mukai M, Histopathologic and immunohistochemical study of MPNSTs (malignant schwannoma)Cancer 1985 56:2269-79. [Google Scholar]
[15]. Wick MR, Swanson PE, Scheithauer BW, Manivel JC, MPNST: an immunohistochemical study of 62 casesAm J Clin Pathol 1987 87:425-33. [Google Scholar]
[16]. Kim JG, Sung WJ, Kim DH, Kim YH, Sohn SK, Lee KB, Malignant peripheral nerve sheath TUMOUR in neurofibromatosis type I: unusual presentation of intraabdominal or intrathoracic massKorean Journal of Internal Medicine 2005 20(1):100-04. [Google Scholar]
[17]. Kindblom LG, Ahlden M, Meis-Kindblom JM, Stenman G, Immunohistochemical and molecular analysis of p53, MDM2, proliferating cell nuclear antigen and Ki67 in benign and malignant peripheral nerve sheath tumoursVirchows Archiv 1995 427(1):19-26. [Google Scholar]
[18]. Kroep JR, Ouali M, Gelderblom H, First-line chemotherapy for malignant peripheral nerve sheath TUMOUR (MPNST) versus other histological soft tissue sarcoma subtypes and as aprognostic factor for MPNST: an EORTC Soft Tissue and Bone Sarcoma Group studyAnnals of Oncology 2011 22(1):207-14. [Google Scholar]