Introduction
Smoking, the most fatal form of tobacco use and is attributed to 5 million deaths worldwide [1,2]. World Health Organization has estimated that about half of the smokers will eventually die prematurely due to persistent smoking habit [1]. Smoking is responsible for numerous of fatal or non fatal health disorders which includes cancer of lung, larynx, stomach, liver, leukaemia, chronic obstructive pulmonary disease, cardiovascular disease, vascular dementia, asthma attacks, macular degeneration and peripheral vascular disease [2].
It was been estimated that 20% of the global population smokes tobacco [3]. Eighty percent of the global tobacco related mortality occurs in low and middle income countries [3,4]. India is not lagging behind in tobacco consumption and smoking. It is second largest consumer of tobacco products [4] and contributes to the largest global tobacco-related mortality [3]. Prevalence of smoking among the Indian males is as high as one fourth of the total male population above 15 years of age [5,6]. Twenty six percent of Indians are smokers [3,7]. Alongside of physical and mental burden, smoking is attributable for burden of social, economic and environmental factors [3]. The indirect and direct economic costs of smoking to India amounted to $1.7 billion in 2004 due to tobacco use [8].
Smoking initiation and pursuance depends on smoking by their favourite movie stars [9] parents’ smoking [10] peer pressure [11] culture (hookah smoking) [12] genetic factors and environmental influences [5]. Smoking among friends, siblings, relatives and parent-teen conflicts, parental monitoring and discussion in the family about smoking hazards are significant predictors of smoking stages [13]. Cessation of smoking can involve influencing the behavior of smokers by regular counselling and mass media, limiting influence of smoking family members, role models (smoking), tobacco industry, empowerment, education, coercion and promotion of treatment in drug de-addiction centers [2]. There are existing policies to reduce the burden of smoking but they had minimal impact due to lack in their effective implementation [14].
There is need of understanding all inclusive roles of multiple factors responsible for smoking initiation and the role of barriers in cessation for developing ‘impactful customized interventions to decrease burden of smoking [3]. The commonest form of known incentive for cessation of smoking is quit and win competition and it has shown positive results, but likelihood of its misuse is a matter of concern [2]. Previous literature have stressed on exploring further evidence on incentives for promoting smoking cessation [15,16]. The objective of this study was thus to assess the factors leading to smoking initiation and cessation along with exploring of various types of incentives needed to promote smoking cessation.
Materials and Methods
A cross-sectional study was conducted in August 2013 for a period of one month at outpatient department (OPD) of Saveetha Medical College and Hospital, Chennai, India, and individuals visiting to the OPD were considered as sampling frame for the study. Inclusion criteria of the study comprised of Individuals of age equal or above 15 years of age, current smokers (smoked at least 100 sticks of cigarettes or similar products - bidis, hookahs, cigars and pipe) in their lifetime, reported smoking daily or occasionally) [17] and ready to give informed consent or assent (along with their parents consent for individuals having age less than 18 years) for the study. Recruitment of the participants was done on the basis of convenient sampling. Investigator approached the visitors (patients and attendants) of the OPD on convenient basis and among them who were found eligible to participate in the study were invited for participation in the study after explaining the purpose of the study. This procedure was repeated until the desired target of 100 participants was achieved. Investigator administered the questionnaire in separate room to maintain the confidentiality. Anonymity of the participants was maintained by assigning unique identity code. Individuals who were not fulfilling the inclusion criteria, having mental or physical challenges, involved in any other clinical trial or unwilling to participate in current study were excluded from the study. The study protocol was approved by the IRB of the Foundation of Healthcare Technologies Society, New Delhi (IRB#FHTS/009/2013).
Data collection
A modified version of previously validated questionnaire was used to gather information. World health organization’s (WHO) ASSIST was contextually modified and used in this study which is a validated tool, feasible, reliable, flexible, comprehensive and cross-culturally relevant, and able to be linked to brief interventions [18-20].
Information was gathered on the following variables
(a) socio-demographic characteristics (age, gender, educational status, marital status, annual household income [21], type of family, number of family members, and occupation status); (b) smoking habits (smoking habits, substances used in lifetime and initiation time of smoking, urge to smoke during last three months, concerns of other people on the individual’s smoking habit, quitting or reducing smoking, smoking partners, smoking after meals and along with/ after liquids’ consumption, effect of smoking on individual’s financial status); (c) smoking initiation (reasons for smoking initiation, participants’ influence on other persons to smoke, use of addictive or other products along with smoking tobacco); (d) accessibility of smoking products (most preferred smoking area, time spent on acquiring smoking product, factors encouraging smoking, availability of smoking products at workplace); (e) expenditure on smoking products (daily expenditure on smoking products, frequency and number of sticks of smoking product smoked per day); (f) smoking cessation (participants’ intention of quitting smoking within the immediate 30 days and 6 months, source of information about smoking cessation products/programs), and (g) incentives (open ended questions on different incentives and motivating factors that would help in smoking cessation). Also, questions regarding the participant's opinion about other people were also asked.
Statistical Analysis
Quantitative descriptive analysis was performed using univariate statistics to report means and standard deviations for the continuous variables and frequency distribution for the categorical variables. T statistics was performed to compare differences in the continuous variables and chi-square analysis was performed to compare the frequency of categorical variables. Analysis of responses to open ended questions was done by extracting common themes from categories after prior coding of textual data manually. All analyses were performed using SPSS version 16.
Results
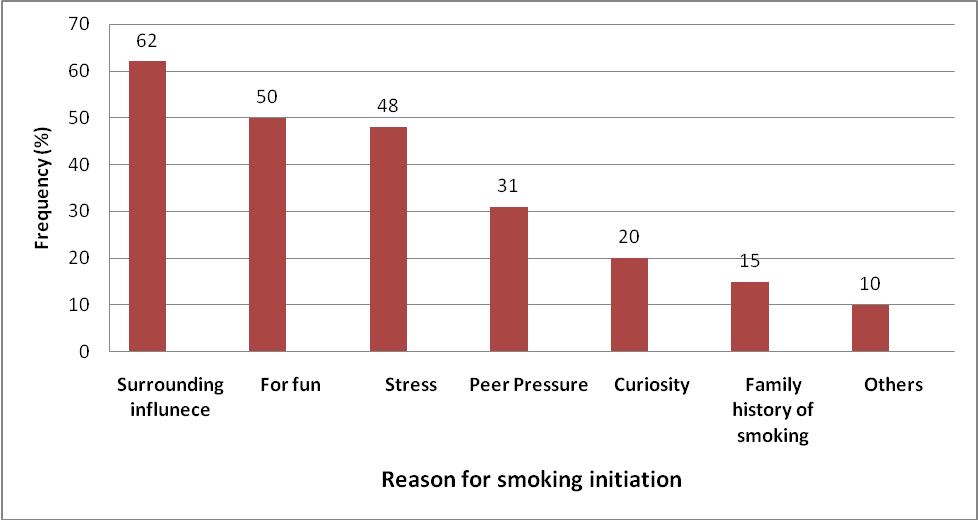
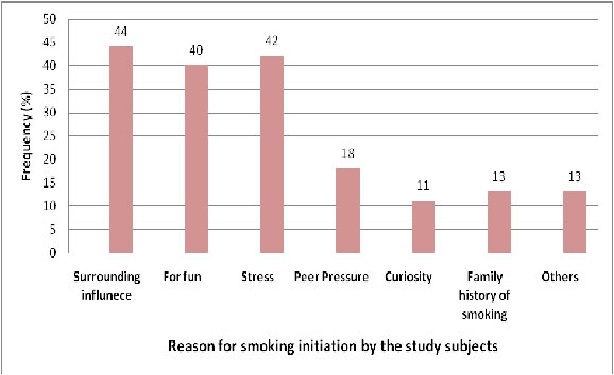
All participants were males with an average age of 43 years (SD = 11). Majority of them were married (88%), residing in rural settings (82%) and having nuclear families (75%) with an average family size of 5 (SD = 2). Sixty four percent of the study participants were educated up to high school. More than half of the participants were unskilled professionals and 44% of the participants had annual household income of more than 100,000 INR (US$ 1613 approx.) [Table/Fig-1]. Smoking initiation, continuation and cessation pattern among the participants. Average age of the study participants who smoked cigarettes and bidi were 41 years (SD = 11) and 48 years (SD = 11) respectively. Mean age of initiating smoking was lower among the Bidi smokers (M = 18; SD = 5) in comparison with cigarette users (M = 22; SD = 5). Majority of them were smoking daily (98%) with an average of 9 (SD = 4) sticks smoked by cigarette smokers and 19 (SD = 9) sticks by bidi smokers. More than half of the study participants had a strong urge to smoke cigarettes daily (65%). Majority of the study participants reported smoking with their friends (83%) and 10% reported smoking when alone. Surrounding influence (62%), fun (50%), stress (48%), and peer pressure (31%) were among the main reasons reported by the participants which could lead a person to initiate smoking. Study participants had initiated smoking due to surrounding influence (44%), during stress (42%) and for fun (40%) [Table/Fig-2,3] .
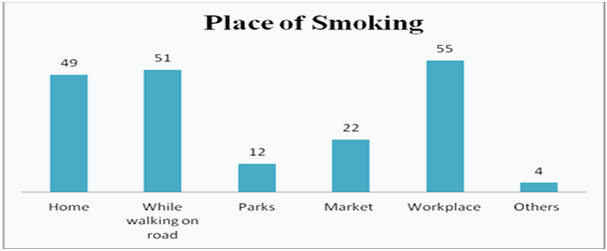
Participants have reported availability of smoking products at an average walking distance of 6 minutes (SD = 4) from work place or home. Fifty-five percent participants reported smoking at work place and 49% of them smoked at home [Table/Fig-4] . More than half of them had access to smoking products (52%) near work place.
Fourteen percent of the participants reported that they have influenced one or more individuals to smoke. Seventy nine percent of the participants had perception that consummation of addictive substance or drugs do not encourage smoking. Majority of the participants perceived that free availability of smoking aids did not encourage them to smoke (71%), while easy availability and accessibility may promote (54%). Half of the study participants admitted that they had faced some kind of health problems, legal penalties, social isolation or financial crisis related to smoking.
More than three quarter of the participants (77%) tried to quit smoking in past but failed and among them 47% attempted to quit smoking in the past three months. One third of the participants have shown desire to quit smoking within next six months. Twenty one percent of the participants have heard about nicotine use curbing substances and 18% of them had heard about nicotine de-addiction centre [Table/Fig-5]. Television (13%) and friends (12%) were the main source of information about the de-addiction centre.
Incentives for smoking cessation: Majority of the participants perceived that health promotion programs (62%) could be of the greatest help to help them quit smoking. One fifth (22%) of the participants perceived that financial incentives as a motivating factor. Other incentives to quit smoking included promotion of self-control mechanisms (10%), involvement of family members (16%), and counselling and guidance (3%). Association between independent variables with intent to smoking cessation .
Statistical analysis was performed to see any difference in independent variables of the participants who had shown desire or no desire to quit smoking in next six months. It was found that none of the Socio-demographic variables had shown any statistical significance difference. Time duration required to reach nearest cigarette or bidi vendor was slightly higher for those who had shown intention to quit smoking (p=.02). Participant who have heard about deaddiction centre (56%) were in higher proportion for willingness to quit smoking in future in comparison to participants who have never heard (29%) about nicotine deaddiction centre (p=.03) [Table/Fig-6].
Discussion
World Health Organization predicts the largest increase, over 1.5 million annually, in tobacco related deaths in India by 2020 [22]. This cross-sectional study was conducted primarily to assess the reasons for smoking initiation, barriers in quitting and also to explore various incentives that could help in cessation of smoking [3]. Mean age of initiation smoking among the current smokers was 21 years (SD = 5). Binnal et al., reported similar mean age of 20 years (SD = 4) at which most of the study subjects initiated smoking [3]. Age plays an important role in determining the smoking habits in future life which may need an intervention targeting at early school ages [23,24]. The risks of tobacco- related diseases are higher among those who start early and continue using it [24].
Surrounding influence, stress, fun and peer pressure were the major reasons for smoking initiation. Stress [3,25], pleasure [3], peer [26] and social pressure [3] have been reported as predominant reasons for smoking initiation among teachers and adolescents. These findings depict the important role played by surrounding influence and stress, an inevitable part of modern day life [3]. Identification of strong influences, targeted peer education and stress reduction strategies should be explored.
Majority of the participants smoked at their work places. Binnal et al., has reported majority of the participants smoking when they were outside their house, and suggested family counselling and advice to facilitate smoking cessation [3]. These findings also imply harnessing work places as an effective medium to promote smoking cessation. Accessibility of tobacco products around workplace showed to encourage the participants to smoke irrespective of the cost of the products.
About two thirds of the participants attempted to quit smoking in past and more than half of the participants had shown intent to quit smoking in near future. Previous studies have shown intention to quit smoking among participants ranging from 10 to 88% [3,7]. Huge variation in intention to quit smoking and higher failure rates could be attributed to multiple factors including behaviour, socioeconomic status, health education, environment and work culture. Lack of awareness on methods of quitting smoking and whom to approach for cessation of smoking despite intent to quit is a matter of concern.
The role of nicotine de-addiction centres at local level may need urgent attention as these have been suggested to facilitate in identification of smokers and thus assist smokers to quit smoking [3]. Majority of the participants in this study had not heard of nicotine de-addiction centres or the location of the one nearest to them. The possible involvement of traditional mass media like television and radio along with healthcare fraternity in spreading awareness of the importance and role of such centres may need to be explored further [3].
Health promotion programs and financial incentives were among the major types of incentives that were perceived by the participants’ to help in quitting smoking. Volpp et al., reported that employees receiving information about cessation and financial incentives had significantly higher cessation rates [27].
Socio-demographic characteristics of the participants
| Variables | Results (%) |
|---|
| Age (years) | Mean = 43; SD = 11 |
| ≤30 | 16 |
| 31-40 | 33 |
| 41-50 | 24 |
| >50 | 27 |
| Type of family |
| Joint | 25 |
| Nuclear | 75 |
| Household location |
| Urban | 18 |
| Rural | 82 |
| Household members | Mean = 5; SD = 2 |
| ≤3 members | 23 |
| 4-5 members | 53 |
| 6 and above | 24 |
| Annual household income, INR | Mean = 128101; SD= 116241 |
| ≤50,000 | 20 |
| 51,000–1,00,000 | 36 |
| >1,00,000 | 44 |
| Marital status |
| Single | 12 |
| Married | 88 |
| Education level |
| ≤Grade 10 | 64 |
| Grade 11-12 but no college | 28 |
| Graduate | 8 |
| Occupation |
| Professional | 13 |
| Skilled worker | 27 |
| Unskilled worker | 53 |
| Student | 7 |
Main Reasons to starting of smoking for first time for anyone - Perceptions of the study participants
Main Reasons for the study participants to start smoking for the first time
Various places of smoking as reported by the participants
Smoking initiation, habits and cessation of participants using two different smoking products
| Variables | Total (%) | Cigarette | Bidi |
|---|
| Smoking initiation age | Mean= 21; SD= 5 | Mean= 22; SD= 5 | Mean= 18; SD= 5 |
| ≤18 | 25 | 13 | 15 |
| 19–24 | 41 | 32 | 9 |
| ≥25 | 34 | 29 | 4 |
| How often do you smoke?* |
| Daily | 98 | 72 | 26 |
| Mean number of sticks | Mean= 12; SD= 7 | Mean= 9; SD= 4 | Mean= 19; SD= 9 |
| Do you smoke after meals?* |
| Yes | 88 | 64 | 24 |
| No | 12 | 10 | 3 |
| Smoking pattern (after meals)* |
| Breakfast | 62 | 40 | 22 |
| Lunch | 87 | 63 | 24 |
| Dinner | 70 | 47 | 23 |
| Substances used along with smoking* |
| Soft drink(aerated drink) | 11 | 11 | |
| Tea | 65 | 47 | 17 |
| Coffee | 24 | 17 | 6 |
| Alcohol (beer, whisky) | 44 | 29 | 14 |
| During past 3 months how often you had a strong urge to smoke?* |
| Daily | 86 | 65 | 23 |
| Once a week | 12 | 9 | 4 |
| Have you ever tried to cut down on smoking but failed? n=77 |
| In the past 3 months | 41 | 39 | 2 |
| Not in the past 3 months | 36 | 28 | 8 |
| Has smoking often led to problems?(personal/social/legal)N=50 |
| In the past 3 months | 29 | 21 | 8 |
| Not in the past 3 months | 21 | 16 | 5 |
| How often have you failed to do normal activities because of smoking? n=46 |
| In the past 3 months | 22 | 16 | 6 |
| Not in the past 3 months | 24 | 21 | 3 |
| Have you influenced anyone to smoke?* |
| Yes | 14 | 12 | 2 |
| No | 86 | 62 | 25 |
| Does use of any drug or addictive substance encourages smoking?* |
| Yes | 21 | 14 | 5 |
| No | 79 | 60 | 22 |
| Do free smoking products encourage you to smoke more often?* |
| Yes | 29 | 24 | 6 |
| No | 71 | 50 | 21 |
| Do you have access to smoking products at your workplace?* |
| Yes | 52 | 43 | 10 |
| No | 48 | 31 | 17 |
| Does accessibility to product increase your chance of smoking?* |
| Yes | 54 | 44 | 11 |
| No | 46 | 30 | 16 |
| Have you heard of nicotine de-addiction centres?* |
| Yes | 18 | 14 | 4 |
| No | 82 | 60 | 23 |
*Some response may not add up to 100 due to some of the participants smoke Bidi as well cigarette. Responses are in multiple scales
Association of independent variables with the intent of smoking cessation
| Variables | Intention to quit smoking within next 6 months | p-value |
|---|
| Yes | No |
|---|
| Age (Years) | 44 (SD=13) | 42 (SD=10) | .35 |
| Household location | .94 |
| Rural | 28 (34%) | 54 (66%) |
| Urban | 6 (33%) | 12 (67%) |
| Marital status | .74 |
| Single | 5 (42%) | 7 (58%) |
| Married | 29 (33%) | 59 (67%) |
| Family Type | .46 |
| Joint | 10 (40%) | 15 (60%) |
| Nuclear | 24 (32%) | 51(68%) |
| Family Size | 5 (SD=2) | 5 (SD=2) | .96 |
| Annual household income | 135235 (SD=91485) | 124303 (SD=126817) | .65 |
| Educational status | .79 |
| <High School | 13 (34%) | 25 (66%) |
| =High School | 7 (27%) | 19 (73%) |
| Intermediate (11th-12th grade) | 7 (41%) | 10 (59%) |
| Some college or above | 7 (37%) | 12 (63%) |
| Occupation | .26 |
| Professional | 7 (54%) | 6 (46%) |
| Skilled worker | 10 (37%) | 17 (63%) |
| Unskilled worker | 14 (26%) | 39 (74%) |
| Student | 3 (43%) | 4 (57%) |
| Age of smoking initiation | 22 (SD=4) | 21 (SD=6) | .75 |
| Number of filter sticks (n=74) | 9 (SD=5) | 9 (SD=4) | .95 |
| Number of Bidi sticks (n=27) | 15 (SD=9) | 21 (SD=8) | .07 |
| Total smoking costs, INR/Day | 47 (SD=35) | 51(SD=31) | .58 |
| Heard about nicotine curbing substance | .13 |
| Yes | 10 (48%) | 11 (52%) |
| No | 24 (30%) | 55 (70%) |
| Heard about nicotine deaddiction centre | .03 |
| Yes | 10 (56%) | 8 (44%) |
| No | 24 (29%) | 58 (71%) |
| Time required from home/office to reach nearest cigarette/Bidi vendor | 7 (SD=4) | 5 (SD=3) | .02 |
| Free smoking aid encourage to smoke more often | .18 |
| Yes | 7 (24%) | 22 (76%) |
| No | 27 (38%) | 44 (62%) |
| Accessibility to smoking products increases chances of smoking | .31 |
| Yes | 16 (30%) | 38 (70%) |
| No | 18 (39%) | 28 (61%) |
| Access to smoking products at workplace | .52 |
| Yes | 15 (29%) | 37 (71%) |
| No | 19 (40%) | 29 (60%) |
Limitations
The limitations of this study included a small sample and only male gender due to which gender differences could not be compared. Majority of the participants belonged to rural areas because of which urban differences could not be determined. Since it was a hospital-based study, extrapolation of the results to the wide population of current smokers may not be possible.
Conclusion
Work places may serve as an effective platform to deliver targeted strategies aimed at smoking cessation. Such strategies should include incentives, periodic health education informing the risks to them and their families and awareness about drug de-addiction centres. A review of national guidelines to regulate and evaluate the accessibility and availability of smoking products in and around the work place may be needed.
*Some response may not add up to 100 due to some of the participants smoke Bidi as well cigarette. Responses are in multiple scales
[1]. BA Sela, Time for setting a good example: physicians, quit smoking now. EditorialIsraeli Medical Association Journal 2013 15:379-81.http://www.ima.org.il/FilesUpload/IMAJ/0/60/30260.pdf (Accessed 15 Sep. 2014) [Google Scholar]
[2]. R West, Tobacco control: present and futureBritish Medical Bulletin 2006 77(1):123-36.doi:10.1093/bmb/ldl012 [Google Scholar]
[3]. A Binnal, G Rajesh, J Ahmed, Insights into smoking and its cessation among current smokers in IndiaAsian Pacific Journal of Cancer Prevention 2013 14(5):2811-18.doi:10.7314/APJCP.2013.14.5.2811 [Google Scholar]
[4]. R Jayakrishnan, A Mathew, A Uutela, Multiple approaches and participation rate for a community based smoking cessation intervention trial in rural Kerala, IndiaAsian Pacific Journal of Cancer Prevention 2013 14(5):2891-96.doi:10.7314/APJCP.2013.14.5.2891 [Google Scholar]
[5]. M Rani, S Bonu, P Jha, Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household surveyTobacco Control 2003 12(4):e4-e4.doi:10.1136/tc.12.4.e4 [Google Scholar]
[6]. SK Jindal, AN Aggarwal, K Chaudhry, Tobacco smoking in India: prevalence, quit-rates and respiratory morbidity Indian Journal of Chest Diseases and Allied Sciences 2006 48(1):37-11.http://smokelesscigarettestoday.net/goto/http://medind.nic.in/iae/t06/i1/iaet06i1p37.pdf (Accessed Nov. 2013) [Google Scholar]
[7]. Government of India (Ministry of Health and Family welfare), International Institute for Population Sciences, World Health Organization and Centres for Disease Control and Prevention. Global adult tobacco survey India (GATS India), 2009–2010. 2010. http://ww.searo.who.int/entity/tobacco/documents/2010-pub2.pdf (Accessed 29 Sep. 2014) [Google Scholar]
[8]. RM John, HY Sung, W Max, Economic cost of tobacco use in India, 2004Tobacco Control 2009 18(2):138-143.doi:10.1136/tc.2008.027466 [Google Scholar]
[9]. JD Sargent, ML Beach, AM Adachi-Mejia, Exposure to movie smoking: its relation to smoking initiation among US adolescentsPaediatrics 2005 116(5):1183-1191.doi:10.1542/peds.2005-0714 [Google Scholar]
[10]. JF Scherrer, H Xian, H Pan, Parent, sibling and peer influences on smoking initiation, regular smoking and nicotine dependence. Results from a genetically informative designAddictive Behaviours 2012 37(3):240-47.doi:10.1016/j.addbeh.2011.10.005 [Google Scholar]
[11]. Z Harakeh, WA Vollebergh, The impact of active and passive peer influence on young adult smoking: An experimental studyDrug and alcohol dependence 2012 121(3):220-223.doi:10.1016/j.drugalcdep.2011.08.029 [Google Scholar]
[12]. CC Reveles, NJ Segri, C Botelho, Factors associated with hookah use initiation among adolescentsJornal de pediatria 2013 89(6):583-587.doi:10.1016/j.jped.2013.08.001 [Google Scholar]
[13]. PD Jeganathan, NN Hairi, N Al Sadat, Smoking Stage Relations to Peer, School and Parental Factors among Secondary School Students in Kinta, PerakAsian Pacific Journal of Cancer Prevention 2013 14(6):3483-89.doi:10.7314/APJCP.2013.14.6.3483 [Google Scholar]
[14]. JL Elf, B Modi, F Stillman, P Dave, B Apelberg, Tobacco sales and marketing with in 100 yards of schools in Ahmedabad City, IndiaPublic Health 2013 127(5):442-48. [Google Scholar]
[15]. K Cahill, R Perera, Competitions and incentives for smoking cessation Cochrane Database of Systematic Reviews 2011 11:4doi:10.1002/14651858.CD004307.pub3 [Google Scholar]
[16]. P Aveyard, L Bauld, Incentives for promoting smoking cessation: what we still do not know Cochrane Database of Systematic Reviews 2011 7(1):8doi:10.1002/14651858.ED000027 [Google Scholar]
[17]. Centre for Disease Control and Prevention (CDC). Smoking and Tobacco Use. Adult Cigarette Smoking in the United States: Current Estimate 2012. http://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/ (Accessed Nov. 2013) [Google Scholar]
[18]. R Humeniuk, S Henry-Edwards, R Ali, The Alcohol, Smoking and Substance involvement Screening Test (ASSIST): manual for use in primary care 2010 http://whqlibdoc.who.int/publications/2010/9789241599382_eng.pdf. (Accessed Nov. 2013) [Google Scholar]
[19]. R McGee, WR Stanton, A longitudinal study of reasons for smoking in adolescenceAddiction 1993 88(2):265-71.doi:10.1111/j.1360-0443.1993.tb00810.x [Google Scholar]
[20]. LT Sichletidis, DA Chloros, AI Tsiotsios, Prevalence and risk factors for initiation of smoking in Greek high-school studentsInternational Journal of Environmental Research and Public Health 2009 6(3):971-79.doi:10.3390/ijerph6030971 [Google Scholar]
[21]. N Kumar, N Gupta, J Kishore, Kuppuswamy’s socioeconomic scale: updating income ranges for the year 2012Indian Journal of Public Health 2012 56(1)doi:10.4103/0019-557X.96988 [Google Scholar]
[22]. CJ Murray, AD Lopez, Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease StudyThe Lancet 1997 349(9064):1498-1504.doi:10.1016/S0140-6736(96)07492- [Google Scholar]
[23]. R Narain, S Sardana, S Gupta, Age at initiation & prevalence of tobacco use among school children in Noida, India: A cross-sectional questionnaire based surveyIndian Journal of Medical Research 2011 133(3):300-07.http://icmr.nic.in/ijmr/2011/march/0309.pdf (Accessed Nov. 2013) [Google Scholar]
[24]. T Use, Tobacco use among children in India: A burgeoning epidemicIndian Pediatrics 2005 42:757-61.http://www.indianpediatrics.net/aug2005/aug-757-761.htm (Accessed Nov. 2013) [Google Scholar]
[25]. RA Al-Naggar, AA Jawad, YV Bobryshev, Prevalence of cigarette smoking and associated factors among secondary school teachers in MalaysiaAsian Pacific Journal of Cancer Prevention 2012 13:5539-43.doi:10.7314/APJCP.2012.13.11.5539 [Google Scholar]
[26]. UM Bhojani, SJ Chander, N Devadasan, Tobacco use and related factors among pre-university students in a college in Bangalore, IndiaThe National Medical Journal of India 2009 22(9):294-97.http://imsear.hellis.org/bitstream/123456789/139083/1/nmji2009v22n6p294.pdf (Accessed Nov. 2013) [Google Scholar]
[27]. KG Volpp, AB Troxel, MV Pauly, A randomized, controlled trial of financial incentives for smoking cessationNew England Journal of Medicine 2009 360(7):699-709.doi:10.1056/NEJMsa0806819 [Google Scholar]