Imaging Diagnosis of Herlyn-Werner-Wunderlich Syndrome- An Extremely Rare Urogenital Anomaly
Shibani Mehra1, Komal Chamaria2, UC Garga3, Ankur Kataria4, Ashim Ahuja4
1Associate Professor, Department of Radiodiagnosis, Dr Ram Manohar Lohia Hospital & PGIMER, New Delhi, India.
2Senior Resident, Department of Radiodiagnosis, Dr Ram Manohar Lohia Hospital & PGIMER, New Delhi, India.
3Professor and Head of Department, Department of Radiodiagnosis, Dr Ram Manohar Lohia Hospital & PGIMER, New Delhi, India.
4Senior Resident, Department of Radiodiagnosis, Dr Ram Manohar Lohia Hospital & PGIMER, New Delhi, India.
5Senior Resident, Department of Radiodiagnosis, Dr Ram Manohar Lohia Hospital & PGIMER, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shibani Mehra, C1/36 Safdarjung Development Area, New Delhi-110016, India.
E-mail: Shibani.mehra@yahoo.in
Herlyn-Werner-Wunderlich (HWW) syndrome is a very rare congenital anomaly of the urogenital tract resulting from maldevelopment of both Mullerian and Wolffian ducts. It is characterized by the triad of uterus didelphys, obstructed hemivagina and ipsilateral renal agenesis. It generally presents at puberty shortly following menarche with the symptom of acute pelvic pain. Management of these cases is surgical and consists mainly of vaginoplasty with excision of the vaginal septum in order to release the obstruction and prevent the long term complication of recurrent pyocolpos and infertility. We report here a case of Herlyn-Werner-Wunderlich syndrome in a 13-year-old adolescent girl, emphasizing the role of imaging in the accurate and prompt diagnosis of this rare developmental urogenital anomaly. Only a few hundred such cases have been reported in literature till date.
Hematometra, MRI, Obstructed hemivagina, USG, Uterus Didelphys, Vaginal atresia, Vaginal septum
Case Report
A 13-year-old female with complaint of cyclical pain in the lower abdomen of three months duration, hindering her daily activities, was referred from the Department of Gynecology for ultrasound of abdomen. The patient denied any recent abdominal trauma, abnormal vaginal bleeding, nausea, vomiting or diarrhea. Patient had attained menarche just two months back. A bimanual abdominal examination revealed a cystic and tender left sided pelvic mass that was movable and mildly tender on palpation. The external genitalia were normal. The blood work was normal and the urine pregnancy test was negative.
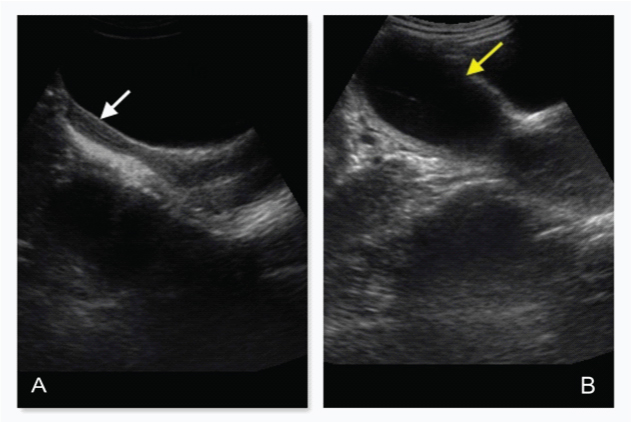
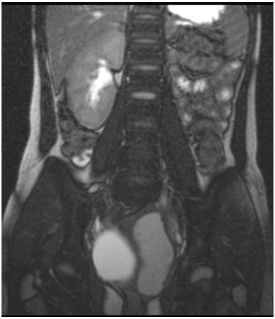
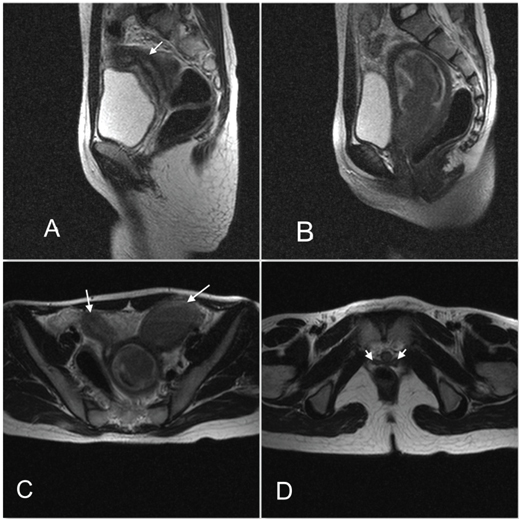
Ultrasound of abdomen showed absence of left kidney with two structures in the pelvis demonstrating the shape, contour and echo pattern of a uterus. The endometrial cavity of the left uterus was distended with fluid contents. The vagina was not clearly appreciated in continuity with this structure. The uterus on the right was of normal size and shape with the myometrium, endometrial cavity, cervix as well as vagina [Table/Fig-1A,B]. There was no evidence of communication between the two uteri. MRI abdomen was performed on 1.5T Siemens Symphony Scanner for better characterization of pelvic anatomy. On T2 weighted Trufi coronal image, absence of left kidney was confirmed [Table/Fig-2]. The endometrial cavity of the left uterus and upper part of left hemi vagina was distended with fluid which appeared hyper intense on T1WI and heterogeneous on T2W images and showed signal suppression on inversion recovery sequences suggestive of hemorrhagic contents, depicted in sagittal MR images [Table/Fig-3A,B]. The lower part of hemivagina was normally visualized between the rectum and lower urethra. The right endometrial cavity, cervix and hemivagina appeared normal. A simple cyst was present in the right ovary.
The T2 weighted axial images of the pelvis depicted two separate uteri each with a separate cervix and vagina with no communication between the two at any level [Table/Fig-3C,D]. The coronal, sagittal and axial MR images depicted a septum just below the hematometrocolpos in the mid left hemi vagina appearing as hypo intense band on both T1 and T2 weighted images and was the cause of ipsilateral genital tract obstruction [Table/Fig-4A,B]. A diagnosis of left renal agenesis with didelphys uterus and left hemivaginal septum causing obstruction and left hematometrocolpos was arrived at, based on the MR imaging. These findings were further confirmed on surgery with release of genital tract obstruction and drainage of hematometrocolpos after excision of the hemi vaginal septum through a perineal approach.
Discussion
Herlyn-Werner-Wunderlich (HWW) syndrome, also known as obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) is a rare form of uterovaginal duplication, with three characteristic anomalies namely, didelphys uterus, unilateral obstructed hemivagina and ipsilateral renal agenesis [1]. Müllerian duct anomalies have an incidence of 1-5% in the general population and 13-25% in women with recurrent pregnancy loss, with OHVIRA constituting 0.16-10% of these anomalies [2]. OHVIRA syndrome results from an embryologic aberration occurring during the 8th week of gestation that simultaneously involves the metanephric ducts as well as the Paramesonephric or Müllerian ducts. Failure of complete lateral fusion of the Paramesonephric ducts results in uterus didelphys and lack of development of the metanephric duct results in ipsilateral renal agenesis [3].
During embryogenesis, after 6 weeks, absence of Müllerian Inhibiting Factor in females promotes bidirectional growth of paired Müllerian (Paramesonephric) ducts. These paired ducts cross the Wolffian ducts (which act as inductors for promoting the former’s growth), migrate towards the midline and fuse to form the uterovaginal primordium, with simultaneous regression of the Wolffian ducts. By 9th embryological week, lateral fusion of the caudally and medially migrating paramesonephric ducts is complete with resorption of the intervening septum, forming a single uterovaginal canal which develops into the uterus and upper two third of vagina. The unfused cranial portions of the Müllerian ducts form the fallopian tubes. The lower third of vagina develops from the urogenital sinus. Vertical fusion takes place between the cranially moving sinovaginal bulb, which forms the vaginal plate and joins the canal [4].
In HWW syndrome embryonic arrest of the caudal portion of one of the Wolffian duct from an insult as early as 4th gestation week causes its maldevelopment, preventing the cross over and subsequent fusion of the Mullerian ducts [5]. The paramesonephric duct on the side lacking the Wolffian duct gets displaced laterally and cannot come in contact to fuse with the contra lateral duct in the midline. Instead each duct develops fully with a separate well formed cervix and hemivagina, resulting in duplication of uteri, (uterus didelphys) [6]. Complete nonunion between the paramesonephric ducts and the cranially migrating uterovaginal bulb results in a blind sac or vaginal atresia; while partial non fusion produces a remnant transverse vaginal septum which may be incomplete or complete with obstruction and hematometra or hematometrocolpos [7]. The location of the septum may be in the upper vagina in 46%, in mid vagina in 40% and in lower vagina in only 16% [5]. Since the ureteric bud develops from the Wolffian duct and ultimately induces the metanephric blastema to form the kidney, absence of Wolffian duct leads to omolateral renal agenesis. Renal anomalies are known to be associated in 35% of MDA in the form of agenesis, duplication, malrotation or ectopia [5].
HWW syndrome is usually discovered at puberty with symptoms of increasing pelvic pain, dysmenorrhea and a palpable mass due to the associated hematocolpos or hematometra resulting from the vaginal septum; though rarely a neonate may present with an abdomino-pelvic mass due to complete obstruction of the genital tract [2]. Retrograde menstruation may cause distension of the fallopian tubes and hematosalpinx and endometriosis, pelvic adhesions and increased risk of infertility too has been reported [6].
HWW syndrome is a combination of class I A (vaginal anomaly) and class III (uterine duplication anomaly) with associated renal agenesis as per The American Society for Reproductive Medicine (ASRM) classification of Mullerian duct anomalies [8]. According to this classification, based on the type of developmental aberrations there can be:-
a) Failure of development of one or both paramesonephric ducts and unicornuate uterus when unilateral; uterine agenesis / hypoplasia when bilateral (Class I and II anomalies).
b) Failure of lateral fusion of the two paramesonephric ducts resulting in bicornuate uterus when incomplete; and didelphys uterus when complete (Class III and IV anomalies).
c) Failure of resorption of the midline septum between the fused Paramesonephric ducts results in septate or arcuate uterus (Class V and VI anomalies)
d) Failure of vertical fusion of the ascending sinovaginal bulb with the fused paramesonephric ducts results in vaginal atresia or persistent vaginal septum.
MRI is the modality of choice for the diagnosis, characterization and presurgical evaluation in patients of OHVIRA, although sonography is the first modality in the work up due to its wide availability. Uterus didelphys is recognised on sonography when two completely separate uteri are seen in the pelvis with no communication between the two endometrial cavities. Two separate cervices and duplicated upper vaginas should be documented [9]. The major limitation of sonography is that hemivaginal septum may not be apparent .MRI is superior due to its multiplanar capability, inherent high soft tissue contrast and better characterization of pelvic anatomy.
MR imaging enables a diagnosis of uterus didelphys in OHVIRA by demonstrating two completely separate uteri, each with the normal zonal anatomy with presence of endometrial cavities and normal endometrial-myometrium ratio; and two separate cervices along with two hemivagina without communication between the hemi uteri and hemivagina [10]. The vagina appears as intermediate signal intensity structure between the urethra and rectum. The vaginal septum can be located by the level of obstruction. The unilateral hemivaginal septum in the upper part of vagina leads to hematometra and hematocolpos when in the lower third of vagina [10]. Hematometra is diagnosed as markedly distended endometrial cavity with characteristic high signal intensity on T1-weighted images of blood products. A very close differential diagnosis of this syndrome is bicornuate bicollis uterus with hemivaginal atresia wherein imaging demonstrates two widely divergent horns, communication between the two horns at some level, an intercornual distance of greater than 4.5 cm and presence of a deep fundal cleft greater than 1 cm [11].
Our patient is a classical case of uterus didelphys, transverse septum in the mid hemivagina and ipsilateral renal agenesis who presented soon after menarche with typical symptoms of cyclical lower abdomen pain, due to hematometrocolpos confirmed by MRI.
Ultrasound of pelvis showing two uterine cavities in the pelvis. Right sided uterus with its cervix and vagina (white arrow in A) is normal in size, shape and echo texture with normal endometrial cavity. Left sided uterine cavity (yellow arrow in B) is grossly distended and filled with fluid containing fine internal echoes within
T2W TRUFI coronal MR image is showing absence of left kidney
T2W sagittal MR images of the pelvis [A and B] show two uteri with two separate cervices each with its hemi vagina; there is no communication between the duplicated genital structures at any level. Left sided hematometrocolpos is demonstrated (arrow in image A) indicating presence of vaginal septum. The axial MR images [C and D] show two uteri (Arrow in image c) and two hemivagina with left hematometrocolpos(Arrow in image d) due to presence of a septum in the left hemivagina
T2W Coronal, Sagittal MR images of pelvis demonstrating the septum as a hypo intense band in the mid vagina (arrow) causing obstruction and hematometrocolpos

Conclusion
Ultrasound and MRI findings can collectively delineate uterine morphology, absence of the ipsilateral kidney, and the nature of the contents in the uterus and obstructed hemivagina. Knowledge of this rare syndrome of obstructed hemivagina in a duplicated genital system and ipsilateral renal agenesis will help the radiologist to arrive at an accurate and early diagnosis, critical in preventing chronic complications.
[1]. A Sarac, MK Demir, Herlyn-Werner-Wunderlich syndrome: a rare cause of infertilityEur Radiol 2009 19:1306-08. [Google Scholar]
[2]. D Cox, BH Ching, Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolposJRCR 2012 6(3):9-15. [Google Scholar]
[3]. C Behr Spencer, L Courtier Jesse, A Qayyum, Imaging of Mullerian Duct AnomaliesRadiographics 2012 32(6):E233-50. [Google Scholar]
[4]. P Acien, Embryological observations on the female genital tractHuman Reprod. 1992 7(4):437-45. [Google Scholar]
[5]. E Somigliana, P Vercillini, Asymmetric lateral distribution of obstructed hemivagina and renal agenesis in women with uterus didelphys: instant case series and a systematic literature reviewFert Sterility 2007 87(4):719-24. [Google Scholar]
[6]. II L Adair, M Georgiades, R Osborne, T Ng, Uterus didelphys with distal vaginal agenesis and unilateral renal agenesis: common presentation of an unusual variationJ Radiol Case Rep 2011 5(1):1-8. [Google Scholar]
[7]. JM Goldberg, S Falcone, Müllerian anomalies: reproduction, diagnosis and treatment. In:Gidwani G, Falcone T, eds. Congenital malformations of the female genital tract :diagnosis and management. 1999 Cleveland OhioLippincott Williams & Wilkins:249 [Google Scholar]
[8]. The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions Fertil Steril 1988 49(6):944-5510. [Google Scholar]
[9]. SN Salim, MR imaging diagnosis of uterovaginal anomalies. Current state of the artRadiographics 2003 23(5):e13 [Google Scholar]
[10]. C Reinhold, H Hrisak, R Forstner, Primary amennorrhoea: evaluation with MR imagingRadiology 1997 203(2):383-90. [Google Scholar]
[11]. R Del Vescovo, S Battisti, VD Paola, CL Piccolo, RL Cazzato, I Sansoni, Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosisBMC Medical Imaging 2012 12:4 [Google Scholar]