Bindi Tuberculosis – Lupus Vulgaris Associated with Bindi Use: A Case Report
Gyanshankar Mishra1, Sushil Rathi2, Jasmin Mulani3
1 Assistant Professor, Department of Chest & TB, Government Medical College, Nagpur, India.
2 Assistant Professor, Department of Dermatology, Government Medical College, Nagpur, India.
3 Medical Officer, Regional Mental Hospital, Nagpur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gyanshankar Mishra, Assistant Professor, Department of Chest & TB, Government Medical College, Nagpur, Maharashtra– 440003, India. Email: gpmishra81@gmail.com
Cutaneous lesions are relatively uncommon manifestations of tuberculosis (TB). A 40-year-old female presented with skin lesion over the forehead since two months. She used to apply bindi over the same area since past 25 years. Based on skin biopsy and other ancillary investigations, she was diagnosed as a case of lupus vulgaris and initiated on anti TB medications following which, the lesion regressed. Thus, we herein report the first case of cutaneous tuberculosis (lupus vulgaris) associated with long term use of bindi.
Cosmetic tuberculosis, Cutaneous tuberculosis, Inoculation tuberculosis, Skin tuberculosis
Case Report
A 40-year-old female housewife presented with complaint of skin lesion over the forehead since two months. It was not associated with itching or local irritation. There was no other symptom. She did not have a history of any major illness in the past. She used to regularly stick bindi over the same area of the forehead since past 25 years on a daily basis. She did not give any history of use of other cosmetic (e.g. vermillion) over the same area during these years. Her systemic examination was unremarkable. There was no associated cervical lymphadenopathy. Local examination revealed an erythematous asymptomatic plaque with ill-defined margins of size approximately 2 × 2 cm on the central area of the forehead [Table/Fig-1]. Her blood/serum investigations were as follows: Hemoglobin – 13.7 g/dl, Total leukocyte count – 9000/mm3, Differential count - within normal limit, Platelet count – 3,16,000/mm3, liver function tests and kidney function tests were within normal limits. Mantoux test revealed 33 mm of induration and erythrocyte sedimentation rate (ESR) was 35 mm at the end of one hour. She was sero negative for human immunodeficiency virus (HIV). Skin biopsy from the lesion showed epidermis with irregular acanthosis and caseating granulomas in the dermis [Table/Fig 2]. Special stains (Fite Faraco (FF) staining and acid fast bacilli (AFB) staining) were negative. Histopathological features were thus suggestive of lupus vulgaris. Her induced sputum AFB smear was negative. Her chest radiograph was normal [Table/Fig-3]. Thus her clinico-pathological profile was compatible with a diagnosis of lupus vulgaris. Her treatment began with four drugs (Rifampicin, Ethambutol, Isoniazid and Pyrazinamide) for three months, followed by two drugs (Rifampicin, Isoniazid) for six months. At the end of the treatment the lesion had regressed considerably with significant clinical improvement [Table/Fig-4]. She was also advised to abstain from sticking bindi on the forehead henceforth.
Skin lesion at the start of treatment

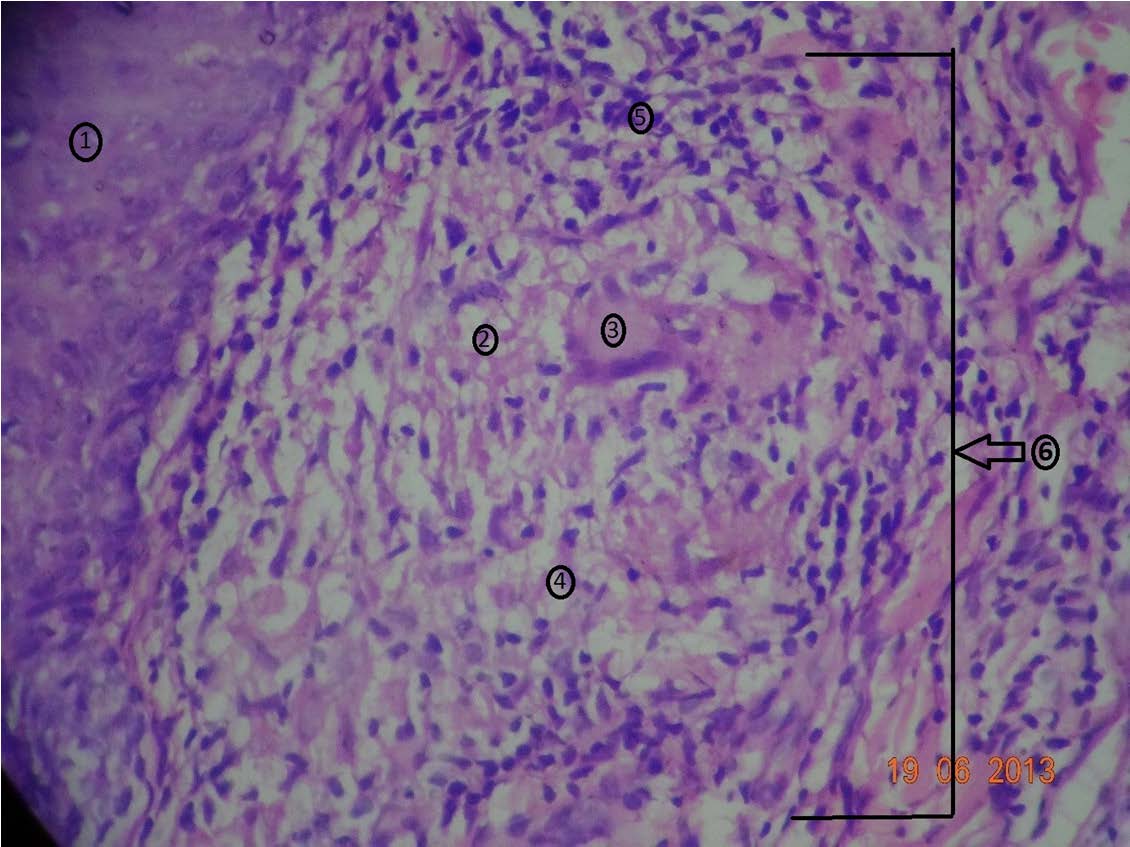
Skin biopsy showing features suggestive of lupus vulgaris.Serial sections showed epidermis with irregular acanthosis (1) with prominent adnexal structures. Dermis showed multiple granulomas (6); few with central caseation necrosis (2), surrounded by giant cells (3), epitheloid cells (4), histiocytes, lymphocytes (5)
Chest X-ray PA view of the patient
Regression of skin lesion following anti tubercular treatment

Discussion
The most common manifestation of tuberculosis is lung infection, while cutaneous tuberculosis is relatively uncommon and accounts for 1% of extra pulmonary tuberculosis. The skin may be infected via haematogenous spread, direct inoculation or auto-inoculation. Primary inoculation tuberculosis (PIT) is due to direct inoculation of Mycobacterium tuberculosis into the skin in a non-sensitised patient. This may result from minor abrasions, tattooing, ear piercing, minor surgical procedures or injections. PIT may occasionally evolve into lupus vulgaris (LV) or Tuberculosis verrucosa cutis (TVC) [1].
Lupus vulgaris (also known as tuberculosis lupus) is a chronic and progressive form of cutaneous TB that represents a reactivation of TB infection in people with moderate to high immunity against the bacillus. The classic plaque type of the disorder begins as a collection of discrete, red-brown papules that subsequently coalesce to form an indolent, asymptomatic plaque. The plaque gradually grows peripherally and develops central clearing and atrophy. Hypertrophic, ulcerative, and vegetative forms of lupus vulgaris may also occur. Lupus vulgaris is a paucibacillary form of cutaneous TB, and mycobacteria often cannot be detected histopathologically or by culture. Information that may be used to support the diagnosis includes consistent clinical and histopathological features and positive polymerase chain reaction (PCR) test results. Tuberculin skin testing is also often positive. Histopathological examination reveals tuberculoid granulomas with discrete central caseation in the upper dermis. The epidermis may be atrophic or acanthotic. If anti-TB therapy is not administered, lesions of lupus vulgaris persist. Over the course of years, the plaques may grow to enormous sizes. In addition, ulceration and destruction of underlying tissues may occur, causing severe disfigurement. Malignancies are known to occasionally develop in these lesions [2].
The points in favour of a diagnosis of lupus vulgaris in our patient were as follows: 1) Clinical history and physical appearance consistent with diagnosis (Classic plaque type lupus vulgaris), 2) Tuberculous granulomas seen on histology, 3) Positive Mantoux test and 4) Therapeutic response to anti-tuberculosis therapy.
Lupus vulgaris has been reported to occur as a result of exogenous inoculation like tattooing [3]. Also unusual presentations of lupus vulgaris over the face has been reported in the past [4]. Our patient used to wear bindi on the forehead for years. The development of lupus vulgaris over the same area points to possible etiology of exogenous inoculation of the infection due to long term bindi use. To the best of our knowledge this is the first case of lupus vulgaris associated with long term bindi use.
Cosmetics are defined as “articles intended to be rubbed, poured, sprayed on or sprinkled, introduced into or otherwise applied to the human body or any part thereof for cleansing, beautifying, promoting attractiveness or altering the appearance”. Particular cosmetics, such as kumkum, bindi, tilak, are applied in India and a few other countries among the Hindus. The bindi spot is traditionally worn only by married Hindu women, but it is now regarded as a fashion accessory and is worn by unmarried women and even by non-Hindus [5]. A bindi may be paste or a sticker and is worn only between the eyes (i.e. over the glabella). Self-adhesive bindis (sticker bindis) are disposable substitutes for older liquid bindis, and are popular because of their ease of application. The sticker bindis are made up of circular discs of polyvinylchloride (PVC) and the adhesive material contains para-tertiary butyl phenol (PTBP) the concentration of which may be as high as 80%. These agents have a melanocytotoxic effect. Other allergens present in the bindi include epoxy resins, Disperse Blue 124, Disperse Blue 106, nickel and thimerosal and gallate mix. The dermatological effects that have been linked with bindi use include contact leukoderma, allergic contact dermatitis and granuloma formation [6].Our patient used sticker bindi. Long term use of these bindis may be associated with local skin breach due to repeated and regular skin contact of adhesives on the “bindi”. Also unhygienic manufacturing processes may be associated with these bindis. These could be the possible causes of exogenous inoculation of the infection in the present case.
Conclusion
The present case implies the possible health concerns that may be associated with the widespread use of the extremely common decoration, the “Bindi”. Thus, there is a need for awareness in the population about the possible adverse cutaneous reactions to the cosmetics they use.
[1]. Ho S, Cutaneous tuberculosis: clinical features, diagnosis and managementHK Dermatol Venereol Bull 2003 11(2):130-38. [Google Scholar]
[2]. Evangeline B, Handog M, Maria Juliet E, Macarayo MD, Cutaneous manifestations of tuberculosis Massachusetts 2013 USAWolters Kluwer Health[updated Jul 16, 2013; cited 2014 24-10-2014]. Available from: http://www.uptodate.com/contents/cutaneous-manifestations-of-tuberculosis [Google Scholar]
[3]. Ghorpade A, Lupus vulgaris over a tattoo mark--inoculation tuberculosisJournal of the European Academy of Dermatology and Venereology: JEADV 2003 17(5):569-71. [Google Scholar]
[4]. Khandpur S, Reddy BS, Lupus vulgaris: unusual presentations over the faceJournal of the European Academy of Dermatology and Venereology: JEADV 2003 17(6):706-10. [Google Scholar]
[5]. Nath AK, Thappa DM, Clinical spectrum of dermatoses caused by cosmetics in south India: High prevalence of kumkum dermatitisIndian J Dermatol Venereol Leprol 2007 73:195-96. [Google Scholar]
[6]. Gupta D, Thappa DM, Dermatoses due to indian cultural practicesIndian J Dermatol 2015 60:3-12. [Google Scholar]