Lumbar Apophyseal Ring Fracture- A Case Report
Ravi Kumar T.V.1, Raghavendra Rao2, Daksh Gadi3, Amit Grover4
1Assistant Professor, Department of Orthopaedics, M S Ramaiah Medical College, Bangalore, India.
2Assistant Professor, Department of Orthopaedics, M S Ramaiah Medical College, Bangalore, India.
3Post Graduate Resident, Department of Orthopaedics, M S Ramaiah Medical College, Bangalore, India.
4Post Graduate Resident, Department of Orthopaedics, M S Ramaiah Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Daksh Gadi, Room No. 36, Neelgiri Hostel M S Ramaiah Medical College, Mathikere, Bangalore - 560054, India.
E-mail: Dr_daksh@yahoo.com
Posterior apophyseal ring fracture is a rare condition typically seen in adolescent age group because the ring apophysis and the adjacent vertebral body does not fuse completely and may separate at the cephalad or caudal edge. It usually simulates disc herniation in adolescents and children but disc lesion is very commonly associated with PRAF. The condition although is rare but a high index of suspicion should be there during evaluation of any adolescent patient with low back ache as it is often missed on conventional radiography. Multiple treatment options have been described in literature, both conservative and surgical. We hereby report a case of posterior apophyseal ring fracture with a calcified disc adherent to the dura for which decompression alone without discectomy was found to be an effective treatment.
Decompression, Discectomy, PRAF
Case Report
A 35-year-old male patient presented with low back pain of six months duration following a trivial fall. Pain was associated with numbness and pain in both lower extremities. Pain was initially insidious in onset and progressive in nature and walking distance was less than 500 meters. He was able to stand for not more than five minutes before the aggravation of pain. There was no history of constitutional symptoms and evening rise of temperature. On spine examination, there was no deformity but tenderness was present around L4-5 spinous process and paraspinal muscle spasm was significant. Range of motion in spine was decreased in flexion and extension and was painful. Pelvic and hip examination was normal. Neurological examination of lower limbs revealed bilateral SLR of 40*, EHL/EDL bilaterally 4/5 and FHL/FDL 3/5 with intact reflexes and sensation.
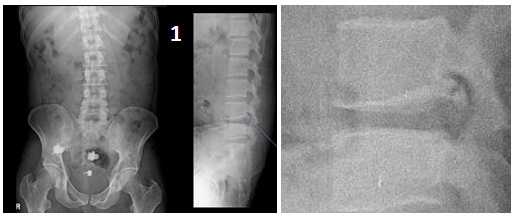
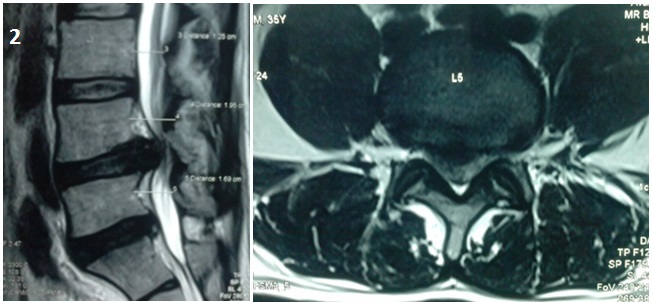
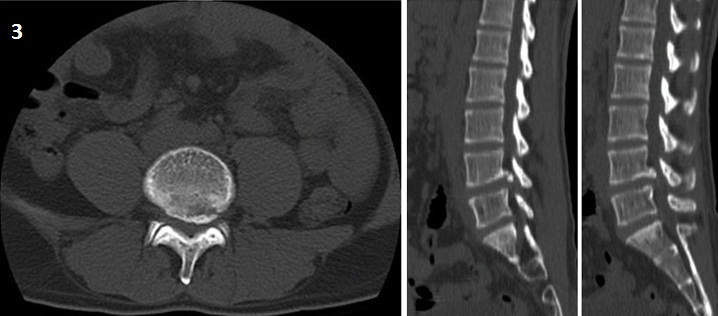
Blood investigations were normal and did not reveal any infective pathology. Plain radiographs [Table/Fig-1] were taken which showed avulsion of the posterior ring of inferior end plate of L4. MRI revealed a degeneration of L4-L5 and L5-S1 disc, with a central protrusion of the disc at L4-5 lateralising to the right side and a hyperintense area in the inferior end plate of L4 [Table/Fig-2]. To confirm the apophyseal ring fracture and size the fragment CT scan [Table/Fig-3] was done which confirmed the bony avulsion.
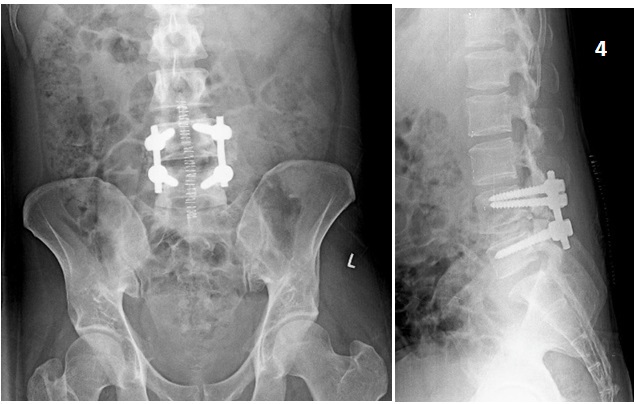
Patient was planned for decompressive surgery with stabilization of L4-5 level. After general anaesthesia, patient was positioned prone on Wilson Spinal Frame, opertive part was marked using fluroscopy. With standard midline incision and paraspinal muscle elevation and retraction at L4-5 level, decompression of stenosis was done with a L4 laminectomy, L4-L5 facetectomy and bilateral deroofing of L5 foramen. Intraoperatively, dura was found to be adherent to the apophyseal fragment anteriorly and was immobile. The disc and the fragment were left alone inview of adequate decompression. Since wide decompression and facectomy was needed with expected instability, posterolateral fusion was planned at L4-5 using pedicular instrumentation [Table/Fig-4]. Patient had a significant reduction in pain and improvement in deficits. Post operatively he was given regular wound care and physiotheraphy. He was discharged on post operative day five and sutures were removed on 12th post operative day and were on regular follow up. There was marked improvement of symptoms and nerological status at three months of follow up and patient is back to his agricultural profession.
Discussion
Posterior apophyseal ring fracture is a rare condition and is most commonly seen in age group of 10-50 y [1]. It is most commonly seen in the lumbar region [2]. Adolescent lumbar disc herniation [3,4] is an uncommon and is often associated with apophyseal ring fracture of the vertebral body. These fractures are often missed on plain film radiography [5]. Computed tomography [6] or magnetic resonance imaging (MRI) reveal the fragments much more readily [4,7]. Takata et al., have classified these fractures into three types on the basis of CT scan studies: Type I, a simple separation of the entire arcuate posterior margin of the vertebra; Type II, an avulsion fracture of the posterior rim of the vertebral body, including the overlying cartilage of the annulus fibrosus, resulting in a thicker and larger fragment; Type III, a more localized fracture involving a larger amount of the vertebral body such that the resulting fragment is larger than the vertebral rim [8]. There is an antecedent history of trauma in majority of the patients; however in few cases such history might be absent. The condition simulates an intervertebral disc prolapsed [9] so the decision making for the treatment is very important. Literature shows good results by multiple treatment options including conservative and surgical treatment [Table/Fig-5]. Surgical treatment options available include decompression alone, removal of fracture fragment, discectomy and fusion [1].
In this particular situation, the patient had chronic back pain since six months which had increased in severity leading to significant functional limitation. Type 2 fracture of posterior apophysis according to Takata K et al., classification was diagnosed and it was associated with central disc protrusion with significant neurodeficits. So, surgical intervention was planned. Xueyuan Wu et al., [1] showed that decompression depends upon type of PRAF, Fragment location, number of affected segments, surgeon’s skills. Removal of fracture fragment depends upon size of fragment, mobilisation of fragment, location and symptoms caused by it. Discectomy depends upon the degeneration of disc, age of patient and MRI findings.
In a study of 21 patients Ajay Krishnan et al., found that fracture fragment is less pliable than the disc material and require wider surgical exposure for excision of the fragment with disc. Partial laminectomy was inadequate and total laminectomy for satisfactory excision of disc and fragment is required [2].
In our case calcified disc with attachment of fragment to dura was noted intra-operatively. Decompression with laminectomy and facetectomy with posterior stabilisation was found to be an effective treatment, leading to a good functional outcome. Since the decreased pliability of the fragment [10] has been reported and also seen in this particular patient discectomy was not done and adequate decompression of the neural elements was found to be sufficient to achieve good functional outcome.
Radiograph, LS spine showing posterior apophyseal ring fracture of L4 inferior end plate
MR scan showing L4-L5 central disc protrusion
CT scan images showing the fracture fragment in sagittal and axial view
Post operative radiographs
Comparison of various treatment modalities as described in other studies
| Year | Author | Treatment |
|---|
| 2001 | CH YEN et al., | S1 roots decompression, L5 lamina fenestration, discectomy |
| 2000 | CH YEN et al., | physiotherapy |
| 2003 | CH YEN et al., | fenestration, discectomy,trimming of lower apophyseal ring of L2 |
| 1992 | Anthony C Tibbles et al., | electrotherapy and spinal manipulative therapy |
| 2014 | Our case | L4-L5 Facetectomy, decompression and posterior stabilisation |
Conclusion
Posterior apophyseal ring fracture with a calcified disc adherent to dura is a rare condition which requires not only meticulous decision making for the treatment but also a high index of suspicion for diagnosis by CT and MRI scans. Posterior instrumentation with decompression and discectomy may be an effective treatment option. In situations where the dura is adherent, decompression alone without discectomy can be an optimal mode of treatment. The need to stabilise the motion segment is guide, as usual, by the extent of instability caused by the wide decompression.
[1]. Wu Xueyuan, Ma Wei, Du Heng, Gurung Kiran, A review of current treatment of lumbar posterior ring apophysis fracture with lumbar disc herniationEur Spine J. 2013 22(3):475-88. [Google Scholar]
[2]. Krishnan Ajay, Patel Jyotish G, Patel Dinubhai A, Patel Pankaj R, Fracture of posterior margin of lumbar vertebral bodyIndian Journal of Orthopaedics 2005 39(1):33-38. [Google Scholar]
[3]. Peh Wilfred CG, Griffith James F, Yip Daniel KH, Leong John CY, Magnetic resonance imaging of lumbar vertebral apophyseal ring fracturesAustralasian Radiology 1998 42(1):34-37. [Google Scholar]
[4]. Tibbles Anthony C, Cote Pierre, Cassidy J David, Donat J, Adolescent apophyseal ring fracture simulating lumbar disc herniation: a case reportThe Journal of the CCA 1992 36(1):11-16. [Google Scholar]
[5]. D Resnick, Avulsion of the ring apophysis. In: Diagnosis of bone and joint disorders 2003 4th EditionPhiladelphiaWB Saunders:3007-3015. [Google Scholar]
[6]. Khoury Nabil J, Hourani Mukbil H, Arabi Mohammad MS, Abi-Fakher Faysal, Haddad Maurice C, Imaging of Back Pain in Children and AdolescentsCurr Probl Diagn Radiol 2006 :224-44. [Google Scholar]
[7]. Yen CH, Chan SK, Ho YF, Mak KH, Posterior lumbar apophyseal ring fractures in adolescents: a report of four casesJournal of Orthopaedic Surgery 2009 17(1):85-89. [Google Scholar]
[8]. K Takata, S Inoue, K Takahashi, Y Ohtsuka, Fracture of the posterior margin of a lumbar vertebral body.J Bone Joint Surg (Am) 1988 70:589-94. [Google Scholar]
[9]. AB Lippittm, Fracture of a vertebral body end plate and disc protrusion causing subarachnoid block in an adolescentClin Orthop 1976 16(1):112-15. [Google Scholar]
[10]. CH Chang, ZL Lee, WJ Chen, CF Tan, LH Chen, Clinical significance of ring apophysis fracture in adolescent lumbar disc herniationSpine (Phila Pa 1976) 2008 33(16):1750-54. [Google Scholar]