Orofacial pain (OFP) is one of the most common regional pain syndromes. The term OFP consists of two parts: facial and oral. Facial pain includes pain that originates below the orbitomeatal line, above the neck and anterior to the ears while oral pain indicates pain within the mouth [1]. Heterogeneous group of disorders come under chronic Orofacial Pain that are characterized by ongoing pain in the head and face region [2].
It is now generally recognized that psychological factors play an important role in chronic pain [3,4]. Hypotheses have been proposed relating to the childhood origins of increased levels of psychological distress, to adult psychiatric illness [5]. Quality of Life is the perception that people have of life taking into account their cultural and values context in which they live [6]. World Health Organization described Quality of life as “an individual’s perception of their position in life in the context of the culture and value system of which they live with the relation to their goals, expectations, standards and concerns” [7]. Measures of oral health related quality of life capture non clinical aspects of oral health that patients seem most relevant to their overall health and wellbeing. These are increasingly used in descriptive population based research for the same [8]. Patients who report Orofacial Pain are hypothesised to have a poorer perception of their oral health-related quality of life
This study aims to examine the hypothesis that psychological factors of Psychological Distress and retrospective perception of unhappiness in childhood are associated with self reported Orofacial Pain and whether such patients have a poorer perception of their oral health related quality of life.
Materials and Methods
Study Group and Design
A cross-sectional hospital based study was conducted amongst a random sample of 800 patient’s aged 18-65 yrs attending the outpatient department of Hitkarini Dental College and Hospital, Jabalpur. A detailed case history was recorded and thorough clinical examination was performed by oral medicine specialists. Patients were informed about the study and written consent was obtained. From November 2013 to November 2014, 400 patients with Orofacial Pain were examined against age, sex and socioeconomic status matched 400 pain free controls.
The control group comprised of 400 subjects who gave no history of pain and who were age sex and socio-economic status matched with the case group. Patients were included in the study group based on following inclusion and exclusion criteria.
Inclusion Criteria
Patients were included based on the main question concerning Orofacial Pain which included various types of pain experienced over the past month at any moment. Orofacial Pain was defined as present if the respondent had experienced pain during the past month in at least one of the following:
In the jaw joint/s
In the area just in front of the ear/s
In or around the eyes; when opening the mouth wide
In the jaw joint when chewing food
In and around the temples
If there had been tenderness of muscles at the side of the face
If there had been prolonged burning sensation in the tongue or other parts of the mouth
If there had been shooting pain in the face or cheeks (Locker & Slade) [9].
Exclusion Criteria
Following patients were excluded:
Patients who refused to undergo the examination or complete the questionnaire
Patients with history of TMJ surgery or head and neck radiation treatment
Patients with history of head and neck trauma in past two months
Patients who were pregnant
Patients under medications like narcotic analgesics, muscle relaxants or corticosteroids whose treatment could not be suspended one week prior to the study
Patients under antidepressants and NSAIDs at least three days prior to the study
Drug-dependent patients [10].
All the patients were informed about the examination and were asked to complete a 27 items questionnaire in accordance with the norms and guidelines approved by the ethical committee of Hitkarini Dental College and Hospital. This 27 items questionnaire was made up of 12 items general health questionnaire, 14 items oral health impact profile questionnaire and a question on Happy Childhood. These questionnaires were converted into the regional language (Hindi) which was validated by distribution of the same amongst linguistic experts.
Participants completed the 12-item general health questionnaire (GHQ-12) (Goldberg), as the measure of Psychological Distress. This self complete questionnaire was used to identify the recent onset of symptoms of Psychological Distress. It concentrates on two main areas: inability to continue normal functions and the appearance of new problems of a distressing nature, and is a screening instrument for mental disorders. Each item within the questionnaire consists of asking the subject whether they have recently (during the past few weeks) experienced a particular symptom, on a 4-point likert scale [5]. In the view that psychological stress in adult life is influenced by childhood experience, a question about a happy childhood was also included in the questionnaire.
For the qualitative analysis of self-perceived oral health in patients with Orofacial Pain oral health impact profile questionnaire (OHIP) questionnaire was used. The 49 item oral health impact profile questionnaire was developed and validated by Slade and Spencer and contains 49 questions that capture the seven dimensions of Locker’s theoretical model of oral health [10]. The OHIP-14 items, a short form of the OHIP-49 items consists of 2 items for each of the 7 subscales in the source instrument (functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap). Items are scored on a Likert-type frequency scale, as follows: never, hardly ever, occasionally, fairly often and very often (coded 0 through4, respectively) [11].
Statistical Analysis
Frequency, percentages, mean, standard deviation (SD), and median values of variables in case and control groups were calculated. Further data analysis was done using Pearson’s Chi-Square Test, Unpaired t-Test, Mann-Whitney U-test and Binomial Logistic Regression (Odds Ratio). P-values <0.05 were considered statistically significant. Data analysis was done using Statistical Package for Social Sciences (SPSS) v.21
Results
The study was conducted on age, sex and socio-economic status matched 400 cases and 400 controls. The mean age of the participants in the study group was 39 (SD ± 10) years, of whom 51.5% were males and 48.5% were females. The mean age of the participants in the control group was 40 (SD ± 7) years, of whom 55.2% were males and 44.8% were females.
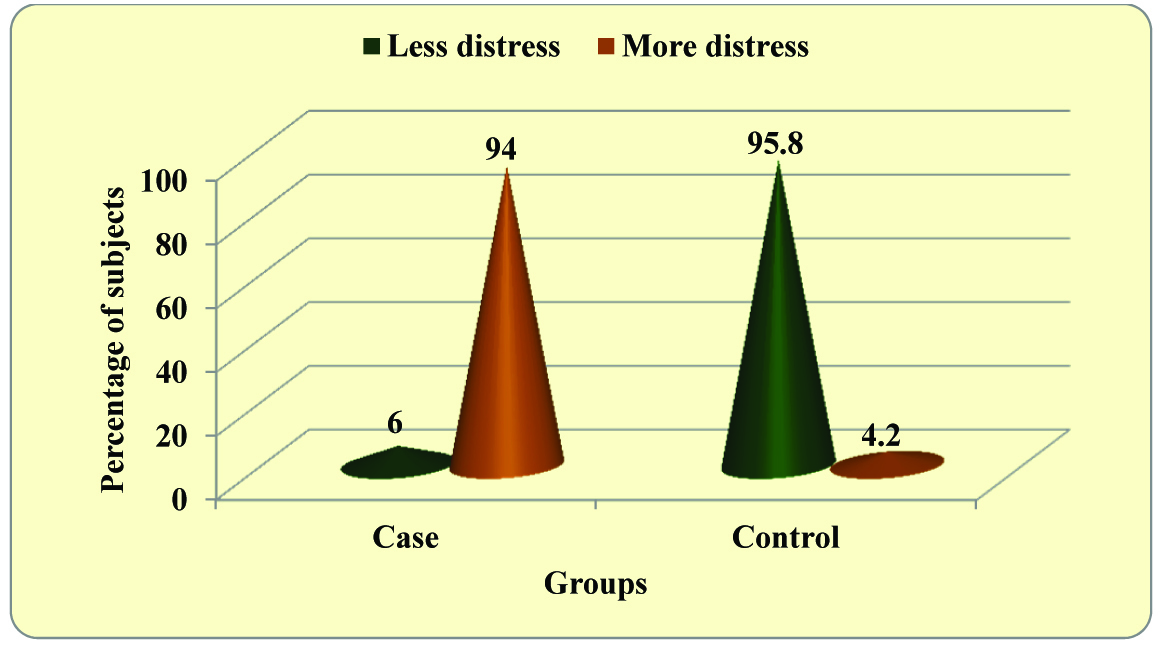
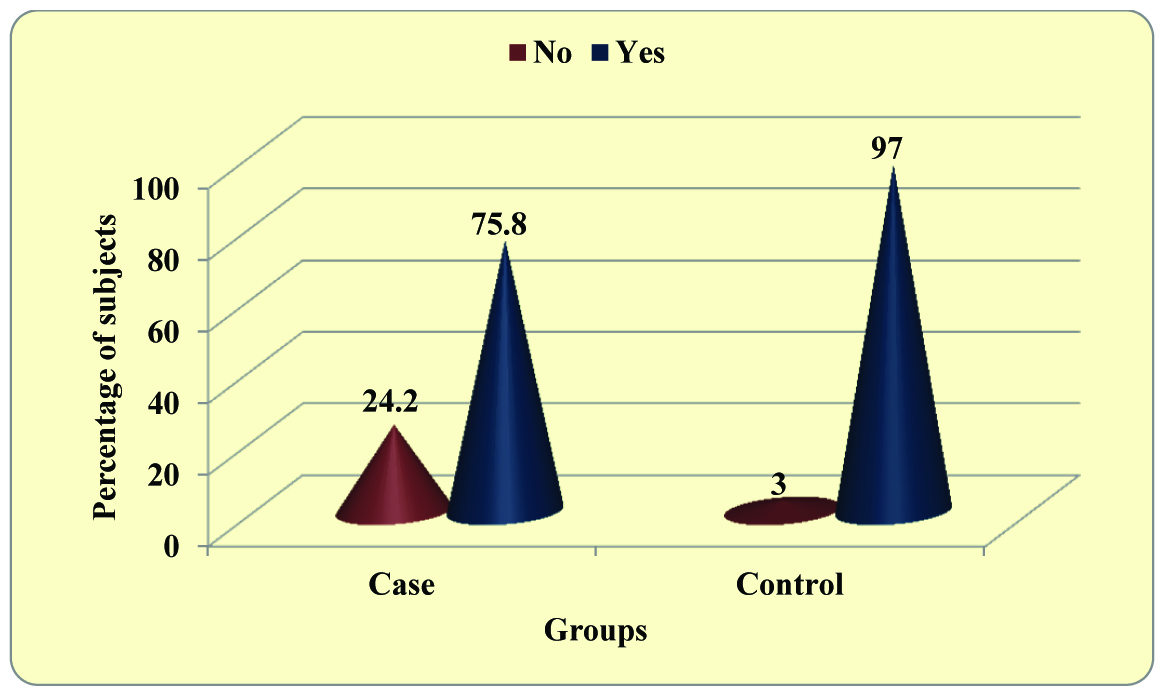
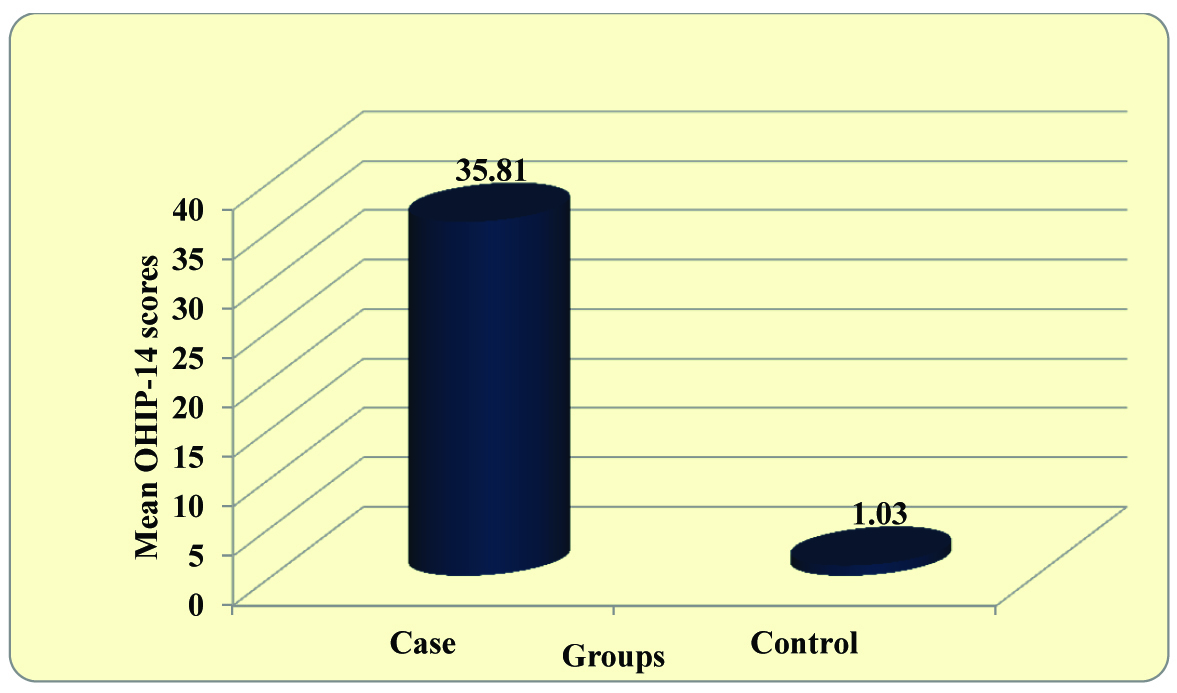
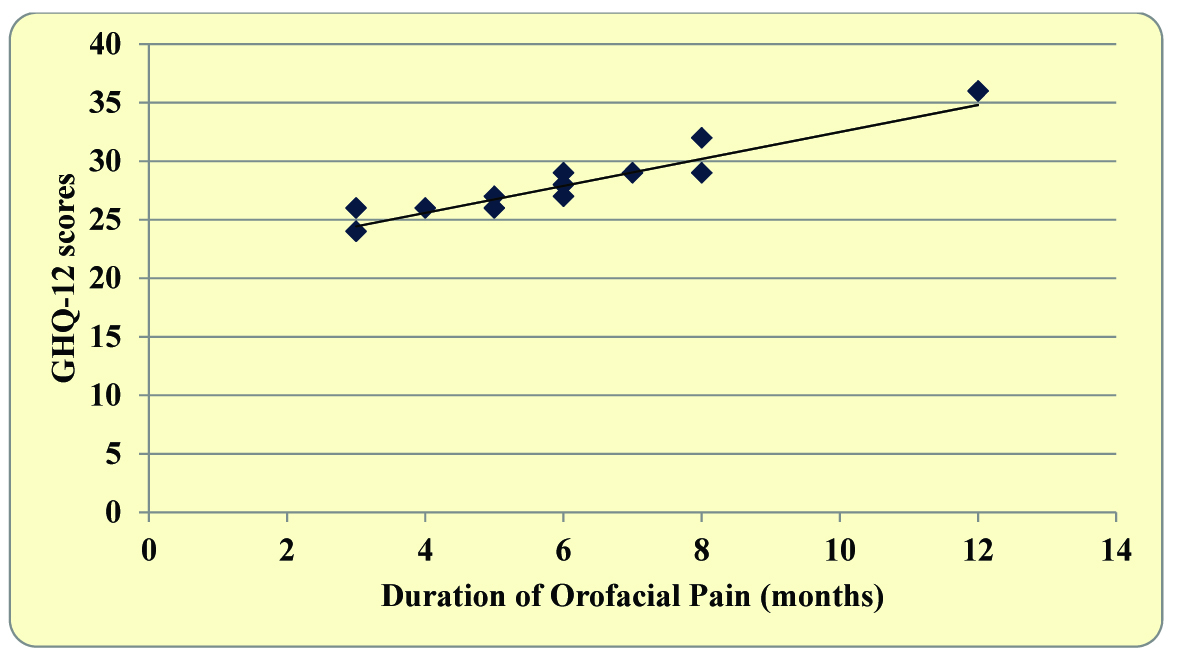
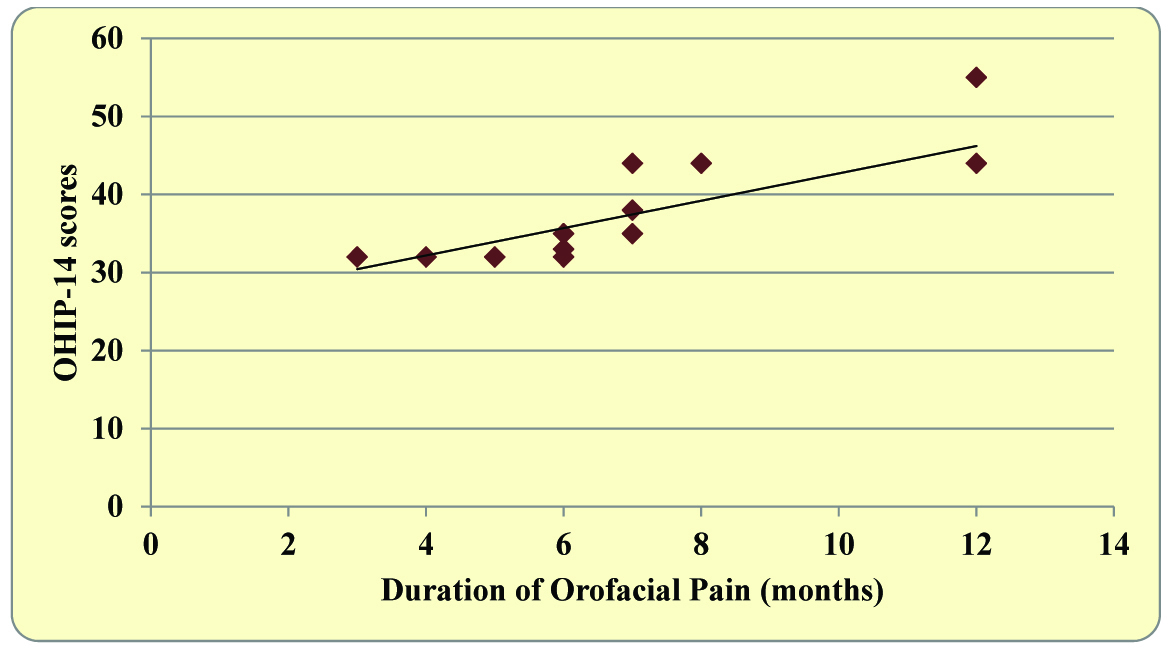
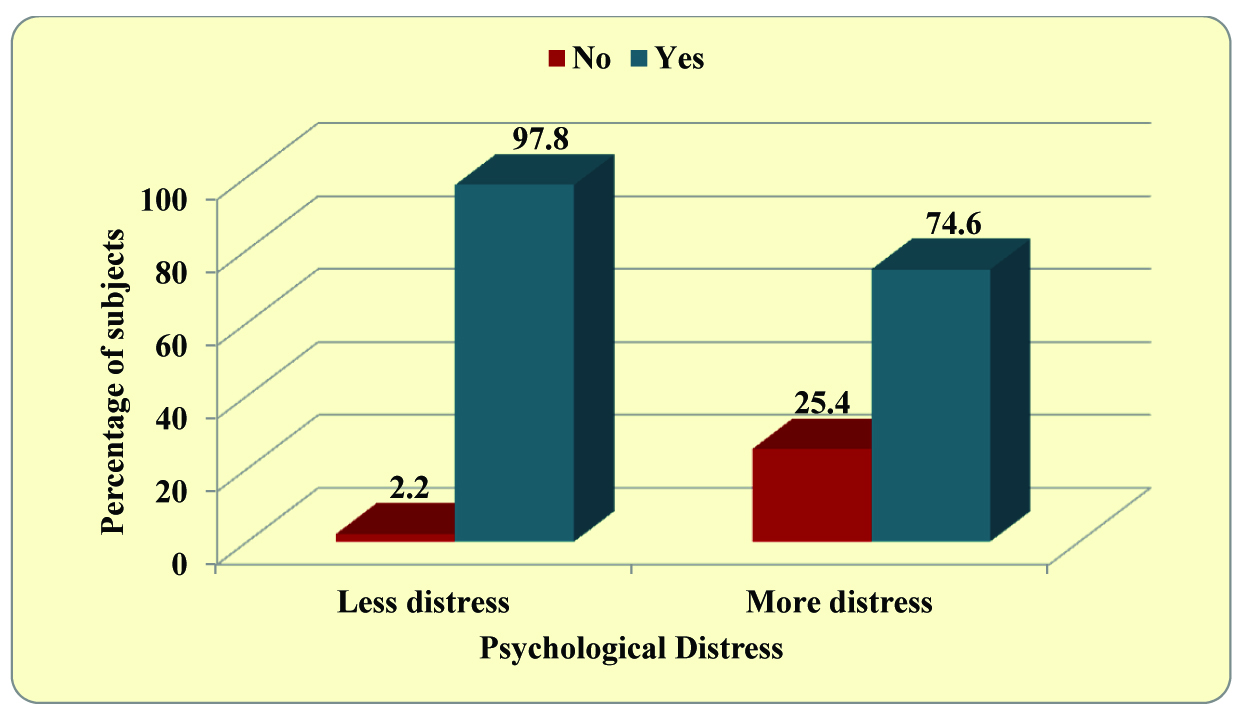
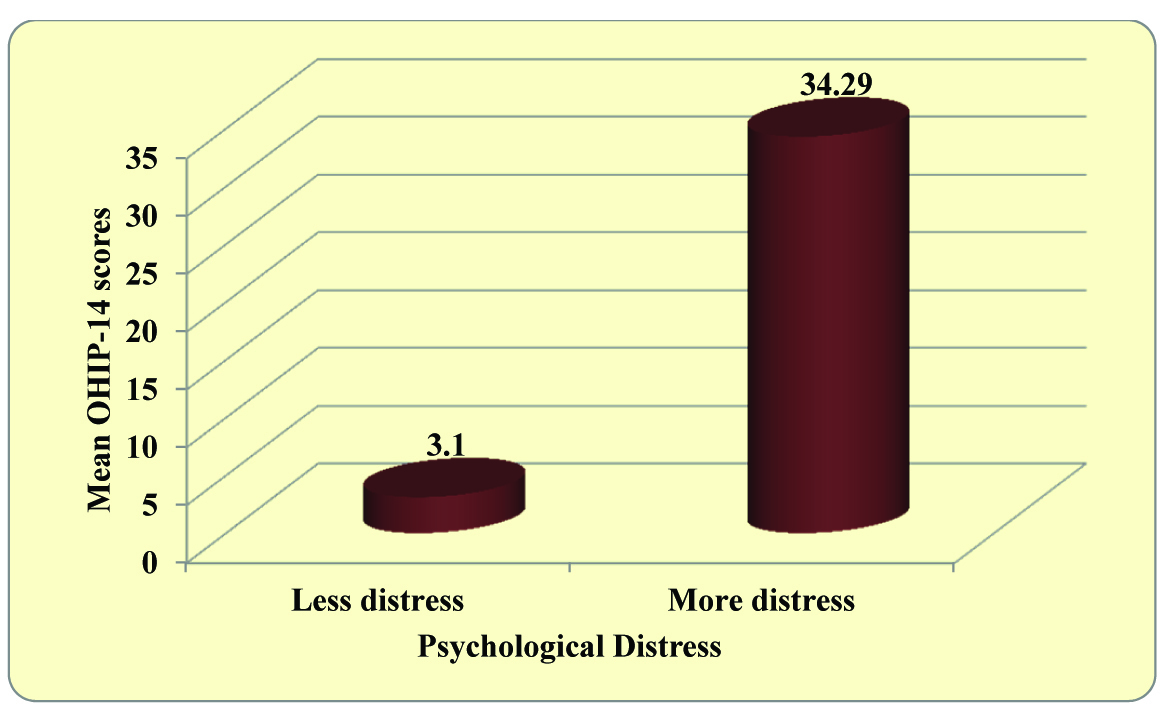
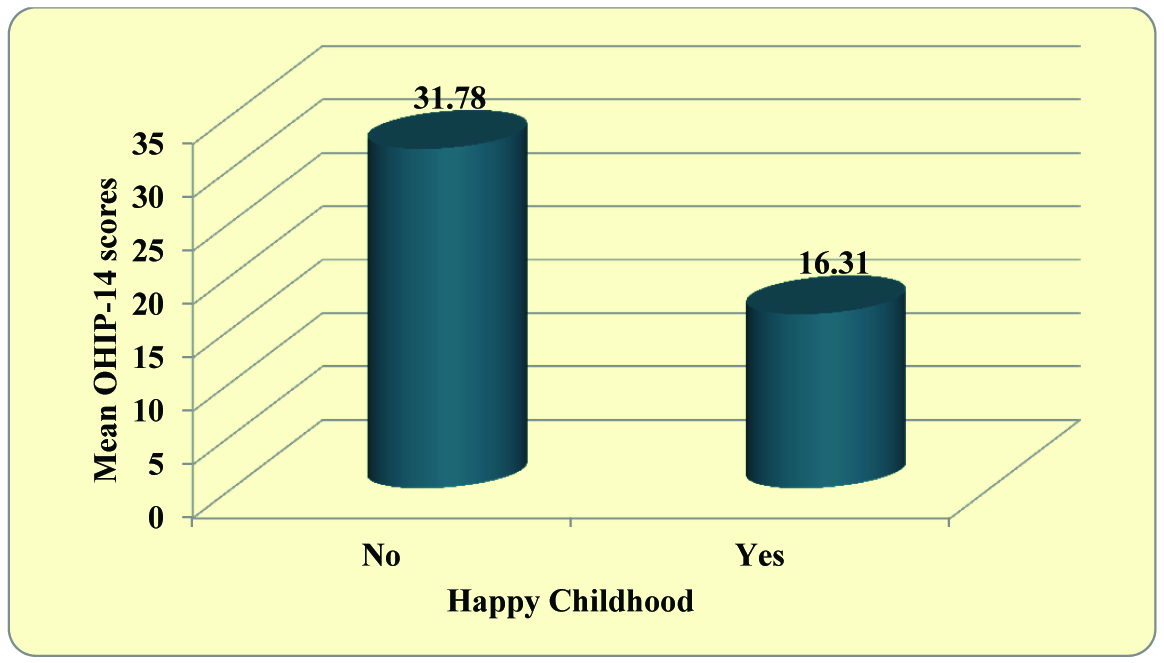
Based on GHQ scores, compared to less distress subjects, psychologically more distressed subjects were having 367.56 times higher odds for oro-facial pain [Table/Fig-1]. In the study group 24.2% of the subjects gave a history of an unhappy childhood whereas similar history was given by 3% of the subjects in the control group. Compared to subjects with Happy Childhood, Unhappy subjects were having 10.00 times higher odds for Orofacial Pain [Table/Fig-2]. Significant difference between Orofacial Pain cases and controls was seen for OHIP-14 scores in which cases had higher scores compared to the controls [Table/Fig-3]. Amongst the participants in the study group, it was seen that with increase in duration of pain, Psychological Distress became more and quality of life became worse [Table/Fig-4,5]. Significant difference was seen statistically between Psychologically Distressed subjects for Happy and Unhappy Childhood [Table/Fig-6]. More Distressed subjects gave higher OHIP scores [Table/Fig-7]. Higher OHIP scores were also given by subjects with a history of an unhappy childhood [Table/Fig-8].
Comparison of Orofacial Pain (cases and controls) according to Psychological Distress (GHQ-12)
Comparison of Orofacial Pain according to Happy Childhood
Comparison of OHIP-14 scores in Orofacial Pain cases and controls
Correlation of duration of Orofacial Pain with GHQ-12 scores among cases of Orofacial Pain (n=400)
Correlation of duration of Orofacial Pain with OHIP-14 scores among cases of Orofacial Pain (n=400)
Comparison of Happy or Unhappy Childhood according to levels of Psychological Distress (GHQ-12)
Comparison of OHIP-14 scores in different levels of Psychological Distress (GHQ-12)
Comparison of OHIP-14 scores according to Happy and Unhappy Childhood
Discussion
The epidemiological data produced in this study stimulate potentially important hypotheses about the cause-and-effect relationships between levels of Psychological Distress and current perceptions of Orofacial Pain both of which could be affected by childhood events, and further discusses the impact of both on quality of life of the individual. The most obvious two possibilities with Orofacial Pain and Psychological Distress are either that the pain itself may produce the distress or that the existence of the Psychological Distress, whatever the cause, may lead to a high level of perception or reporting of Orofacial Pain.
The work of Melzack and Wall suggested that emotional state can influence the perception of pain and cause individuals to develop new symptoms. Recent evidence has suggested that psychological problems can manifest as somatic symptoms, sometimes referred to as ‘masked depression’ or in extreme cases, somatisation and these symptoms are not restricted just to the face [5]. Although pain has many adaptive qualities in regard to physical insult/injury or pathology, for some individual’s persistent pain in the presence or absence of organic pathology becomes a source of significant personal distress and life disruption. There is considerable evidence that psychological processes are operative in the experience of Orofacial Pain. In fact, research indicates that psychopathological disorders are common among Orofacial Pain patients [12].
GHQ questionnaire is a self complete questionnaire to assess levels of Psychological Distress. A positive association was seen between Psychological Distress and Orofacial pain in the present study. Patients with higher levels of Psychological Distress showed increased chances of self reported Orofacial Pain. Similar results have been obtained in other studies [5,13–18].
Stanfield et al., in their cross-sectional study investigated association between physical and psychological morbidity and reported that overall health status and self-reported physical symptoms were strongly associated with psychiatric disorder (measured using GHQ questionnaire), and suggested that psychiatric disorder is likely to be secondary to the pain [19]. Hotopf et al., found that there is a relationship between psychological distress and pain, which appears to operate both ways. The study showed that presence of psychiatric disorder increased the odds of experiencing physical symptoms and that multiple physical symptoms were a powerful indicator of psychiatric disorder [20].
A statistically significant difference was evident amongst Orofacial Pain subjects with a history of an Unhappy or a Happy Childhood. Subjects with Unhappy Childhood demonstrated increased chances of self reported Orofacial Pain. Assuming that adverse childhood events determine the happiness of childhood, the results support the findings of other studies. Similar results were given by Macfarlane et al., in their cross-sectional study which showed that participants who reported of an Unhappy Childhood had an increased risk of reporting Orofacial Pain compared to those with a Happy Childhood [5]. Hypotheses have been proposed relating to the childhood origins of increased levels of Psychological Distress, to adult psychiatric illness [21–23], and fibromyalgia in patients attending clinic [24,25]. In addition, somatisation, which is also associated with reports of adverse childhood events, has also been associated with fibromyalgia [5]. It has also been demonstrated that reports of adverse events in childhood, such as the separation or death of parents or abuse, and perceived paternal overprotection, or lack of care are strongly associated with a high tender point count (McBeth et al.,) [26].
Oral diseases which are not usually fatal, contribute to ones’ general wellbeing by affecting the ‘ability to eat, speak and socialize without active disease or embarrassment. Oral disorders can greatly affect interpersonal relationships and daily activities, and hence the ‘goodness’ or ‘quality of life’. The impact of oral diseases on the quality of life is very obvious. The general quality of life would be adversely affected by any disease that could interfere with the activities of daily life. Observations and research about the impact of oral diseases on different aspects of life lead to the development of the notion of oral health-related quality of life [8].
Measures of subjective oral health such as single-item self-ratings of oral health and self-perceived need for dental treatment and multi-item, multidimensional scales such as the Geriatric Oral Health Assessment Index, the Oral Health Impact Profile and the Child Oral Health Quality of Life Questionnaires are now widely employed in oral health research. These measures help in documentation of the functional and psychosocial impacts of oral disorders. Issues such as pain, problems with eating and sleeping, concerns about appearance and difficulties in social situations are also assessed [11]. People’s perceptions of the social impact of oral disorders on their well-being are measured by the Oral Health Impact Profile (OHIP). The OHIP-49 contained 49 questions which capture seven conceptually formulated dimensions based on Locker’s theoretical model of oral health. This was adapted from the WHO framework used to classify impairments, disabilities and handicaps. The OHIP-14 was developed as a shorter version of the OHIP especially for settings where the full battery of 49 questions seemed to be inappropriate [27].
Patients with self reported Orofacial Pain demonstrated higher OHIP scores. Similar results were seen by Montero et al., in a sample of adults in Granada, Spain [28]. Barros VM et al., concluded in their study that all individuals with Orofacial pain showed some impact related to physical pain [29]. Geerten-Has E Tjakkes et al., in their study concluded that in Orofacial pain patients, social functioning appears to be considerably affected [7].
Luo Y et al., also correlated Psychological Distress, Orofacial Pain and Quality of Life and concluded that mean OHIP-14 summary score was significantly higher in Orofacial Pain subjects than controls. GHQ scores of > or = 4, indicating greater psychological distress, were more common in Orofacial Pain subjects than controls. In their study Orofacial Pain had a substantial detrimental impact on daily life activities, psychological distress level, and quality of life [17].
Several newer findings were elicited by this study. Amongst the participants in the study group, GHQ-12 scores (Psychological distress) and OHIP-14 scores were directly proportional with the duration of pain. It was seen that with increase in duration of pain, Psychological Distress became more and quality of life became worse. This shows that as the chronicity of the pain increases, so does increases the stress levels of the patient which inturn affects the psychosocial and functional capabilities of the individual. Aguilera AB et al., in their study also demonstrated that increased OHIP scores were seen with chronic pain subjects [10]. Also, amongst the study group, subjects with higher levels of Psychological Distress had more number of participants with a history of an Unhappy Childhood. This indicates towards childhood origins of increased levels of Psychological Distress which could have a bimodal association with Orofacial Pain. Subjects with an Unhappy Childhood could be more sensitized for self reported Orofacial Pain, because of increased stress levels, or could be more stressed because of their high tender point count for Orofacial Pain. The study group also showed that patients with higher levels of Psychological Distress and those with a history of an Unhappy Childhood demonstrated increased impairment of their physical, social and functional activity. This further confirms the association that increased self reported Orofacial Pain, be it because of childhood events or because of increased stress demonstrates increased effect on the quality of life of the patient.
Conclusion
The present study has shown positive relationship between Orofacial Pain, quality of life and psychological factors. If we assume that the Psychological Distress leads to a high level of perception or Orofacial Pain, which further deteriorates the oral health related quality of life in such patients, then the presentation of Orofacial Pain could be considered as a specific variant of somatization which might in principle be amenable to psychological therapeutic intervention. The assumption that the pain itself may produce the distress should not however be seen as ruling out the relevance of psychological interventions, and a combined dental/psychological intervention might be appropriate in which a proper childhood history should be taken heed of. In either case a combined dental/psychological assessment process catering to childhood origin of stress, even if not, intervention is probably going to be needed for those individuals for whom the intensity or duration of their Orofacial Pain produces a continuing interference in their day to day activities.