Nasopalatine Duct Cyst Associated with a Mesiodens: Misdiagnosis or Missed Diagnosis?
Deepika Gopal1, Ajay Telang2, Lahari A. Telang3, Kamaraj Loganathan4, B. Thirupathi Reddy5
1 Assistant Professor, Department of Oral Pathology, Penang International Dental College, Malaysia.
2 Associate Professor, Department of Oral Pathology, Penang International Dental College, Malaysia.
3 Associate Professor, Department of Oral Medicine and Radiology, Penang International Dental College, Malaysia.
4 Associate Professor, Department of Oral & Maxillofacial Surgery, Penang International Dental College, Malaysia.
5 Assistant Professor, Department of Prosthetic Dentistry, Penang International Dental College, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepika Gopal, Penang International Dental College, NB Tower, Level 18-21, 5050 Jalan Bagan Luar, 12000 Butterworth, Penang, Malaysia.
E-mail: drdeepikagopal@gmail.com
Nasopalatine duct cyst ( NPDC) is described as most common non-odontogenic developmental cyst of the jaws. Despite being common, its clinical and radiographic presentation could be varied and it can sometimes be a diagnostic challenge. This paper presents an unusual case of an infected NPDC associated with an impacted inverted mesiodens and a history of trauma that misled the clinical diagnosis.
Cone beam computed tomography, Impacted tooth, Non odontogenic cyst
Case Report
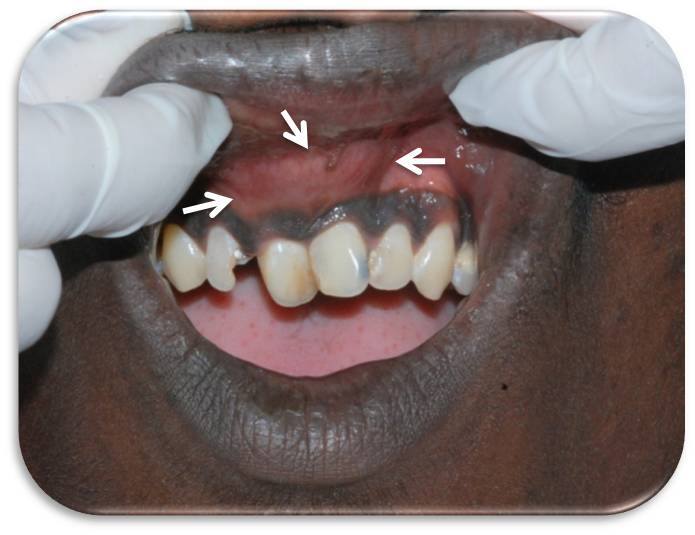
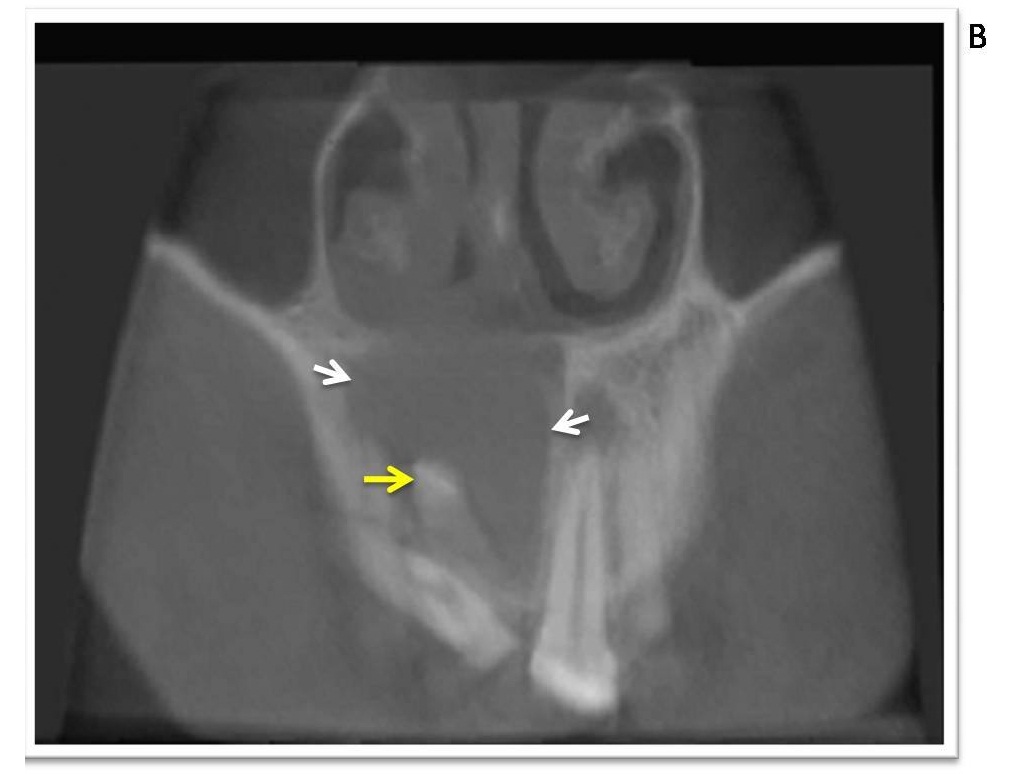
An 18-year-old boy reported with complaint of swelling and recurrent episodes of pus discharge in relation to upper front teeth for six months. He gave a history of trauma to the upper front teeth three years ago for which he underwent treatment, the nature of which was unsure. He was apparently alright until six months ago when he noticed a slow growing swelling of the upper lip that was painful. On examination a diffuse swelling was seen involving the entire upper lip extending to the right ala of nose. The lesion was warm, tender, fluctuant and firm on palpation. [Table/Fig-1] shows the intraoral swelling involving the maxillary labial vestibule, about 3x2 cm in size with overlying normal mucosa. The maxillary right central incisor (11) was distally tilted, maxillary right lateral incisor (12) had a palatal temporary restoration and maxillary left central incisor (21) had proximal caries. 11 and 21 were positive for Electric Pulp Testing. Radiographs showed an impacted, inverted mesiodens present within a large well defined radiolucency about 3x2cm in size, extending from the apex of 12 to the apex of 21 [Table/Fig-2a,2b].
Intraoral swelling involving the maxillary labial vestibule, about 3x2 cm in size with overlying normal mucosa
Intraoral periapical radiograph showing a impacted and inverted mesiodens (yellow arrow) within a well defined radiolucency about 3x2cm in size (white arrows);
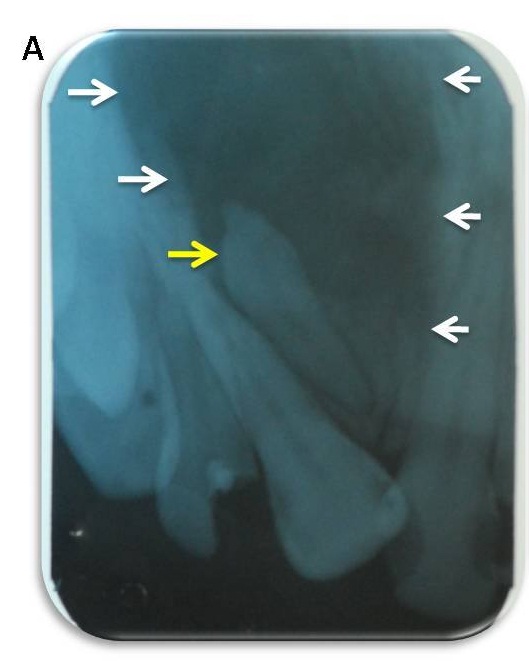
Occlusal view which showed the inverted mesiodens (yellow arrow) within the radiolucency
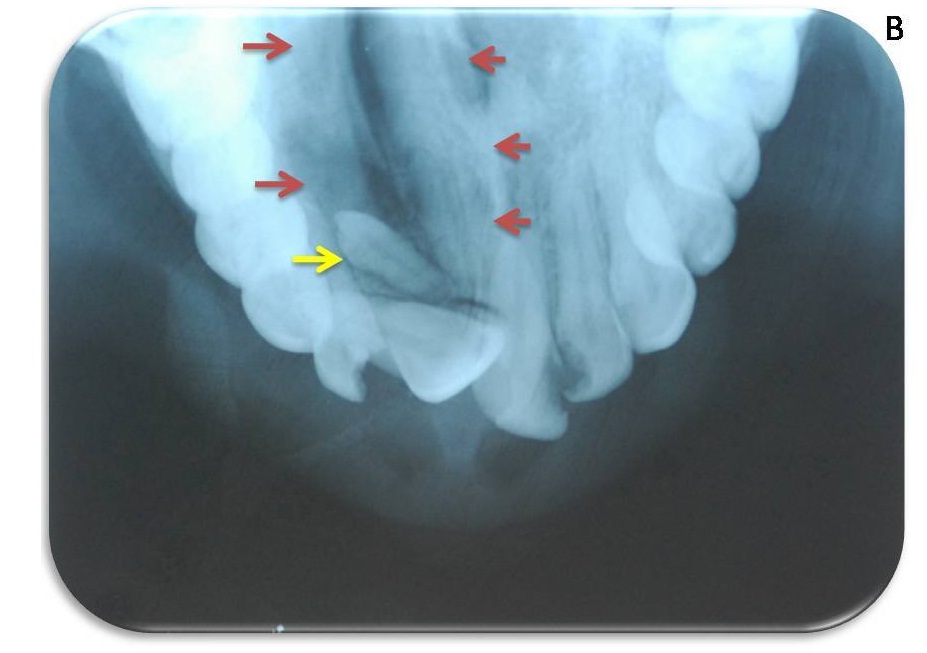
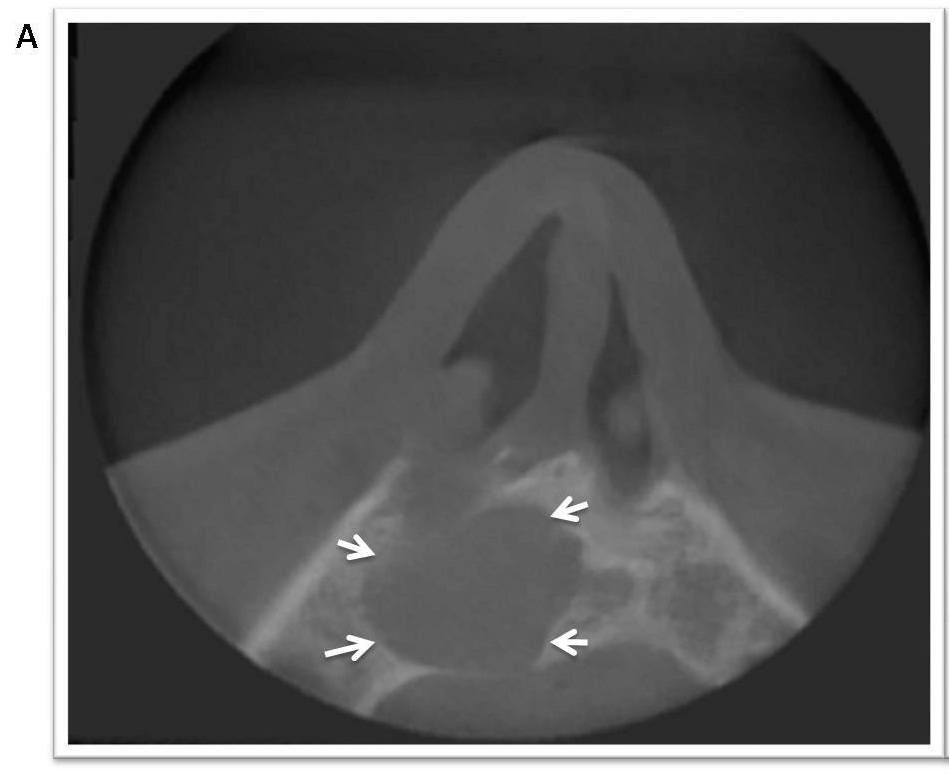
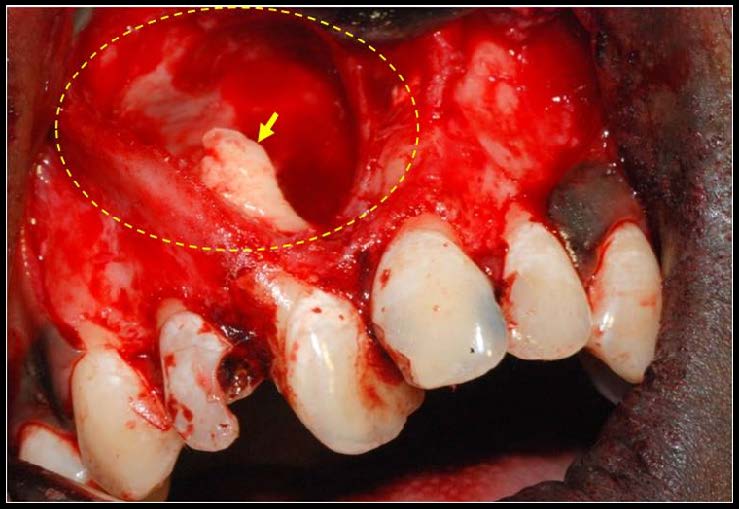
A provisional diagnosis of Dentigerous cyst associated with a mesiodens was made. Aspiration of the swelling was negative. A Cone beam computed tomography (CBCT) advised, helped to plan treatment and to define the initial diagnostic hypothesis. The various sections and views revealed its association with the mesiodens and the precise extent of the lesion which was from 12 to 22, encroaching the nasal floor and having regular margins [Table/Fig-3a,b]. Surgical enucleation and removal of mesiodens was planned. A vestibular approach was carried out as the swelling was more prominent on the labial aspect and the supernumerary tooth was easier to approach. A trapezoidal flap was raised involving 13 to 23, mesiodens was removed and cystic cavity curetted, irrigated & specimen sent for histopathological analysis. [Table/Fig-4] shows the cystic cavity and the mesiodens.
CBCT Axial section shows the precise extent of the lesion and well defined margins (white arrows);
CBCT Coronal section shows the lesion encroaching the nasal floor & impacted inverted mesiodens (yellow arrow) within the radiolucency (white arrows)
Shows the surgical cystic cavity and the inverted mesiodens (yellow arrow)
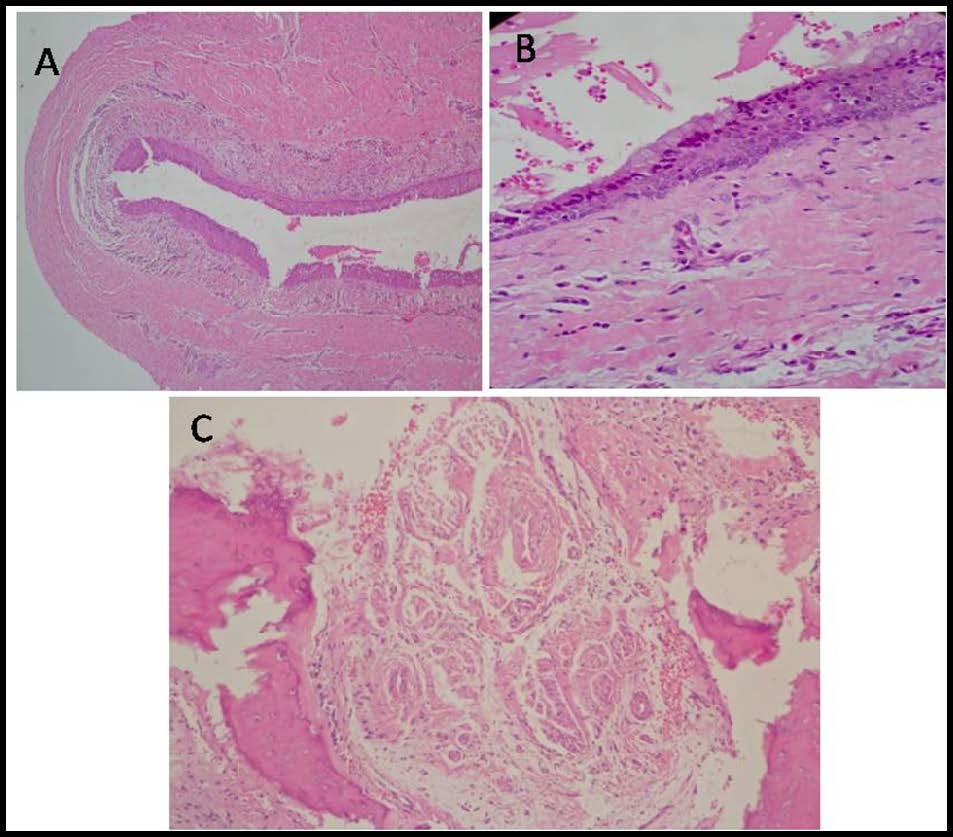
The patient was reviewed after a week and healing was satisfactory with no parasthesia or pain. Histopathology revealed the presence of a cystic tissue lined by pseudostratified ciliated columnar epithelium, low cuboidal epithelium and few areas of stratified squamous non keratinized epithelium [Table/Fig-5a,b]. The fibrous capsule showed varying sizes of nerve bundles and blood vessels as well as presence of acute and chronic inflammatory cells mainly plasma cells, lymphocytes and mast cells [Table/Fig-5c]. Based on clinical, radiological and histopathological features a diagnosis of an infected NPDC associated with impacted inverted mesiodens was made.
Histopathology sections - 5A: Section showing cyst lumen, cyst lining and capsule. (H&E stain, original magnification, 4X); 5B: Pseudo stratified columnar lining epithelium with goblet cells. (H & E stain, original magnification, 10X); 5C: Neurovascular bundles in the wall of nasopalatine duct cyst (H & E stain, original magnification, 10X)
Discussion
Nasopalatine duct cyst (NPDC) is a non odontogenic cyst of developmental origin which represents 1% of all cysts in the maxilla [1]. It was first described by Meyer in 1914 as an accessory paranasal sinus [2]. The term NPDC is now preferred to the synonymous ‘incisive canal cyst’ because it may occur within the nasopalatine canal or in the soft tissues of the palate or, at the opening of the canal [3]. Most cases occur in the third to the sixth decades but some have also been reported in the first decade [4]. The frequency of NPDC is more in males than in females. The exact pathogenesis of this lesion is still unclear but is believed to arise from the remnants of nasopalatine duct triggered by trauma or infection. Tsuneki et al., [5] in their study on 41 cases of NPDC concluded the two possible histopathogenesis to be inflammatory like radicular cyst or salivary duct cyst like mucocoele. In our case the patient gave a history of chronic infection of permanent maxillary incisors secondary to trauma suggesting it as a possible trigger.
The other aspect of the case is the presence of a mesiodens which is a supernumerary tooth reported in literature with a higher Asian prevalence [4]. These teeth either erupt or remain impacted and can often cause problems such as malocclusion or give rise to tumors or cysts. Common cysts associated with impacted teeth are dentigerous cyst and odontogenic keratocyst [6]. NPDC associated with impacted mesiodens is rare with only two reported cases at the time of writing this report [7,8].
There are various reports on misdiagnosis of NPDC with or without association to trauma. One such case was reported by Gulabivala & Briggs [9] where the case was initially diagnosed as a periapical abscess because of its unusual presentation but later found to be an infected NPDC. Vitality testing of incisors is important to differentiate NPDC from a periapical lesion [3]. In this case differential diagnoses of dentigerous cyst & radicular cyst were made based on the clinical and imaging studies. This is needed to prevent unnecessary interventions like endodontic treatment in vital teeth. To establish a confirmed diagnosis histopathology is the key .An important diagnostic feature in NPDC is the presence of blood vessels and nerves in the fibrous capsule [3]. Our case showed all features consistent with the presence of acute and chronic inflammatory cells which helped to confirm the diagnosis.
Thus, in this case, the question that comes to mind is did trauma trigger the formation of the cyst or did it get secondarily infected? Either ways this case clearly mimics a lesion of endodontic origin. Treatment in all cases involves complete surgical enucleation as early as possible. A recurrence rate of 11-30% has been reported by various authors [1,7,10]. Our patient is on follow up and shows no recurrence one year post treatment.
Conclusion
This report presents a rare infected NPDC associated with an impacted inverted mesiodens. The importance of this case is that the lesion was associated with a history of trauma and impacted mesiodens causing a diagnostic dilemma. It could have been misdiagnosed as a periapical cyst because of history of trauma or misdiagnosed as a dentigerous cyst because of an associated impacted mesiodens, but histopathological examination helped to establish the diagnosis. Hence a triangular approach of clinical, radiological and histopathological correlation is imperative for a definitive diagnosis, also, NPDC should be considered as a differential diagnosis in a radiolucent lesion associated with impacted mesiodens.
[1]. Swanson KS, Kaugars GE, Gunsolley JC, Nasopalatine duct cyst: an analysis of 334 casesJ Oral Maxillofac Surg 1991 49(3):268-71. [Google Scholar]
[2]. Meyer AW, Spolla Anatomica: Unique Supernumerary Para-Nasal Sinus Directly Above Superior IncisorsJ Anat & Physiol 1914 48:118-20. [Google Scholar]
[3]. Shear M, Speight PM, Cysts of the Oral and Maxillofacial Regions 2007 4th ednOxfordBlackwell Munksgaard:108-18. [Google Scholar]
[4]. Velasquez-Smith MT, Mason C, Coonar H, Bennett J, A nasopalatine cyst in an 8-year-old childInt J Paediatr Dent 1999 9(2):123-27. [Google Scholar]
[5]. Tsuneki M, Maruyama S, Yamazaki M, Inflammatory histopathogenesis of nasopalatine duct cyst: a clinicopathological study of 41 casesOral Dis 2013 19:415-24. [Google Scholar]
[6]. Rajab LD, Hamdan MA, Supernumerary teeth: Review of the literature and a survey of 152 casesInt J Paediatr Dent 2002 12:244-54. [Google Scholar]
[7]. Tariq Salamm AR, Parthiban Vijay, Karpagam Gopinath R, Extensive Nasopalatine Duct Cyst Causing Nasolabial ProtrusionIndian Journal of Multidisciplinary Dentistry 2011 1(5):285-88. [Google Scholar]
[8]. Bereket C, Kaynar M, Nasopalatine Duct Cyst Concurrent With Supernumerary Tooth: A Case ReportJ Dent Fac Atatürk Uni 2013 23(1):98-102. [Google Scholar]
[9]. Gulabivala K, Briggs PF, Diagnostic dilemma: an unusual presentation of an infected nasopalatine duct cystInt Endod J 1992 25:107-11. [Google Scholar]
[10]. Francolí JE, Marqués NA, Aytés LB, Escoda CG, Nasopalatine duct cyst: report of 22 cases and review of the literatureMed Oral Patol Oral Cir Bucal 2008 13(7):E438-E43. [Google Scholar]