Subhallucal Interphalangeal Sesamoiditis: A Rare Cause of Chronic Great Toe Pain
Sandeep Kumar1, Rajagopal Kadavigere2, Radha Puppala3, Anurag Ayachit4, Ruchika Singh5
1 Assistant Professor, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, India.
2 Professor, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, India.
3 Junior Resident, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, India.
4 Associate Professor, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, India.
5 Junior Resident, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandeep Kumar, Assistant Professor, Department of Radiodiagnosis, Kasturba Medical College, Manipal, Karnataka-576104, India.
E-mail: drsandeepkumarradiologist@gmail.com
Subhallucal interphalangeal sesamoiditis presenting as chronic great toe pain is a rarely reported clinical entity, being often overlooked and misdiagnosed for other pathologies. By altering the biomechanics of the movements at great toe, the interphalangeal sesamoid is prone to various painful pathologies like trauma, infection, degeneration, osteonecrosis and inflammation. Imaging plays an important role in narrowing down the differentials and guiding for appropriate therapy. Herein, we present a neglected case of hallucal interphalangeal sesamoiditis presenting as a case of chronic great toe pain and discuss the role of Magnetic resonance imaging (MRI) and Computed tomography (CT) scan in its diagnosis.
Case Report
A 49-year-old man, bus driver by occupation presented to our hospital’s outpatient department with complaints of right forefoot pain, since 5 years. The pain was localized over the plantar aspect of great toe, predominantly in the region of interphalangeal joint and was aggravated during application of brakes while driving. He had been previously investigated for the same and a Magnetic Resonance Imaging (MRI) scan performed 3 years back was reported to be essentially normal. Physical examination of the patient revealed mild antalgic gait. On clinical examination, severe tenderness and discomfort was found on palpation over the first interphalangeal joint at the plantar aspect of the proximal phalanx with no obvious swelling or redness. Forced flexion of the great toe against resistance revealed pain. No obvious restriction of active and passive movements could be appreciated. Plain radiograph of foot (Antero-posterior and lateral view) revealed a small bone fragment of approximate size 4x3 mm at the plantar aspect of the head of proximal phalanx [Table/Fig-1a,b]. MRI revealed a smooth edged and well corticated triangular ossicle embedded superficially within the tendon of flexor hallucis longus on the plantar aspect of interphalangeal joint of great toe with bone remodelling in the form of exaggerated concavity of the adjacent head of proximal phalanx of great toe [Table/Fig-2a-c]. Fat suppressed short tau inversion sequences (STIR) revealed marrow oedema within the sesamoid bone [Table/Fig-2d,e]. No abnormal associated soft tissue lesion was seen. Physiological fluid was seen in interphalangeal and metatarsophalangeal joints of great toe. No bony fracture, destruction or erosion was seen. Joint space appeared to be maintained.
Plain radiograph of right Foot AP (A) and lateral (B) views reveal a small well defined bone fragment at the plantar aspect of proximal phalanx of great toe (arrow)

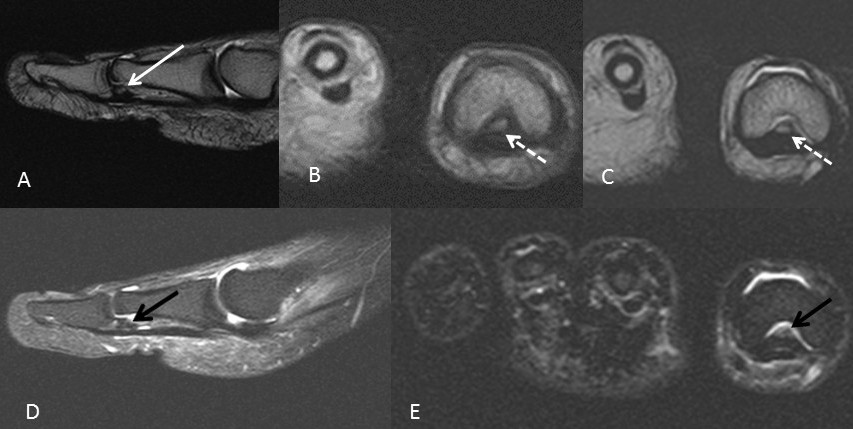
Magnetic Resonance Imaging. T2- weighted sagittal (A) and coronal (B) and T1- weighted coronal (C) images reveal a sesamoid bone embedded superficially within the flexor hallucis longus tendon (white arrow). STIR weighted sagittal (D) and coronal (E) images reveal hyperintense marrow signals within the subhallucal sesamoid (black arrow)
Correlated Computed Tomography (CT) confirmed the location and smooth margins of the subhallucal sesamoid bone [Table/Fig-3a-c]. No fracture or sclerosis was seen.
CT scan coronal (A) and sagittal (B,C) images accurately localises the well defined smooth edged bone ossicle at the plantar aspect of the proximal phalanx of great toe

Based on the clinical and imaging findings a diagnosis of hallucal interphalangeal sesamoiditis was made. The patient was treated by local injection of 1 ml of 0.125% levo-bupivacaine mixed with 10 mg of triamcinolone acetonide between the sesamoid bone and flexor hallucis longus tendon under ultrasound guidance. The patient was pain free within 10 min. Furthermore, the patient was advised with placement of a soft pad within the shoe underneath the symptomatic area and prescribed oral analgesics for two months. However the patient was lost on follow up.
Discussion
Sesamoid by definition refers to a bone, partially or completely embedded in a tendon or joint capsule. Their function is to protect the tendon from injury by reducing friction [1]. Sesamoids in the foot and ankle vary widely in their prevalence and appearance. Usually the sesamoids are asymptomatic, but they too can become painful by getting afflicted by any of the common osseous pathologies namely inflammation, infection, osteonecrosis, traumatic events, degeneration and likewise [2]. Sesamoiditis refers to inflammation of the sesamoid bone and/or its supporting apparatus, with resultant pain in its anatomical region [3]. Symptomatic interphalangeal sesamoids are rare, being often overlooked and misdiagnosed for unrelated conditions [4]. Subhallucal interphalangeal sesamoid is one of the rare conditions known to cause severe great toe pain. Lack of awareness of this particular entity leads to misdiagnosis, delayed treatment and contributes to significant morbidity. To complicate matters further, the hallucal interphalangeal sesamoid may be completely ossified in some, whilst in others; it may be purely fibrocartilagenous, making it almost indistinguishable from the surrounding soft tissues [5]. Thus, identification of this entity on radiographs is not always possible.
The incidence of the interphalangeal joint sesamoid of great toe is 2-13% [6]. On imaging, the sesamoid is usually seen as an ossicle with portion of it being embedded within the flexor hallucis tendon at the interphalangeal joint of great toe.
Interphalangeal sesamoid is known to cause a decrease in the range of motion at the first metatarsophalangeal joint, with consequent hyperextension of the interphalangeal joint of the hallux. Due to altered local biomechanics, an increase in pressure is exerted in the area located beneath the interphalangeal joint which may result in a painful hyperkeratotic callous on the plantar aspect of the foot [5,6].
Sesamoiditis is a diagnosis of exclusion with more common pathologies causing sesamoid related pain being fracture, osteonecrosis, degenerative joint disease, chronic bursitis, and neural entrapment [4]. Plain radiographs are usually employed as the first line of investigation, but it might fail to pick up the condition due to faulty technique like improper positioning, small size of the sesamoid and its presence in its non radio-dense fibrocartilagenous form. CT, Scintigraphy and MRI play an important role in assessment of hallucal sesamoiditis, by accurately localising it, describing its morphology in exquisite detail and thus help differentiate it from other causes of great toe pain.
On MRI, sesamoiditis is described to show bone marrow oedema confined to the sesamoids without marrow changes in adjacent bones. On CT they show smooth corticated margins without any sclerosis. They show increased uptake on 99mTc-MDP bone scan. However, since increased uptake is also seen in conditions like osteonecrosis, fracture and infection, Scintigraphy has only limited role to play in the evaluation of sesamoiditis [4,6].
CT and MRI can conclusively differentiate the poorly corticated margins of the irregular bony fragments of fracture from the smooth corticated margins of sesamoiditis. They can also demonstrate the callus formation associated with long standing stress fractures.
Osteonecrosis shows features of marrow oedema in early stages with sclerosis predominating in late stages. Thus in early stage they are hyperintense on STIR and mildly hypointense on T1W images, but in later stages, due to sclerosis they appear hypointense on all sequences. Since both early stage osteonecrosis and sesamoiditis share the same imaging features of bone marrow oedema, MRI cannot reliably differentiate between the two. However, CT can differentiate between the two by demonstrating increased sclerosis in osteonecrosis, compared to the normal density seen in sesamoiditis [6].
Osteomyelitis of the hallucal sesamoid is usually a direct extension from infective foci in the adjacent soft tissue or from the adjoining infected joint. Osteomyelitis presents with radiographic features of cortical erosion or destruction with periosteal reaction and associated soft tissue swelling and collections. On MRI they show typical marrow changes of STIR and T2W hyperintensity with T1W hypointensity and robust post contrast enhancement. CT and MRI by demonstrating lack of cortical erosion or destruction with lack of any associated soft tissue can effectively rule out osteomyelitis as a differential for sesamoiditis.
The treatment of hallucal interphalangeal sesamoiditis is primarily conservative, mainly directed towards relieving pain and discomfort. Local injection with long acting anaesthetic agent mixed with steroids provides effective symptomatic relief and should be tried before surgical excision. Alternatively a custom-moulded orthosis or a soft pad placed just proximal to the lesion often alleviates symptoms. An extra-depth shoe (increased vertical volume) with a prefabricated or custom insole can also be used. Keratotic callus if present may be debrided or shaved [4,7]. Rarely in athletes, when there is significant associated occupational hindrance may radical surgical excision in the form of sesamoidectomy are attempted. However, the possibility of recurrence of hyperkeratotic scar and major complication of detachment of the flexor halluces longus tendon at the time of excision must be borne in mind [7,8].
Conclusion
Subhallucal interphalangeal sesamoiditis, though rarely documented in literature, is a potential cause of severe chronic great toe pain. High index of suspicion should be kept for this condition as it can be easily overlooked and potentially be misdiagnosed as unrelated conditions. Imaging in concert with clinical findings plays an important role by narrowing down the differentials and guiding the appropriate therapy. The condition is usually treated conservatively and surgery is reserved for intractable cases.
[1]. Sarrafian SK, Osteology. In: Sarrafian SK (ed)Anatomy of the foot and ankle 1993 2nd editionPhiladelphiaLippincott:89-112. [Google Scholar]
[2]. Atiya S, Quah C, Pillai A, Sesamoiditis of the metatarsophalangeal jointOA Orthopaedics 2013 1:19 [Google Scholar]
[3]. Sharma P, Singh H, Agarwal KK, Sudhir KS, Khangembam BC, Bal C, Utility of 99mTc-MDP SPECT-CT for the diagnosis of sesamoiditis as cause of metatarsalgiaIndian J Nucl Med 2012 27:45-47. [Google Scholar]
[4]. Shin HY, Park SY, Kim HY, Jung YS, An S, Kang DH, Symptomatic Hallucal Interphalangeal Sesamoid Bones Successfully Treated with Ultrasound-guided Injection - A Case ReportKorean J Pain 2013 26:173-76. [Google Scholar]
[5]. Roukis TS, Hurless JS, The hallucal interphalangeal sesamoidJ Foot Ankle Surg 1996 35:303-08. [Google Scholar]
[6]. Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF, Roemer FW, Sesamoids and accessory ossicles of the foot: anatomical variability and related pathologyInsights Imaging 2013 4:581-93. [Google Scholar]
[7]. Del Rossi G, Great toe pain in a competitive tennis athleteJ Sports Sci Med 2003 2:180-83. [Google Scholar]
[8]. Valinsky MS, Hettinger DF, Mortvedt JK, Hallux interphalangeal joint sesamoidectomy using minimal incision techniqueJ Am Podiatr Med Assoc 1989 79:60-64. [Google Scholar]