Hemangiomatous Ameloblastoma- A Case Report of a Very Rare Variant of Ameloblastoma
Maruthi Devi Kasangari1, Kiran Gundamaraju2, Mandapati Jyothsna3, Andy Venkata Subash4, Kumbakonam Aravind5
1 Reader, Department of Oral & Maxillofacial Pathology, Malla Reddy Dental College for Women, Hyderabad, Telangana, India.
2 Assistant Professor, Department of Oral & Maxillofacial Pathology, Government Dental College and Hospital, Hyderabad, Telangana, India.
3 Associate Professor, Department of Oral & Maxillofacial Pathology, Government Dental College and Hospital, Hyderabad, Telangana, India.
4 Reader, Department of Oral & Maxillofacial Pathology, Lenora Dental College, Rajamundry, Andhra Pradesh, India.
5 Senior Lecturer, Department of Oral Medicine & Radiology, Malla Reddy Dental College for Women, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. G Kiran, Assistant Professor, Department of Oral & Maxillofacial Pathology, Government Dental College & Hospital, Afzalgunj, Hyderabad-500012, Andhra Pradesh, India. E-mail : Kiran.dentist@gmail.com
Ameloblastoma is a true benign odontogenic neoplasm with many classical histological variants, common being follicular and plexiform types. Hemangiomatous amelobalstoma is a very rare variant that shows unique histopathologic characteristics varying from conventional ameloblastoma. We present a rare variant of ameloblastoma in a 35-year-old female patient with a swelling over left mandibular region, showing mixed radiolucent-opacity, which on enucleation histopathologically revealed ameloblastomatous areas with extensive vascular component.
Collision tumour, Follicular ameloblastoma, Haemangioma, Odontogenic tumour, Plexiform ameloblastoma
Case Report
A 35-year-old female patient presented with a chief complaint of painless swelling on the left side of the face since eight months to the Department of Oral Medicine and Radiology, Malla Reddy Dental College for Women, Hyderabad. Telangana, India. Her history revealed that the swelling gradually grew to the present size. Her medical, dental, habitual and family history was not significant. On extra oral examination, inspection showed a swelling measuring approximately 4x3 cm in size, oval in shape, having well defined margins. The colour of the lesion was similar to the normal adjacent skin. The swelling extended superiorly to the line extending from the tragus of the ear to the corner of the mouth. Inferiorly to lower border of the mandible, posteriorly up to the ramus of the mandible and anteriorly up to the corner of the mouth [Table/Fig-1]. No visible pus discharge was seen. On palpation, the inspectory findings were confirmed and the lesion was bony hard with central region showing variable consistency of hard and soft areas. The lesion was non tender. On intra oral examination, firm, smooth, non-fluctuant swelling was seen extending from 31 to the anterior border of the ramus. The mandibular left first molar and second premolar have been extracted 11 months back. First premolar was carious.
Extra oral view showing swelling

Panaromic radiograph revealed an well defined mixed radioopaque-lucent multilocular lesion extending from lower left central incisor to the ascending border of ramus [Table/Fig-2]. Impacted second molar was seen at the inferior border of the mandible. Few septae were arranged in tennis raquet appearance. Root resorption was noticed in relation to 34. Over retained 85 was also seen. Radiological differential diagnosis of central hemangioma, ameloblastoma, odontogenic myxoma was considered.
OPG showing mixed radiolucent-opacification

A provisional diagnosis of ameloblastoma and clinical differential diagnosis of dentigerous cyst and odontogenic keratocyst was made. After obtaining patient's consent, enucleation was done and multiple bits of the soft tissue specimen of approximately 4cm X 2cm X 1cm were sent to the Department of Oral Pathology.
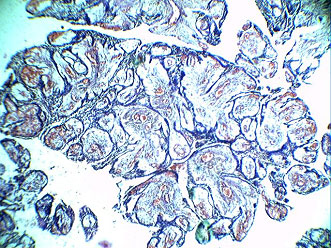
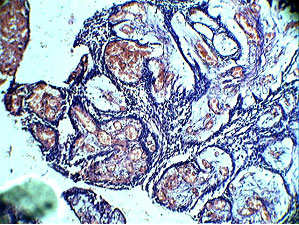
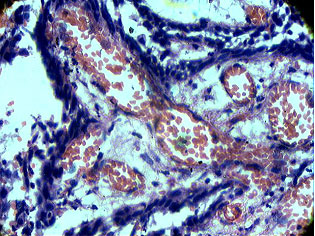
On microscopic examination, the tissue section revealed plexiform ameloblastoma with a prominent vascular component. It showed anastomosing cords and sheets of odontogenic epithelium in a loosely arranged vascular connective tissue stroma. The epithelium was surrounded by cubodial ameloblast like cells with central stellate reticulum like cells. The vascular component consisted of blood filled spaces of varying sizes lined by endothelial cells. At focal areas vascular spaces were large and compressing the odontogenic strands [Table/Fig-3,4,5]. A diagnosis of Hemangiomatous Amelobal- stoma was made.
Photomicrograph (5x) showing odontogenic cords and islands with loose vascular tissue
Photomicrograph (10x) showing ameloblastomatous areas with vascular areas
Photomicrograph (40x) showing extensive vascular area
Partial hemimandibulectomy was planned followed by immediate reconstruction with a nonvascularised illiac graft. But the patient was not cooperative and reluctant for surgical treatment and hence the procedure could not be carried out. The patient was recalled for follow up visits but did not return to the department.
Discussion
Ameloblastoma is one of the most common odontogenic tumours with approximately making 11% of them. It is categorized based on clinico-radiological features into three types: solid or multicystic, unicystic, and peripheral [1,2]. Odontogenesis is a complex process and any deviation from normal process results in odontogenic cysts and tumours. In ameloblastoma there is faulty differentiation of enamel organ to point of actual enamel formation [2,3].
Various histological variants of ameloblastoma have been described in the literature like follicular (most common), plexiform, acanthomatous, granular (most aggressive), basal cell and desmoblastic [4]. Ameloblastoma has many histological variants with follicular ameloblastoma the most common one. Reports of variants like clear cell, papilleferous, keratoameloblastoma and a very rare pattern hemangiomatous ameloblastoma have also been described in the literature. Studies have shown that all the mentioned histological variants do not differ significantly in either biological behaviour of the tumour or its prognosis after treatment. Desmoblastic and hemangiomatous amelobalstoma are exceptions with the former thought to be less aggressive and the later due to its extreme vascular component carry surgical complications. However, in Many cases have been reported with mixture of these patterns [4–6].
Hemangiomatous amelobalstoma is a very rare variant of ameloblastoma. Hemangiomatous amelobalstoma term refers to any ameloblastoma which has in its stroma many spaces filled with blood or large endothelial-lined capillaries. First case of Hemangiomatous Amelobalstoma (vascular ameloblastoma) was described by Kuhn (1932) as a combination of hemangioma and adamantinoma. Aisenberg (1950) later reported a similar lesion as admantinohemangioma. It is supposed that in Hemangiomatous Amelobalstoma the stromal component is mostly replaced by vascular component [7].
Earlier hemangiomatous amelobalstoma was documented as ameloblastic hemangiomas, adamantino hemangiomas and hemangio ameloblastomas [5,6]. Literature search to the best of our knowledge has revealed less than 15 cases of hemangiomatous amelobalstoma, suggesting its rarity [Table/Fig-6] [1,6–12].
Comparison of various cases of Hemangiomatous Amelobalstoma
| Author | Age | Sex | Site | Treatment done | Healing and prognosis |
|---|
| Aisenberg MS [6] | 48 | female | Right posterior mandible | Enucleation | uneventful |
| Lucas RB [9] | 43 | female | Right mandible | Resection of affected portion | Uneventful and no complaint after follow up |
| van Rensburg LJ [10] | 26 | female | Left mandible, 3rd molar region | Partial hemimandibulectomy Planned but patient refused | No follow up could be done |
| Ide F [2] | 56 | male | Anterior maxilla | Enucleation and curettage | Good healing after 6 months follow-up |
| Tamgadge AP [1] | 31 | male | Left mandible premolar molar area | Enucleation and curettage | Good healing after 4 months follow-up |
| Sharma VK [11] | 15 | male | Maxillary right molar area | Enucleated | Followed for 6 months |
| Harshvardhan SJ [12] | 42 | male | Right posterior mandible | Hemimandibulectomy | Uneventful and no complaint after followup for 2 years |
| Sarode GS [13] | 18 | male | Right posterior mandible | curettage | Patient lost to follow-up |
| Rajmohan M [14] | 20 | male | Right posterior mandible | Hemimandibulectomy | Patient lost to follow-up |
| Our Case | 35 | Female | Left posterior mandible | Enucleation | Lost to follow up |
As very few cases of hemangiomatous amelobalstoma are reported, the origin of its vascular component is still debatable and not clearly understood. Few authors consider the vascularity as hamartomatous growth, few others as part of neoplastic process and others consider it as a separate neoplasm. Whereas Smith did not considered hemangiomatous amelobalstoma as a separate variant of ameloblastoma as according to him the extensive vascularity might be owed to other causes [8].
To summarize the various theories proposed to explain the pathogenesis of the vascular component of hemangiomatous amelobalstoma are [6–11,13]
Angiogenesis during tumour development.
Represents a separate neoplasm,
Hamartomatous malformation,
Traumatic incident,
Secondary change,
HA representing a collision tumour.
Sometimes during odontogenesis, anomalous induction of blood vessels may occur and result in their abnormal proliferation. Such proliferated vessels possibly will turn into a component of tumour [11].
Trauma during procedures like extraction of teeth might induce the epithelial cell rests in the periodontal ligament to proliferate and result in tumour process. Usually after any injury the injured tissues undergo repair to retain their original condition. Any disturbance in repair process of damaged tissues involves excessive granulation tissue formation, which consists of proliferating endothelial cells and new capillaries [13]. The presence of extensive vascular component in our case might be due to stimulation and proliferation of blood vessels due to trauma created during extraction of teeth and subsequent repair phenomenon.
Lesions such as hemangiomas, telangiectatic osteosarcoma, angiomatoid malignant fibrous histiocytoma should be included in differential diagnosis. In telangiectatic osteosarcoma, there are large spaces filled with blood and huge areas of necrosis. Whereas, angiomatoid malignant fibrous histiocytoma contain characteristics of a fibrohistiocytic tumour and a vascular tumour [7]. Surgical complications due to extensive vascularity in such vascular lesions should always be kept in mind during treatment planning.
Pathogenesis, clinical features, treatment modality and prognosis of hemangiomatous amelobalstoma until now is not completely understood as only very few cases have been reported. Few authors considered Hemangiomatous Amelobalstoma as a collision type of tumour, in which two separate tumours develop in the same area and collide, and their components blend together [13]. Lucas, viewed that vascular component in hemangiomatous amelobalstoma is purely a secondary change. According to him cystic degeneration occurs in stroma in plexiform ameloblastoma, and during the cysts formation some blood vessels instead of diminishing may persist and dilate resulting in vascular component as seen in hemangiomatous amelobalstoma [12,15].
Conclusion
Hemangiomatous Amelobalstoma and other such lesions with extensive vascular component may lead to fatality even following minor procedures. Our case clearly demonstrates the distinctive histologic pattern and should be kept in differential diagnosis of vascular lesions. More number of such cases has to be studied thoroughly to exactly know the origin, nature and behaviour of Hemangiomatous Amelobalstoma.
[1]. Tamgadge AP, Sirur DG, Bhalerao SS, Pariera T, Tamgadge SA, Hemangiomatous Ameloblastoma: A case report of a rare variant of ameloblastomaInt J Contemp Dent 2010 2:16-19. [Google Scholar]
[2]. Ide F, Horie N, Shimoyama T, Sakashita H, So-called hybrid odontogenic tumours: Do they really existsOral Med Patol 2001 6:13-21. [Google Scholar]
[3]. Shafer WG, Hine MK, Levy BM, Cysts and tumours of odontogenic originShafer’s Textbook of Oral Pathology 2005 5th edNew DelhiElsevier:395-98. [Google Scholar]
[4]. Krammer IR, Pindborg JJ, Shear M, Histological typing of odontogenic Tumours 1992 BerlinSpringer-Verlag:11-14. [Google Scholar]
[5]. Neville BW, Damn DD, Allen CM, Bouquot JE, Oral and maxillofacial Pathology 2002 2nd EdPhiladelphiaWB Saunders Co:611-16. [Google Scholar]
[6]. Aisenberg MS, AdamantinohemangiomaOral Surg Oral Med Oral Pathol 1950 3:798-801. [Google Scholar]
[7]. Oliver RT, McKenna WF, Shafer WY, Hemangioameloblastoma; report of a caseJ Oral Surg Anesth Hosp Dent Serv 1961 19:245-48. [Google Scholar]
[8]. Smith JF, The controversial AmeloblastomaOral Surg Oral Med Oral Pathol 1968 26:45-75. [Google Scholar]
[9]. Lucas RB, A vascular ameloblastomaOral Surg Oral Med Oral Pathol 1957 10(8):863-68. [Google Scholar]
[10]. Van Rensburg LJ, Thompson IO, Kruger HE, Norval EJ, Hemangiomatous ameloblastoma: Clinical, radiologic, and pathologic featuresOral Surg Oral Med Oral Pathol Oral Radiol Endod 2001 91:374-80. [Google Scholar]
[11]. Sharma VK, Verma SK, Goyal L, Chaudhary PK, Hemangiomatous ameloblastoma in maxilla: A report of a very rare caseDent Res J 2012 9:345-49. [Google Scholar]
[12]. Harshvardhan SJ, Kumar Mohan KP, Kumar MS, Waghrey S, A mixed neoplasm of intraosseous hemangioma with an ameloblastoma: A case of collision tumour or a rare variantClinics and practice 2012 2(1):e5 [Google Scholar]
[13]. Sarode GS, Sarode SC, Vaidya K, Intraluminal plexiform hemangioameloblastomatous proliferation in unicystic ameloblastoma: An unusual case reportIndian J Dent Res 2013 24:390-92. [Google Scholar]
[14]. Rajmohan M, Hemangiomatous ameloblastoma: A Rare VariantJ Orofac Res 2014 4(1):63-66. [Google Scholar]
[15]. Villa VG, Hemangioma of the cavernous type associated with ameloblastoma (ameloblastic hemangioma)J Oral Surg Anesth Hosp Dent Serv 1960 18:429-31. [Google Scholar]