Unilateral Obstructive Emphysema in Infancy due to Mediastinal Bronchogenic Cyst-Diagnostic Challenge and Management
Leena Robinson Vimala1, Ravi Kishore Barla Sri Sathya2, Arul Premanand Lionel3, Jeenapalli Srinivasa Kishore4, Kirubakaran Navamani5
1Assistant Professor, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India.
2Associate Professor, Department of Pediatric Surgery, Christian Medical College, Vellore, Tamil Nadu, India.
3Assistant Professor, Department of Pediatrics, Christian Medical College, Vellore, Tamil Nadu, India.
4Resident, Department of Pediatric Surgery, Christian Medical College, Vellore, Tamil Nadu, India.
5Resident, Department of Pediatrics, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Leena Robinson Vimala, Assistant Professor, Department of Radiology, Christian Medical College, Vellore-632004, India.
E-mail: leenarv76@gmail.com
Bronchogenic cysts are the most common cystic mediastinal lesion in children. Bronchogenic cyst causing unilateral obstructive emphysema is a rare presentation. We report the case of a one and half month old infant who presented with respiratory distress which was initially suspected as left pneumothorax on frontal chest radiograph but was later found to be due to hyperinflated left lung and hence the possibility of congenital lobar emphysema was considered. CT thorax and limited MRI sections revealed a cystic lesion in mediastinum causing obstructive emphysema and mediastinal displacement. He underwent an emergency thoracotomy and excision of the cyst via an extrapleural approach. Post operatively, rapid improvement of the infant was noticed both clinically as well as radiologically. Cross sectional imaging like CT or MR is required for reaching the correct and early diagnosis in paediatric patients with respiratory distress, when there is diagnostic dilemma based on chest radiograph.
Cystic lesion, Mediastinal displacement, Respiratory distress
Case Report
A one and half month old infant was brought to the paediatric emergency department in June 2014 with complaints of fever and fast breathing of one week duration. He was evaluated in a local hospital and was suspected to have pneumothorax on chest radiograph and hence referred to our institution for further management of pneumothorax.
He was the first child to non-consanguineous parents born by normal vaginal delivery at term. His neonatal period was uneventful and he was feeding well and active till he developed the above symptoms. At admission to emergency department, he had tachypnoea and severe respiratory distress. In spite of severe respiratory distress he was alert. His respiratory system examination revealed decreased air entry on the left side. No other dysmorphic features were noticed. In the emergency department chest radiograph was done. As the clinicians initially suspected pneumothorax, an emergency needle thoracostomy was done by inserting the needle in the left second intercostal space; minimal air bubbling was noticed in the underwater seal. He was started on high flow oxygen and admitted to paediatric ICU.
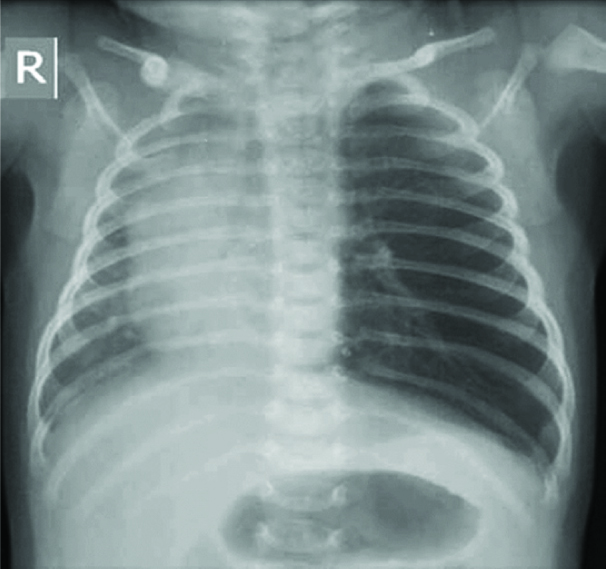
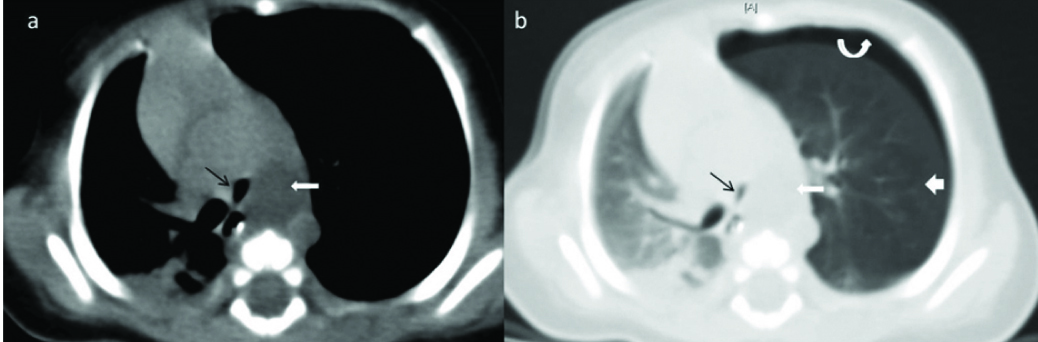
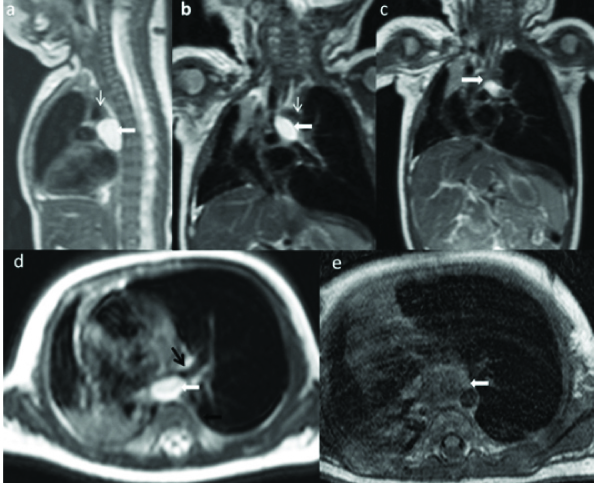
However, his symptoms were not improving and an intercostal drain was placed as an emergency measure. The chest radiograph was reviewed and a differential diagnosis of congenital lobar emphysema was also considered as there was hyperinflation of the left lung with paucity of vessels and the mediastinum was shifted to the right [Table/Fig-1]. CT thorax was done to confirm the diagnosis. Limited MRI sections were also done for better characterisation of the mediastinum. Imaging revealed a well-defined oval shaped lesion located just posterior to the left main bronchus, left lateral to thoracic oesophagus and just inferomedial to distal aortic arch [Table/Fig-2a,b&3a-c]. The lesion was compressing the left main bronchus and was causing obstructive emphysema in the form of hyperinflated left upper and lower lobes with normal vascular divisions which are widely separated within the overinflated lung [Table/Fig-2b,3c]. Small pneumothorax was also noted. There was herniation of left lung into the right hemithorax with mediastinal shift to the right and associated compressive atelectasis of right rightlung [Table/Fig-2b]. The lesion was hypodense on noncontrast CT andwas hyperintense on T2WI and intermediate signal intensity on T1WI [Table/Fig-3d,e]. Differential diagnoses considered were bronchogenic cyst and oesophageal duplication cyst.
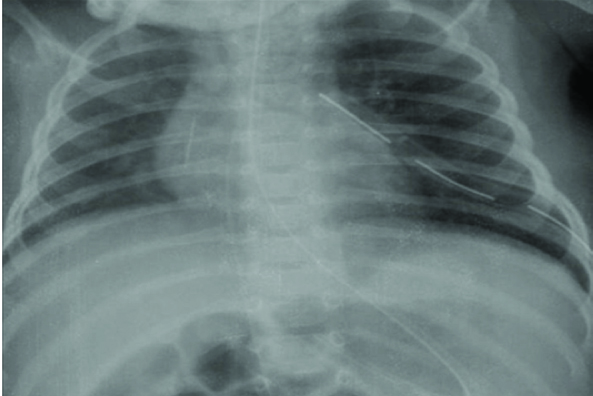
After obtaining written surgical consent from the parents explaining the risks, the child underwent emergency left posterolateral thoracotomy. Pleura were reflected off the thoracic wall and the arch of the aorta was exposed. A cystic lesion was seen within the arch, just medial to the vagus nerve [Table/Fig-4]. Blunt dissection was done around the cyst with a peanut gauge on clamp. A blood vessel seen supplying the cyst was ligated and the excision was completed. There was no communication with the airway or the esophagus. An intercostal drain was left in the extrapleural space and the thoracotomy was closed. Postoperatively, the child improved rapidly as was evident in the fifth post op day chest radiograph with resolution of hyperinflation of left lung with return of mediastinum to normal position [Table/Fig-5]. The child was discharged once the intercostal drain was removed. Histopathologic examination of the specimen confirmed the lesion as bronchogenic cyst.
Discussion
Bronchogenic cysts are the most common cystic lesions of the mediastinum in children [1]. Bronchogenic cysts arise from abnormal budding from the ventral segment of primitive tracheobronchial tree and accounts for 20–30% of congenital bronchopulmonary foregut 4cystic malformation. Depending on the stage of airway development at which abnormal budding happens, the location of the bronchogenic cysts varies. If occurs at the end of carina or first order bronchi, it will be of mediastinal or subcarinal location. If the abnormal budding occurs at the tracheobronchial tree, intraparenchymal bronchogenic cyst occurs. If the abnormal branching loses its connection with patent bronchus, ectopic bronchogenic cyst occurs [2]. Almost 25-30% of bronchogenic cysts remain asymptomatic. Symptomatic cases usually manifest in early childhood, but symptoms can develop at any age. Bronchogenic cysts can cause symptoms either due to mass effect or due to direct pressure on an airway leading to air trapping or due to secondary infection. Two-thirds of patients are diagnosed due to symptoms such as cough, wheezing, stridor, dyspnoea, dysphagia or even chest pain [3,4].
Our patient presented with respiratory distress and had unilateral hyperlucent lung. The common differentials to be considered in case of unilateral hyperlucent lung in children are pneumothorax, congenital lobar emphysema, pneumatocele, congenital lung cyst, diaphragmatic hernia and obstructive lobar emphysema. It is difficult to differentiate between congenital lobar emphysema and obstructive lobar emphysema on chest radiograph. Cross sectional imaging like CT or MR is required to differentiate between congenital lobar emphysema and obstructive lobar emphysema [5].
Congenital lobar emphysema is characterized by the overinflation of a pulmonary lobe. Exact aetiology is uncertain in almost 50% of cases, congenital cartilage defect or absence may be seen in 25% of cases. In the rest of the 25% of cases, varied aetiologies leading to intrinsic bronchial obstruction could be identified [6]. On the contrary, obstructive lobar emphysema could result either due to endobronchial obstruction like foreign body, mucus plugs or due to extrinsic compression from any mediastinal lesions like lymph nodes, mediastinal cyst, and vascular anomalies [2]. Multilobar involvement of the same lung is also favour congenital lobar emphysema over obstructive emphysema.
In our case, the obstructive emphysema of the left lung was due to a mediastinal bronchogenic cyst, compressing the left main bronchus. Mediastinal bronchogenic cyst causing unilateral obstructive emphysema in infants is a rare presentation and only a few cases are reported in the literature [5,7-10]. Mediastinal bronchogenic cysts can produce lobar or pulmonary emphysema by obstructing the lobar or main bronchus. Partial obstruction can lead to check valve phenomenon resulting in obstructing emphysema as demonstrated in our case.Imaging will help to assess the location, morphological features and enhancement pattern of bronchogenic cyst and its relation with the tracheobronchial tree. McAdams et al., [11] has highlighted the typical features of bronchogenic cyst as a well-defined lesion with fluid or soft tissue attenuation and role of MR imaging to elucidate the cystic nature of the lesion [11].
It is important to differentiate between the congenital lobar emphysema and obstructive lobar emphysema as the treatment varies between the two. Lobar resection is required for congenital lobar emphysema whereas uncomplicated obstructive lobar emphysema will resolve with removal of obstruction.
Frontal chest radiograph reveals hyperinflation of left lung with shift of mediastinum to the rightlung
CT thorax section in mediastinal (A) and lung window (B) shows hyperinflated left lung (thick white arrow). Well defined hypodense lesion (thin white arrow) in the mediastinum, located posterior to left main bronchus causing compression and narrowing of the left main bronchus(thin black arrow). Small amount of pneumothorax (curved white arrow)
MRI thorax T2WI sagittal (a) and coronal (b) & (c) sections show T2 hyperintense lesion (white arrow) located just inferior to aortic arch (thin white arrow). (d) T2WI axial image shows the lesion causing compression on the left main bronchus (thin black arrow). (e) T1WI image reveals the intermediate signal intensity of the lesion
Intra operative photograph demonstrating the cystic lesion (C) located within the aortic arch (A), just medial to vagus nerve (V) and right pulmonary artery (P)

Fifth postoperative day frontal chest radiograph demonstrates resolution of hyperinflation of left lung with return of mediastinum to normal position
Conclusion
In our case, initially there was diagnostic dilemma between pneumothorax and congenital lobar emphysema based on chest radiograph. However, CT and MR imaging evaluation helped to identify the mediastinal bronchogenic cyst which caused compression of the left main bronchus resulting in the obstructive emphysema of the left lung. Correct and early intervention was possible because of the imaging diagnosis which resulted in the quick recovery of the patient from the symptoms with resolution of obstructive emphysema in the follow up chest radiograph.
Consent: A written informed consent was obtained from the parents of the child for publication of this case report and the accompanying images (chest radiograph, CT& MR images, per operative photograph).
[1]. CD Wright, Mediastinal tumors and cysts in the paediatric populationThorac Surg Clin 2009 19(1):47-61. [Google Scholar]
[2]. A Jiwane, T Kumar, R Kutumbale, D Bhusare, P Kothari, B Kulkarni, Bronchogenic cyst with stridor and unilateral obstructive emphysema: an unusual presentationJ Indian Assoc Pediatr Sur 2001 6(3):95-98. [Google Scholar]
[3]. ME Ribet, MC Copin, BH Gosselin, Bronchogenic cysts of the lungAnn Thorac Surg 1996 61:1636-40. [Google Scholar]
[4]. J Goswamy, S de Kruijf, G Humphrey, MP Rothera, IA Bruce, Bronchogenic cysts as a cause of infantilestridor: case report and literature reviewJ Laryngol Otol 2011 125(10):1094-97. [Google Scholar]
[5]. M Zedan, MA Elgamal, K Zalata, N Nasef, A Fouda, Progressive stridor: could it be a congenital cystic lung diseaseActa Paediatr 2009 98(9):1533-36. [Google Scholar]
[6]. I Karnak, ME Senocak, AO Ciftci, N Büyükpamukçu, Congenital Lobar Emphysema: Diagnostic and Therapeutic ConsiderationsJ Pediatr Surg 1999 34(1):1347-51. [Google Scholar]
[7]. S Aktou, G Yuncu, H Halilçolar, S Ermete, T Buduneli, Bronchogenic cysts: clinicopathological presentation and treatmentEur Respir J 1996 9(10):2017-21. [Google Scholar]
[8]. T Sata, Y Shiga, R Nakanishi, K Yasumoto, A Shigematsu, Respiratory compromise and dramatic chest X-ray changes during general anaesthesia in a patient with a bronchogenic cystAnaesthesiology 1999 90(3):911-13. [Google Scholar]
[9]. RF Weichert, ES Full, CW Pearce, WW Waring, Bronchogenic cyst with unilateral obstructive emphysemaJ Thorac Cardiovasc Surg 1970 59(2):287-91. [Google Scholar]
[10]. M Khemiri, M Ouederni, FB Mansour, S Mansour, Bronchogenic cyst: An uncommon cause of congenital lobar emphysema.Respiratory Medicine 2008 102:1663-66. [Google Scholar]
[11]. HP Mc Adams, WM Kirejczyk, ML Rosado-de-Christenson, S Matsumoto, Bronchogenic cyst: imaging features with clinical and histopathologic correlationRadiology 2000 217(2):441-46. [Google Scholar]