The main modality of treatment for locally advanced head and neck cancers is surgery; however radiation therapy with the intent to preserve organ function is used as alternative method to surgery combined with chemotherapy. If radiation therapy is used, the doses are in ranges of 66 Gy to 70 Gy which will provide good control in T1 and T2 lesions of around 90% [1,2]. T3 and T4 lesions have poor local control of around 30% to 40% only. Escalation of the doses has improved the local control with higher incidence of toxicity. Though, there have been attempts with various fractionation modalities to increase the biologically effective dose, the optimal fractionation schedule is still not known. Among various altered fractionation schedules, only hyper-fractionation has proven increased local control in head and neck cancers [3]. MARCH collaborative meta-analysis had shown improved survival benefit with hyper-fractionated schedule over single daily fractionation in head and neck cancers. Altered fractionation schedules delivered with conventional radiation therapy techniques have reported increased acute toxicity [4]. The acute effects like mucositis during the radiation therapy is the major cause of treatment prolongation and can lead to inferior tumour control and this remains the major drawback in universal acceptance of these schedules. Integration of this altered fractionation with newer modalities of treatment like 3-dimensional radiation therapy (3D-CRT) and intensity modulated radiation therapy (IMRT) may help to increase the tumour dose and at the same time reduces dose to normal healthy tissues.
This paper reviews the early results of combining hyper-fractionation with IMRT in three patients.The combination of hyperfractionated radiotherapy delivered with Inverse planned intensity modulated radiotherapy technique has not been widely reported. In this pilot study, three patients were treated with such a regimen and the technical feasibility and toxicity of such an approach has been discussed.
Materials and Methods
A. Inclusion Criteria and Patients Characteristics
Patients with newly diagnosed, biopsy proven, locally advanced head and neck cancers of oropharynx, hypopharynx and larynx were eligible for this study. Other inclusion criteria for the study were Eastern Cooperative Oncology Group (ECOG) performance score of 2 or less, age less than 70 y, T3, T4 and N0 or N+ and M0 or stage III and stage IV A and IV B, previously untreated patients, hemoglobin greater 8 gm% and no contraindications for radiation therapy. Prior to inclusion in to the protocol, a written informed consent was obtained from all patients and treatment was carried out according to the protocol from December 2010 to May 2012. Three patients who underwent the HF IMRT protocol were recruited based on the above criteria [Table/Fig-1]. The study was approved by the institutional review board and ethics committee and complied to ethical standards of the relevant national guidelines on human experimentation given by the Indian Council of Medical Research (ICMR) and with the Helsinki Declaration of 1975, as revised in 2008.
| Patient # | Age | Sex | Type/Stage | Histopathology |
|---|
| 1 | 32 | M | Oropharynx (base of tongue) Stage III | Moderately differentiated squamous cell carcinoma |
| 2 | 67 | M | Oropharynx (base of tongue) Stage III | Moderately differentiated squamous cell carcinoma |
| 3 | 68 | M | Supraglottis stage III (left arytenoid and aryepiglottic fold) | Moderately differentiated squamous cell carcinoma |
B. Treatment and Evaluation
The patients were immobilized in supine position using 5- point thermoplastic ray cast mask. The reference points were marked using wall mounted orthogonal lasers. These patients underwent CT simulation with spiral CT scan in the treatment position. 80 ml ionic contrast was given and 3 mm thick images were obtained in Digital Imaging and Communications in Medicine (DICOM) format. The following volumes were delineated: a) GTV or HRV (Gross tumour volume or High risk volume) includes the gross palpable, visible or demonstrable extent of the tumour and the invaded nodes. It is delineated based on CT scan volume along with clinical and scopy data, b) CTV 1 or IRV (Clinical target volume 1 or intermediate risk volume) which is delineated by giving 1 cm margin around GTV in all dimensions and the entire anatomical region of the tumour and involved nodal regions, c) CTV 2 (Low risk volume) includes non involved nodal stations in the neck with greater than 10% expected incidence of subclinical metastases. PTV (Planning target volume) is obtained by expansion of CTV by 5 mm in all directions but was restricted to within the limits of body. Definitions of GTV, CTV and PTV were according to the ICRU report 62. [Table/Fig-2] shows the representation of target volumes and OARs and doses prescribed.
Target volumes and doses prescribed
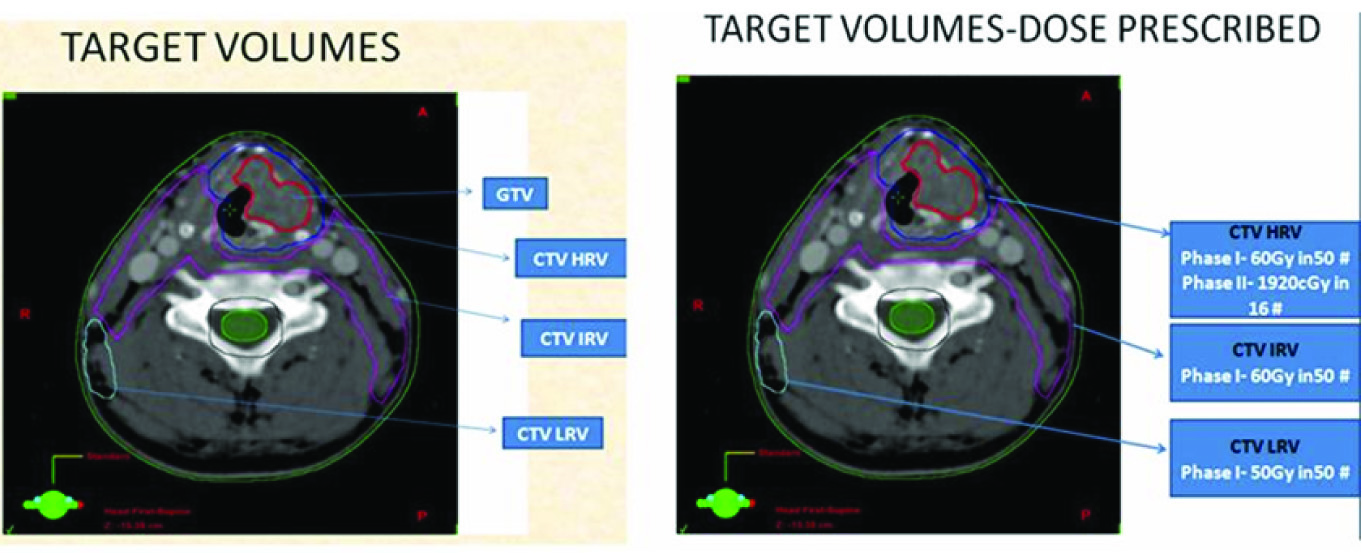
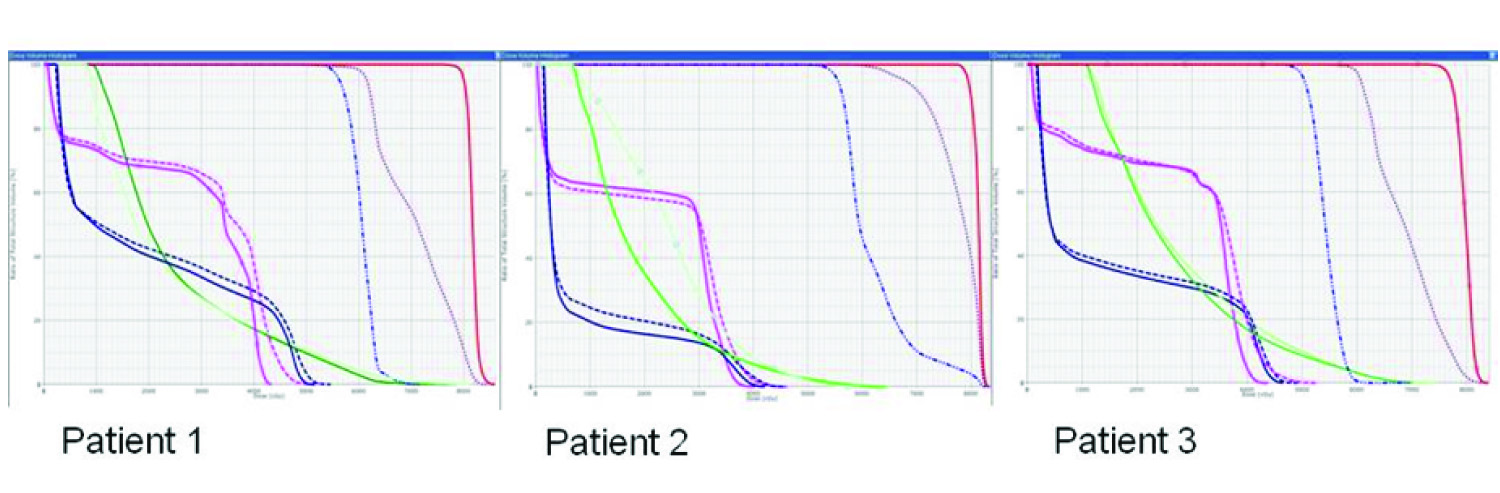
These patients were treated with hyper-fractionation schedule utilizing intensity modulated radiation therapy (HF-IMRT). The dose constraints for organs at risk were given according to the Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) criteria [1,2]. The dose of the target volumes and the organs at risk were calculated according the plan sum obtained from the Phase I and Phase II plans. The dose prescription was given to the International Commission on Radiation Units and Measurements (ICRU) reference point isocentre. [Table/Fig-2] shows the target volume and doses prescribed. These patients were planned on ECLIPSE planning system (version 9) with inverse planning technique. Seven equally spaced beams with 6-MV photons and dynamic multi-leaf collimators were used during planning and treatment. Plan evaluation was done and D98, D2, D95, D90, V100, D2cc and mean doses were calculated for the target volumes from DVH curves and by analyzing the dose distribution. Similarly, V30 and Mean dose were calculated for ipsilateral and contralateral parotid glands, D max and mean doses were calculated for planning risk volume (PRV) spine and PRV brain stem. Mean dose to the larynx was calculated for the patients except for one patient who had supraglottic malignancy. The plan sum DVH curves of the three patients are shown in [Table/Fig-3].
Shows the plan sum DVH curves of the three patients
Dosimetric measurements were done and treatment was started after making sure the variation between calculated and measured doses were between +/-7 percent. These patients were treated in Linear accelerator with 6 MV photon beam. Weekly kV on-board imaging was done and offline corrections made if necessary.
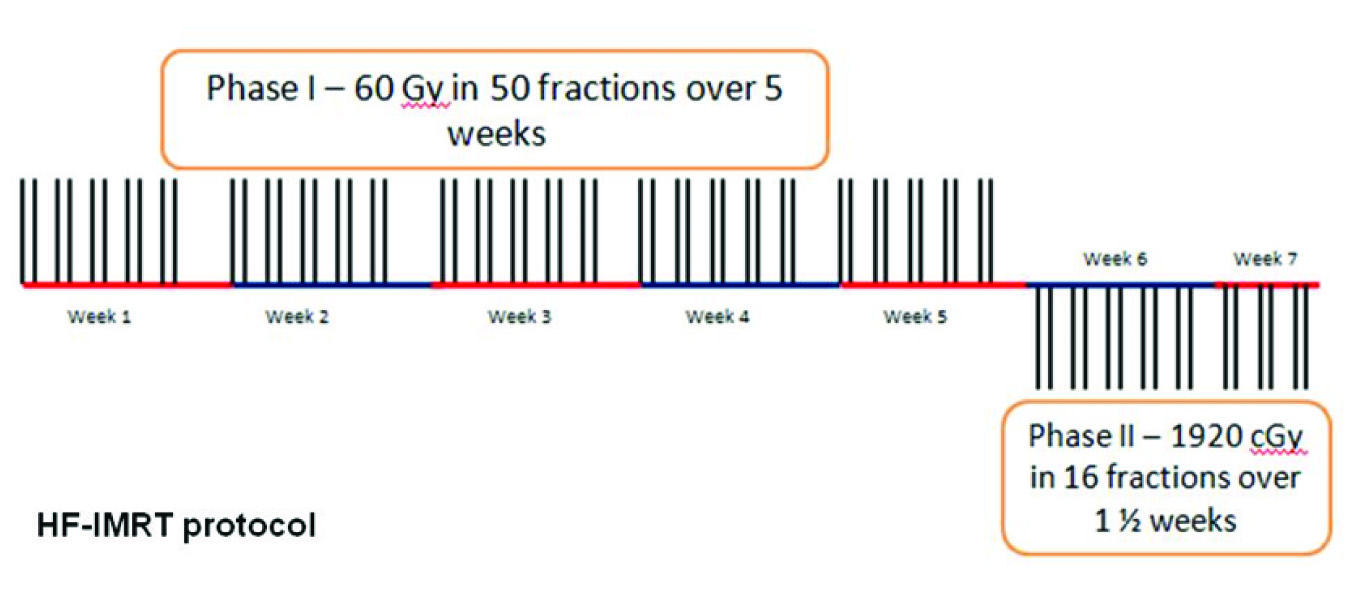
Hyper-fractionated radiotherapy was administered five days per week in twice daily fractions of 1.2 Gy separated by minimum of 6 to 8 hours. No concurrent chemotherapy was administered during radiation therapy. [Table/Fig-4] shows the fractionation and dose schedule in this study.
Shows the fractionation and dose schedule in this study
Weekly monitoring was performed for all patients for acute effects of radiation, which were assessed according to Common Terminology Criteria for Adverse Events (CTCAE) v 3.0. The quality of life was assessed using the EORTC QLQ-H&N35 and EORTC QLQ-C30 (version 3). These patients were expected to complete the radiation therapy including the breaks within 60 days.
Results
For the three patients the plans were evaluated using the dose volume histograms. The D98, D2, D95, D90, mean dose and D2cc were separately calculated for GTV, CTV 1 and CTV 2. For GTV, D98 was between 96.1% and 100.2% (absolute dose range – 7619 cGy to 7939 cGy). The dose received by 95% of volume (D95) was in the range of 97.2% to 100.9% (absolute dose range – 7705 cGy to 7999 cGy). Mean doses were 8119, 7961 and 8165 for each patient respectively. D2cc was within 105% range (102% to 105%, absolute dose range – 8132 cGy to 8352 cGy).
For CTV 1, dose received by 95% volume (D95) was absolute Dose range – 6067 cGy to 6780 cGy. D98 was 5975 cGy to 6402 cGy. For CTV 2 volume, dose received by 95% volume (D95) was absolute Dose range – 5038 cGy to 5629 cGy. D98 was absolute dose ranges – 4936 cGy to 5508 cGy. The mean dose for parotid glands was maintained within 26 Gy. 50% of parotid glands of all patients had received less than 3000 cGy, which were in accordance to QUANTEC guidelines. D1cc of PRV (Planning Risk Volume) spine was less than 5000 cGy for all patients (dose range: 2850 to 4625 cGy ). The maximum dose for spinal cord was (Dmax) was 4625 cGy (dose range: 2850 cGy to 4625 cGy). The maximum D1cc of PRV brain stem was 5118 cGy (dose range: 4199 cGy to 5118 cGy). The maximum dose for PRV brain stem was 5469.1 cGy (dose range: 4597.6 to 5469.1 cGy).
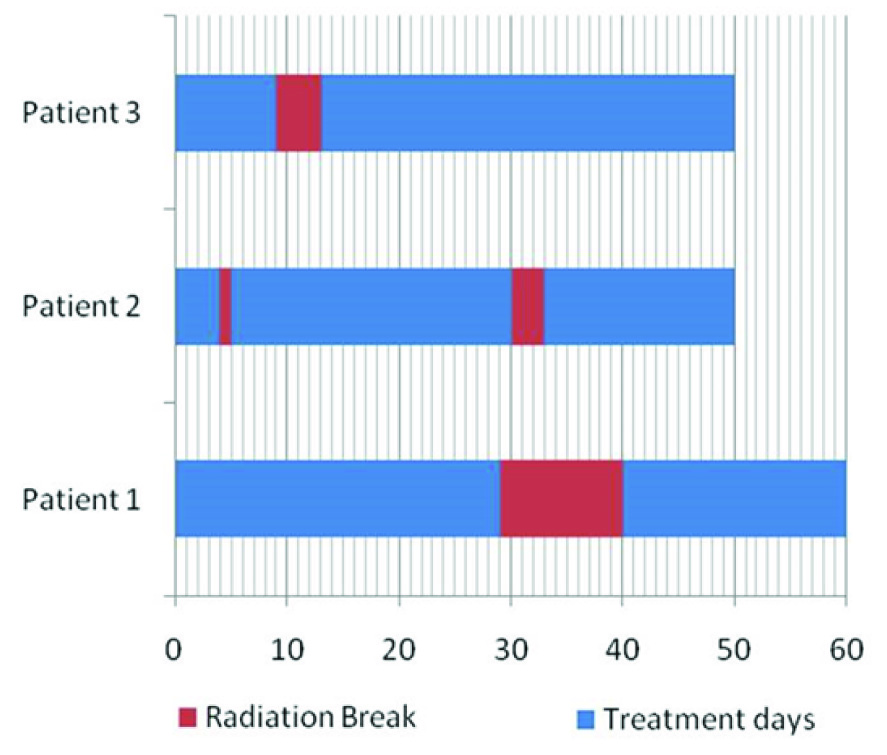
All patients completed treatment within 60 days (Range 50 – 60 d). The maximum treatment break due to radiation toxicity was 11 days and two other patients had four days and two days respectively. [Table/Fig-5] shows the treatment duration and radiation breaks of each of the patient. One patient had early break in radiation due to a non-treatment related fall. The patient with maximum duration break had grade III mucositis during the fourth and fifth week of radiation.
Shows the treatment duration and radiation breaks of each of the patient
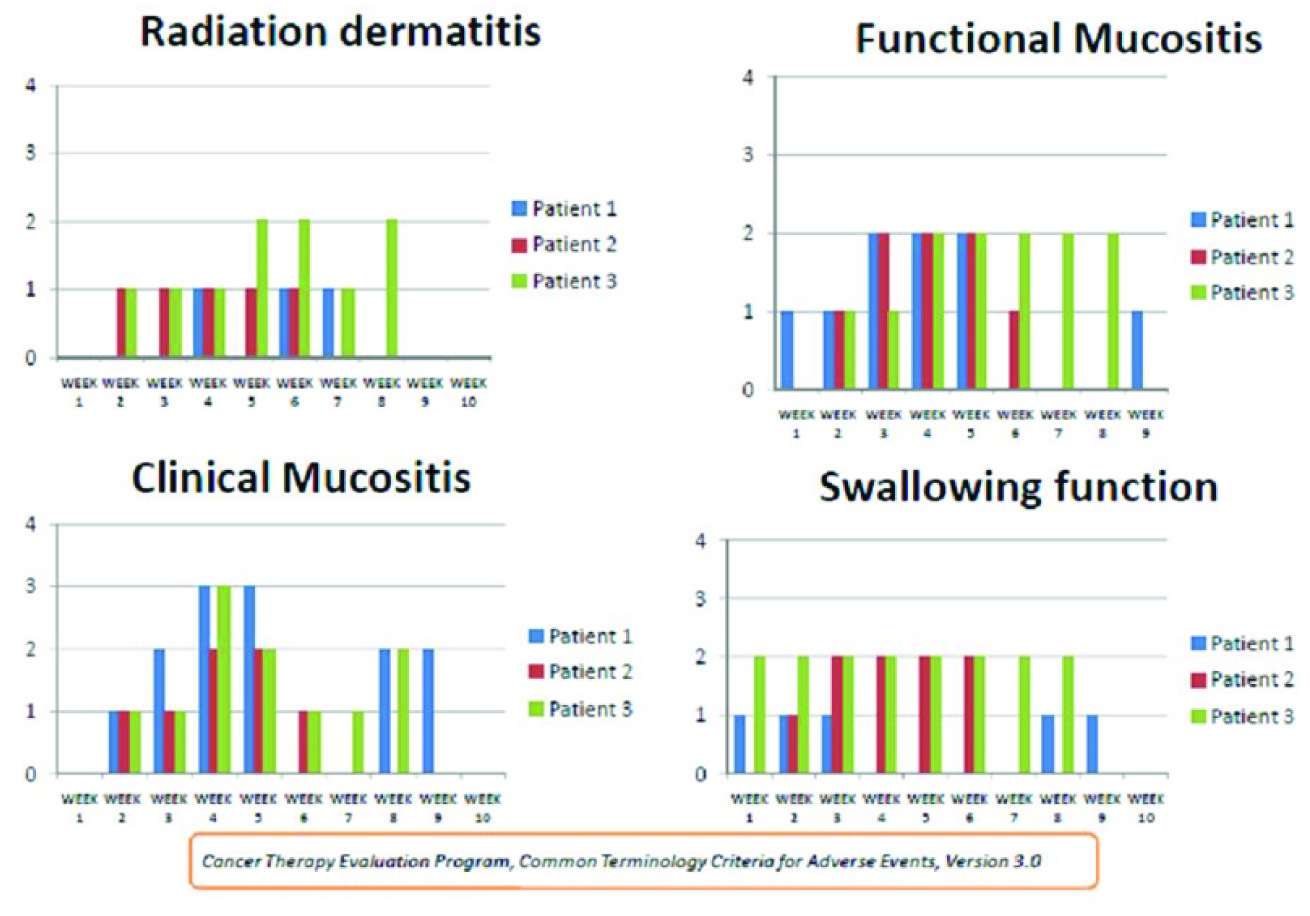
The acute toxicities of each of these patients during the treatment are represented graphically in [Table/Fig-6]. Radiation dermatitis, clinical mucositis, functional mucositis and swallowing function were assessed every week. These toxicities were assessed according to CTCAE v3.0. The maximum grade of radiation dermatitis, functional mucositis and swallowing function was grade II. The maximum clinical mucositis noted as grade 3 in two patients in week four of treatment. One patient with grade III clinical mucositis had grade II functional mucositis and swallowing function. The EORTC quality of life assessment score for all patients showed worsening of pain and decreased social activity during the fourth and fifth week of treatment. However, none of these patients required feeding procedures during the entire treatment. During the first follow up visit, the quality of life scores had reached the baseline for two patients who were on regular follow up. One patient had a follow-up period of three years and other had follow up period of two years and both were disease free during their last follow up visit. One patient had not reported for follow up after completion of radiotherapy.
The acute toxicities of each patient during the treatment
The average time taken for each fraction of hyper-fractionated IMRT was found to be seven minutes. In comparison average time taken by the patient with IMRT in conventional fractionation was also seven minutes per fraction. The beam on time was same for the full treatment time in patients treated with simultaneous integrated boost with conventional fractionation and also for per fraction of HF-IMRT. The total machine time was doubled in HF-IMRT.
Discussion
The preferred treatment of choice for locally advanced head and neck cancer is chemo-irradiation [4]. In the earlier decades various radiotherapy regimens with different fractionation schedules have been analyzed. These were delivered with higher total dose in the same interval of time or same dose with reduced interval of time. Increasing overall tumour dose or reducing overall treatment time prevents resistance and hence results in improved loco-regional control.
Hyper-fractionation schedule comprises of multiple fractions per day with reduced dose per fraction. This reduction in dose per fraction reduces the late toxicity in spite of increase in the total dose.
MARCH meta-analysis done in 2006 showed that altered fractionation schedules showed a significant benefit (p <0.001) in loco-regional control as compared with conventional radiotherapy. However there was no effect on distant metastases. Of all the altered fractionation schedules hyper-fractionation with twice daily fractionation had the greatest benefit with absolute benefit of 8% in overall survival at five years [5]. The combinations of radiobiological effect of hyper-fractionation together with reduced tissue toxicity effect of IMRT were studied in this trial.
This paper is mainly intended to study the technical details of the combination of hyper-fractionation and intensity modulated radiotherapy. The prescription and dose reporting was done according to the ICRU Report No. 83. D95% of all target volumes (GTV, CTV1 and CTV 2) received greater than 95% of the planned absorbed dose in all three patients. All three patients received greater than 90% of the prescribed dose to 98% of target volume. All three patients had maximum doses less than 107% of prescribed dose to the HRV. The mean and median (50%) dose of OARs received by all patients were within standard limits. All the doses were according to the ICRU report No 83 that shows that this combination of hyper-fractionation and IMRT technique is feasible.
All three patients had issues with tolerating the treatment well though they had completed the treatment well within the specified time of 60 days. They had breaks in the 4th or 5th wk of therapy, which is not ideal. The maximum toxicity for clinical mucositits was grade III seen only in one patient and rest all patients had grade II mucositis. Rest of the toxicities like radiation dermatitis, functional mucositis and swallowing function were grade II in all patients. The quality of life assessment showed increased pain during the fourth and fifth week, but did not result in additional feeding procedures in any of the patients. Previously reported phase III trials with hyper-fractionation showed improved loco-regional control however there was increased acute toxicity [6,7]. A phase II trial which combined concurrent weekly Cisplatin and hyper-fractionated IMRT in Stage III and IVA head and cancers reported good loco-regional control but had grade III toxicity in mucositis (38%), fatigue (28%), dysphagia (28%), and leukopenia (26%) [8]. But this trial had used only 70Gy total dose to GTV at 1.25Gy twice daily and did not attempt dose escalation. In comparison, a dose escalation to 80Gy with manageable acute toxicity is a point in favour of HF-IMRT technique. This should be applied on a larger series of patients in trial setting to look in to the actual incidence of acute toxicity and tolerance and compared with previously reported hyper-fractionation trials using conventional planning and treatment delivery techniques. It may also be suggested that hyper fractionated IMRT should be compared in trials with standard fractionation and chemo-radiotherapy settings to assess the tolerance and the efficacy.
Conclusion
Combining inverse planning and intensity modulation with hyper fractionation seems to promise reduction of toxicity as compared to earlier reported trials. The present study, which was a series of three patients, showed that the combination of hyper-fractionation and IMRT is feasible. The regimen had significant acute toxicity. The tolerance of this regimen cannot be commented from this short series.