Disseminated Congenital Neuroblastoma – An Autopsy Case Report
Jyotsna. V. Wader1, Sujata. S. Kumbhar2, Dhirajkumar B Shukla3, Sonu Mavi4
1Professor, Department of Pathology, Krishna Institute of Medical Sciences University, Karad, Maharashtra, India.
2Assistant Professor, Department of Pathology, Krishna Institute of Medical Sciences University, Karad, Maharashtra, India.
3Assistant Lecturer, Department of Pathology, Krishna Institute of Medical Sciences University, Karad, Maharashtra, India.
4Assistant Lecturer, Department of Pathology, Krishna Institute of Medical Sciences University, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyotsna. V. Wader, Professor, Department of Pathology, Krishna Institute of Medical Sciences University, Krishna Hospital and Medical Research Centre, Karad-415110, Maharashtra, India.
E-mail: jyowader@gmail.com
Neuroblastoma is the most common malignant tumour in the neonatal age group. The tumour is derived from neural crest cells of adrenal gland medulla or sympathetic ganglia. Disseminated congenital neuroblastoma is very rare. We hereby report a case of congenital neuroblastoma with multiple metastases diagnosed on autopsy in a fetus of 23 weeks gestational age. Autopsy revealed enlarged bilateral adrenals, large fusiform mass in the right humerus, mass in the lower lobe of left lung and posterior chest wall. Diagnosis of disseminated congenital neuroblastoma was given after histopathological and immunohistochemical examination. We are reporting this case for its rare presentation of disseminated form of congenital neuroblastoma sparing liver.
Bilateral neuroblastoma, Fetal autopsy, Metastases
Case Report
A 22-year-old female, gravida, was referred to our hospital for 8 months of amenorrhea with intrauterine death of the fetus. Previous pregnancy was uneventful with a healthy living 3-year-old female child. Previous ultrasound scan at 16 weeks of pregnancy was normal with a single live intrauterine fetus whereas scan at 32 weeks of amenorrhea revealed a single intrauterine fetus of 23 weeks 6 days (± 1 week) gestational age with a large soft tissue mass in right arm (? Rhabdomyosarcoma) with enlarged adrenal glands. She underwent emecredil instilled complete evacuation after all routine investigations were within normal limits.
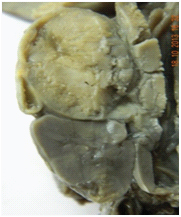
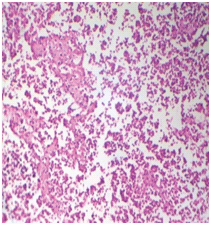
A complete fetal autopsy was performed after informed consent. Pathological examination of placenta was also performed. A macerated male fetus of gestational age 23 weeks weighing 680 grams showed a large fusiform swelling measuring 7x6x2.5 cms in right arm with intact skin [Table/Fig-1]. Cut section of the arm swelling showed a gray tan mass involving the humerus bone and surrounding soft tissue [Table/Fig-2]. Other anomalies noted on morphological examination were cleft lip, saddle nose, abnormal epicanthal folds and flexion deformity in both the lower limbs with high arched left foot. Thoracic cavity revealed a solid mass measuring 3x2x2 cm in lower lobe of left lung [Table/Fig-3] and a solid nodule in posterior chest wall. Cut section of the left lung mass showed gray tan appearance [Table/Fig-4]. Abdominal dissection revealed bilateral enlarged adrenals, left abdominal testis and agenesis of right testis. Liver and spleen were unremarkable. Cut sections from both the adrenals showed tan gray mass compressing the renal parenchyma [Table/Fig-5,6].
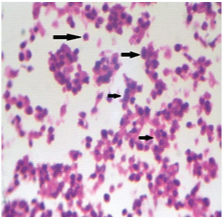
Paraffin sections from bilateral adrenals, right arm mass, left lung mass and posterior chest wall nodule showed tumour composed of solidly packed cells separated by fibrous stroma [Table/Fig-7]. Individual cells were small having round to oval nucleus with fine chromatin and scant cytoplasm [Table/Fig-8]. On the basis of histopathological study diagnosis of disseminated malignant small round cell tumour was given. Placental examination was unremarkable.
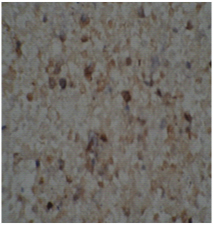
Further study of tumour was done using panel of markers namely Neuron Specific Enolase (NSE), CD99, CD45, Vimentin and myogenin. Tumour cells showed positivity for NSE [Table/Fig-9] and negativity for CD99, Vimentin, CD45 and Myogenin. Negativity for CD99, Vimentin, CD45 and Myogenin ruled out very close differential diagnosis of Ewing Sarcoma Family Tumour (ESFT), lymphoblastic lymphoma and embryonal rhabdomyosarcoma respectively, thereby bringing us to the final diagnosis of disseminated congenital neuroblastoma.
Discussion
Congenital malignant tumours are very rare with neuroblastoma accounting for majority of the cases [1]. Neuroblastoma was first described by Virchow in 1863 [2]. About 80 cases of congenital neuroblastoma have been described [3,4]. The overall reported incidence of neuroblastoma is 58 per 1 million infants per year [5]. Neuroblastoma is a poorly differentiated neoplasm derived from neural crest ectoderm [2]. Most of the cases of neuroblastoma arise in the adrenal glands [6]. Congenital neuroblastoma is a rare entity. Bilateral involvement of adrenal glands has been noted in less than 10% of cases with neuroblastoma [6], as was noted in the present case. Bilateral involvement may occur either by synchronous development or metastatic spread of the tumour [6]. Disease dissemination occurs through lymphatic and haematogenous routes. Bone, bone marrow and liver are the most common site of haematogenous spread with particular predilection for metaphyseal, skull and orbital bone sites [7]. In present case, dissemination was noted in right humerus with adjacent soft tissue involvement, lower lobe of left lung and posterior chest wall. However, liver parenchyma did not show any evidence of tumour cells. Beckwith and Perrin proposed the concept of in situ neuroblastoma, for neuroblastomatous foci confined to the adrenals of newborns [8]. The incidence noted by different authors in autopsy series ranges from 0.4% to 2.5%. High rate of neuroblastoma in situ in comparison with rarely encountered clinically apparent neuroblastomas, has been attributed to suggestion that a substantial number may undergo spontaneous regression and degeneration or maturation [2,3]. Shimada along with his associates proposed a histological system for stratifying neuroblastic tumours correlating prognosis with histological presentation [9]. System proposed by Shimada and his associates was replaced by the “International Neuroblastic Pathology Classification” (INPC) [2]. Based on the clinical pattern of the tumoural dissemination evidenced by imaging studies, surgical resectability, and involvement of lymph nodes and bone marrow, a staging system “International Neuroblastoma Staging System” (INSS) has been devised [2]. Prenatal diagnosis of congenital neuroblastoma was first described by Fernart and associates in 1983 [10].
Genomic amplication of gene MYCN (located in the short arm of chromosome 2 is the most common genetic aberration associated with the worst prognosis among neuroblastomas [2]. Other alterations that have been identified are loss of heterozygosity of 1p and 11q and increased expression of TrkA [2]. Neuroblastoma cells can produce and excrete substances such as vanillylmandelic acid (VMA), homovalnillic acid (HVA), neurone specific enolase (NSE), vasoactive intestinal peptide, ferritin and lactic dehydrogenase. NSE is the tumour marker for neuroblastoma [6].
Ultrasound is a useful screening modality in the evaluation of neuroblastoma. In our case ultrasonography only showed swelling over right arm and enlarged adrenals with possibility of rhabdomyosarcoma of right arm. However, with detailed morphological, histopathological and immunohistochemical examination, diagnosis of disseminated congenital neuroblastoma was made.
Macerated fetus with a large fusiform mass in right arm

Cut section of the arm swelling showing tan coloured mass

Mass in the lower lobe of left lung

Cut section of the left lung mass with gray tan appearance

Cut section showing enlarged left adrenal with gray tan mass and compressed kidney
Cut section showing enlarged right adrenal with gray tan mass and compressed kidney

Photomicrograph showing tumor composed of solid packed cells separated by fibrous septa. (H & E stain, 100x)
Photomicrograph showing tumor cells having small round blue nucleus and eosinophilic cytoplasm. (H & E stain, 400x)
Photomicrograph showing positivity of tumor cells for NSE
Conclusion
Congenital bilateral neuroblastoma is a rare entity. Ultrasonography can be a tool in the diagnosis of neuroblastoma but sometimes it can be missed. Fetal autopsy alone or in conjunction with ancillary techniques play an important role in the diagnosis of neuroblastoma in the cases with unusual presentation especially the one with disseminated form and sparing liver as in the present case.
[1]. Parambath A Nelliyulla, Rajendran V, Vasu C, Congenital neuroblastoma: A Case ReportThe Internet Journal of Radiology 2007 9(1) [Google Scholar]
[2]. AD Costa, MCN Zerbini, L Cristofani, Metastatic congenital neuroblastoma associated with in situ neuroblastoma: case report and review of literatureAutopsy Case Rep 2014 4(2):27-33. [Google Scholar]
[3]. Sul HJ, DY Kang, Congenital Neuroblastoma with Multiple Metastases: A Case ReportJ Korean Med Sci 2003 18:618-20. [Google Scholar]
[4]. B Pongtanakul, KS Sanpakit, G Veerakul, Congenital Bilateral Neuroblastoma presenting with Hepatic FailureThai J Haematol Transf Med 2003 13:141-46. [Google Scholar]
[5]. JG Nuchternn, Perinatal NeuroblastomaSeminars in Pediatric Surgery 2006 15(1):10-6. [Google Scholar]
[6]. A Chandraprakash, Abhijeet A Shamim, A Rupa, VV Kumar, Bilateral Adrenal Neuroblastoma; Stage IV – A P Case ReportSch J App Med Sci 2013 1(4):298-300. [Google Scholar]
[7]. JR Park, A Eggert, H Caron, Neuroblastoma: Biology, Prognosis and TreatmentPediatr Clin N Am 2008 55:97-120. [Google Scholar]
[8]. JB Beckwith, EV Perrin, In situ neuroblastomas: a contribution to the natural history of neural crest tumours Am J Pathol 1963 43:1089-104. [Google Scholar]
[9]. H Shimada, J Chatten, WA Newton, N Sachs, AB Hamoudi, T Chiba, Histopathologic prognostic factors in neuroblastic tumours: definition of subtypes of ganglioneuroblastoma and an age-linked classification of neuroblastomasJ Natl Cancer Inst 1984 73:405-16. [Google Scholar]
[10]. Fénart D, Deville A, Donzeau M, Bruneton JN, Retroperitoneal neuroblastoma diagnosed in utero. Apropos of 1 caseJournal de Radiologie 1983 64(5):359-61. [Google Scholar]