The Stomatognathic System requires a co-ordinated and a harmonious relationship between the muscles, bone, joints and teeth. All prosthetic rehabilitation is directed towards restoration of missing teeth and oral structures to reinstate this harmony. It is known that the lower third of the face presents two main positions in the maxillo-mandibular relation: the vertical dimension at rest (VDR) and the vertical dimension at occlusion (VDO) [1]. The physiologic rest position of the mandible, defined as “the habitual postural position of the mandible when the patient is relaxing comfortably in the upright position and the condyles are in a neutral unstrained position in the glenoid fossae” [2], is one of the most important position within this complex relationship.
Restoring the proper vertical dimension is further complicated because the rest position may be subjected to change [1,3]. The vertical relation of rest or postural position is a critical landmark in determining the vertical dimension of occlusion in the completely edentulous patients. The VDO can be obtained through several techniques: Unstrained lip contact most comfortable position, Phonetic, Facial aesthetic measurements, Swallowing technique, Electromyography, Boos Biometer and Cephalometric methods [1,4-9]. None of them is capable of achieving a precise and predictable VDO in the edentulous patient. However, among the functional or physiologic methods, Swallowing and Phonetics method has been used for determining the vertical dimension since long [10].
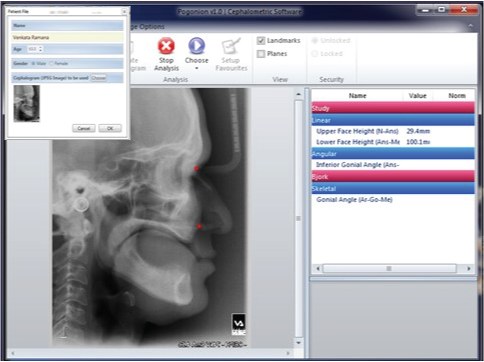
A computer assisted cephalometric program (PRO-CEPH V3) that applies cephalometric analysis as an objective method of diagnosis, treatment planning and determining VDO was indigenously developed by our research and development team at Kamineni Institute of Dental Sciences Narketpally, India. This software program was then used to assess, evaluate and compare the VDO recorded by the three physiological methods and also to investigate the possibility of predicting or correlating the clinical VDO through a linear measurement from the MFH:LFH (Middle facial height: Lower facial height) proportion and through an angular measurement measured from Gonial Angle (GA) using regression formula IGA=0.508 x ( GA-15.7) by computer assisted cephalometric mean where IGA refers to inferior gonial angle [11].
The aim of this study was to compare the vertical dimension in edentulous patients recorded by using three physiological methods with the aid of digital cephalometric tracings using indigenously developed PRO-CEPH V3 software.
Materials and Methods
The present study was conducted in the Department of Prosthodontics at Kamineni Institute of Dental Sciences, Narketpally for which 50 dentulous patients (Group A) and 25 edentulous patients (Group B) were selected based on the inclusion and exclusion criteria.
Inclusion criteria for the dentulous subjects
Male or female dentulous patients of age 20-35 years.
Angle Class I molar relationship with normal over jet and over bite.
Full complement of permanent teeth till the second molar (third molar may or may not be present).
Exclusion criteria for the dentulous subjects
Temporomandibular joint disorder.
Any prior orthodontic treatment and/ or prosthetic replacement of teeth.
Medical conditions (e.g. Diabetes mellitus, Arthritis, Osteoporosis)
Inclusion criteria for the completely edentulous patients
Male or female completely edentulous patients of age 45-75 years.
Good denture-supporting tissues.
Class-I Ridge relationship.
Good neuromuscular control.
Exclusion criteria for the completely edentulous patients
Temporomandibular joint disorders.
Highly resorbed ridge.
Systemic disorders.
A lateral cephalometric radiograph was taken for all the dentulous subjects (Group A) at Maximum Intercuspation (VDO). Three Lateral cephalometric radiographs were obtained for all edentulous patients (Group B) at the VDO following three different techniques firstly using Niswonger’s method (Group B1), followed by Phonetics method (Group B2), and the Swallowing threshold method (Group B3), subsequently.
Group B1: Niswongers method – Cephalogram 1
“Vertical Dimension at rest (VDR) =Vertical Dimension at occlusion (VDO) + Free-way space” was used to evaluate the vertical dimension at occlusion for the first cephalogram taken with Niswonger’s physiological method for all edentulous patients. Point marked adhesive triangles were placed on tip of the nose and the most prominent part of the chin. Pre-adjusted occlusion rims were then placed in the mouth. The patients were asked to swallow and relax, a freeway space of 2mm was confirmed at this position and the VDR was recorded between the points by means of a calliper. Lateral cephalogram was made later with the rims in contact at the VDO [Table/Fig-1].
Niswonger’s method to record Vertical dimension at occlusion

Group B2 : Phonetics method – Cephalogram 2
The vertical dimension at rest was recorded while the patient was in a natural, comfortable position and VDR was confirmed by phonetic sounds m, m, m and minimal speaking space of 1 mm with 'S' sound. Lateral cephalogram was made later with the rims in contact at the VDO [Table/Fig-2].
Phonetics method to record Vertical dimension at occlusion
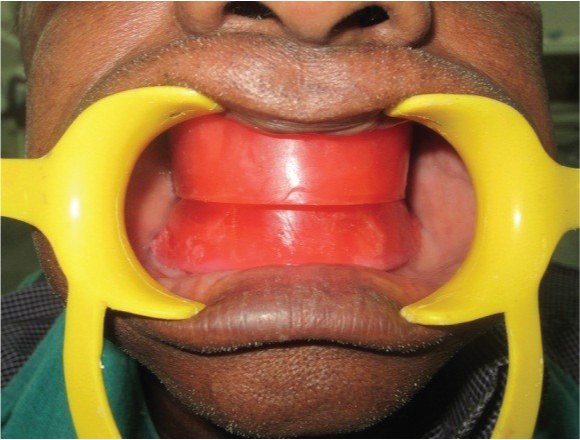
Group B3: Swallowing Threshold method – Cephalogram 3
The upper and lower occlusion rims were placed in the mouth with cones of Aluwax placed on top of the lower occlusion rim, and the patient was requested to swallow several times. As the patient swallowed, the soft wax was reduced to the vertical dimension at occlusion [Table/Fig-3]. Cephalogram was taken at Vertical dimension of occlusion by placing upper and lower record base and patient was instructed to slightly touch their rims during exposure. The radiographic unit used for digital exposures in all the study groups was Digital Cephalogram apparatus ROTOGRAPH EVO, with the recommended settings of 72 kV and 6 mAS in 4.5sec for single exposure. All digital images were then compressed in JPEG image (jpg) format and imported into the tracing software. All images were of good quality and had no artifacts that might interfere with the location of the anatomical points. Cephalometric analyses were performed with the aid of a cephalometric software program indigenously developed by our research and development team at Kamineni Institute of Dental Sciences (PRO-CEPH V3). For the computerized measurements, direct digital images were imported to the PRO-CEPH V3 software program which automatically generates measurements after digitizing a set of landmarks.
Swallowing threshold method to record Vertical dimension at occlusion

Cephalometric Landmarks and Angles Used in the Study
The cephalometric analysis was based on the Ricketts cephalometric analysis and the landmarks used were as follows [Table/Fig-4].
Cephalometric analysis software
Anterior Nasal spine (ANS) - The anterior point of the nasal floor; the tip of the pre-maxilla in the midsagittal plane.
Nasion (N) - Most anterior point of fronto nasal suture in the mid sagittal plane.
Menton (M) - The lowest point of the contour of the mandibular symphysis.
Articulare point (Ar) -The point of intersection of the images of the posterior border of the condylar process of the mandible and the inferior border of occipital bone.
Cephalometric analysis software showing distances and angles
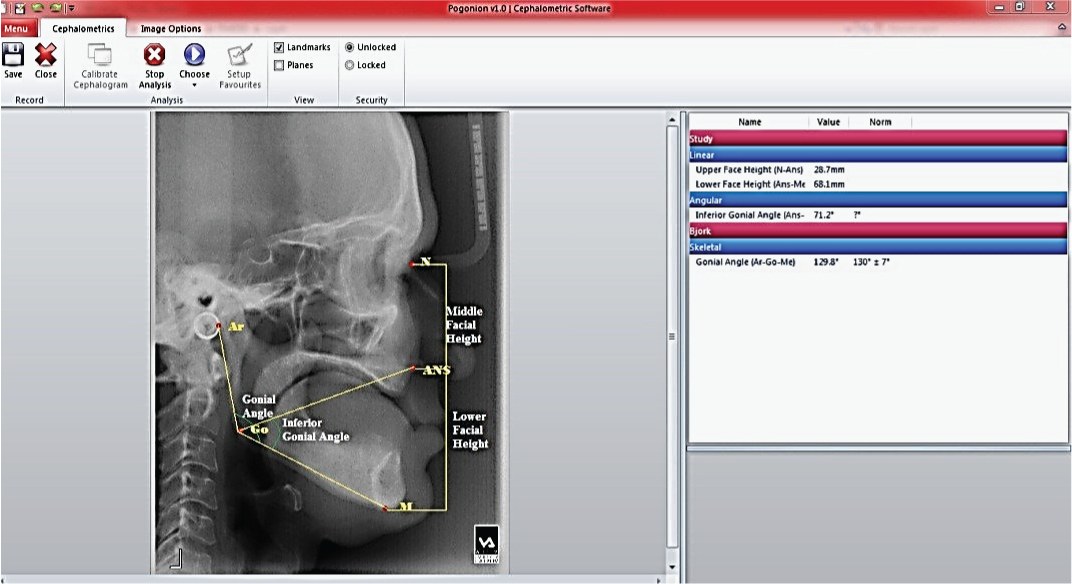
Middle face height (MFH) -Measured between Nasion and Anterior Nasal Spine.
Lower face height (LFH) - Measured between Anterior Nasal Spine and Menton.
Inferior Gonial Angle (IGA) -The Inferior Gonial angle measures the lower facial height from the Gonion point to the Anterior Nasal Spine and Anterior Nasal Spine to the Menton.
Gonial Angle (GA) – Gonial angle measured from the Articulare to the Gonion point and Gonion point to the Menton.
The cephalograms were then digitised in JPEG format and loaded into the PRO-CEPH V3 software. The various landmarks were identified and marked. Linear and the required angular measurements were then tabulated by the software and recorded.
Statistical Analysis
A statistical analysis was applied to compare the measured lower facial height and also the ratio of Middle and Lower facial heights between Group A and Group B and also within Group B between Subgroups B1, B2 and B3 using Analysis of Variance (ANOVA Test). All values ≤ 0.5 were considered statistically significant. Post-Hoc test was used for multiple comparisons between the groups.
Results
In the present study we compared the measurements of lower facial height (LFH) determined by Niswonger’s, phonetics and swallowing threshold method by linear measurement after identifying the landmarks through the PRO-CEPH V3 Software. The lower facial height, given by the height between Anterior Nasal Spine and Menton (ANS-M) recorded the value of Vertical Dimension of Occlusion (VDO) [Table/Fig-5]. In this study, the mean value of VDO was 46.3mm (SD 4.3) with swallowing threshold method (Sub Group B3:n=25), 45.11mm (SD 3.0) with phonetics method (Sub Group B2:n=25) and 44.51mm (SD 4.5) with Niswonger’s method (Sub Group B: n=25) [Table/Fig-6]. In this study, we calculated the proportion between the Middle Facial Height (MFH) and Lower Facial Height (LFH), measured between Nasion (N) and Anterior Nasal Spine (ANS), and Anterior Nasal Spine and Menton (Me) respectively. We found that there was stability in the skeletal VDO, corroborating that the proportion of 0.75 was present between MFH (N-ANS) and LFH (ANS-Me) [Table/Fig-7]. No significant difference was found in middle and lower third ratio when comparing the measurements with Niswonger’s method (Subgroup-B1), phonetics (Subgroup-B2) and swallowing threshold method (Subgroup-B3). In dentate patients the proportion between the middle and lower thirds of the face was found 0.75 and no significant difference was found [Table/Fig-7].
Linear Measurements- Lower Facial Height
| Group | n | Mean | Std. Deviation |
|---|
| A: DENTULOUS | 50 | 49.97 | 5.32 |
| B1:NISWONGER’S | 25 | 44.51 | 4.54 |
| B2:PHONETICS | 25 | 45.11 | 3.01 |
| B3:SWALLOW | 25 | 46.31 | 4.34 |
Linear Measurements – Ratio of Middle Facial Height to Lower Facial Height
| Groups | Methods | Ratio | Sig. |
|---|
| Dentate (Group-A) | Maximum intercuspation | MFH | 0.75 | 0.005 |
| LFH |
| Edentate (Group-B) | Niswonger’s (Sub-Group-B1) | MFH | 0.77 | 0.006 |
| LFH |
| Phonetics (Sub-Group-B2) | MFH | 0.75 | 0.005 |
| LFH |
| Swallowing threshold (Sub-Group-B3) | MFH | 0.73 | 0.007 |
| LFH |
The lower facial height is also given by the angle between Anterior Nasal Spine, Gonial point and Menton. (ANS-Go-M) described as the Inferior Gonial Angle (IGA). We compared the angular measurement values of IGA determined by Niswonger’s, phonetics and swallowing threshold method. The mean value of IGA for Niswonger’s method was 45.71 (SD 3.4) and 46.31 (SD 4.0) with Phonetics method and 47.61 (SD 3.8) with Swallowing threshold method. Swallowing method was, on average, 1.9 degree higher than IGA obtained with the Niswonger’s method and 1.3 degree higher than the Phonetics method. Statistically insignificant difference was found between Niswonger’s and Phonetics method (p>0.05). Statistically significant differences were found between Niswonger’s and Swallowing threshold methods (p<0.01) [Table/Fig-8]. The mean Gonial angle measured among dentulous (Group A) subjects was 123.73(SD = 2.62) which was lesser than that measured in the edentulous (Group B) subjects, which was 128.46 (SD 3.56). The mean difference in Gonial angle between the edentulous subjects (Group B) and the dentulous subjects (Group A) was 4.73 degrees. A Statistically significant difference in the Gonial Angle was observed between the dentulous and the edentulous (p<0.01) [Table/Fig-9].
Angular Measurements – Inferior Gonial Angle
| GROUPS | n | Mean | Std. Devtn. |
|---|
| A:DENTATE | 50 | 48.02 | 3.20 |
| B1:NISWONGER’S | 25 | 45.71 | 3.49 |
| B2:PHONETICS | 25 | 46.31 | 4.04 |
| B3:SWALLOW | 25 | 47.61 | 3.85 |
Angular Measurements – Gonial Angle
| Methods | n | Mean | Std. Deviation | Mean Difference | Sig. |
|---|
| Dentulous | 50 | 123.73 | 2.62 | 4.73 | 0.02 |
| Edentulous | 25 | 128.46 | 3.56 |
This study also compared the cephalometrically measured value of the Inferior Gonial Angle (IGAm) and the Inferior Gonial Angle calculated from the regression formula {IGAc = 0.508 x (GA -15.7)} [11] among edentulous subjects and dentulous subjects (in degrees). The mean inferior gonial angle of Cephalometric Measured value among dentulous (Group A) was 48.2 degrees (SD = 3.2) and 45.56 degrees (SD = 3.6) when calculated from the regression formula. Among edentulous subjects, with Niswonger’s method the measured value was 45.71 (SD 3.4) and 43.65 (SD 2.2) with calculated value. With Phonetics method 46.31 degrees (SD 4.0) was recorded from Cephalometric Measured value and 43.79 degrees (SD 3.2) was calculated from the regression formula. For swallowing threshold method Cephalometric Measured value was 47.61 degrees (SD 3.8) and calculated value was 45.23 degrees (SD 2.6). It was seen that there was a mean difference of approximately 2.3 degrees (SD 1.5) between the IGAm and IGAc within each group [Table/Fig-10].
Angular Measurement -Inferior Gonial Angle
| n | Measured Mean IGAm | Std. Deviation | Calculated mean IGAc | Std. Deviation |
|---|
| Swallowing threshold (Sub-Group-B3) | 25 | 47.61 | 3.85187 | 45.23 | 2.6 |
| Phonetics (Sub-Group-B2) | 25 | 46.31 | 4.04412 | 43.79 | 3.2 |
| Niswonger’s (Sub-Group-B1) | 25 | 45.71 | 3.49477 | 43.65 | 2.2 |
| Dentulous (Group A) | 50 | 48.02 | 3.20908 | 45.56 | 3.6 |
Cephalometric measured value and Calculated value from Regressional formula
Discussion
Cephelometric analysis of determing the vertical dimension in edentulous patients have been proven to be the most accurate and acceptable method till date [12]. Developments in computer technology have led to increasing use of digital systems both for tracing and analysing cephalometric films. Manual Cephalometric analysis is prone to errors in identification and measurements and requires more time for calculations. Computer Assisted-Cephalometric analysis however, improves the diagnostic value of cephalometry by reducing errors and saving time. It has been proved that Computerized cephalometry is a “smart service” which has revolutionized the dental profession providing precision and sophistication in clinical work [13]. Earlier studies revealed that computer-aided cephalometric analysis does not introduce greater measurement error than hand tracing, as long as landmarks are identified manually (Gravely and Benzies & Enlow and Hans) [14,15]. Computerized or Computer-Aided Cephalometric analysis eliminates the mechanical errors introduced by calibrated instrumentation. Computerized cephalometric analysis uses manual identification and location of anatomical or constructed landmarks points on digitized cephlogram image and then transfers it to computer software which completes the cephalometric analysis by automatically measuring distances and angles with respect to their corresponding landmarks [16]. In this study the software program, PRO-CEPH V3,was used to assess, evaluate and compare the lower facial height and therefore the vertical dimension at occlusion recorded by three physiological methods, Niswonger’s, Phonetics and Swallowing Threshold. It was also used to investigate the possibility of predicting or correlating the clinical VDO through a linear measurement from the MFH:LFH proportion and through an angular measurement of the Inferior Gonial Angle (IGAm) from the measured Gonial Angle (GA) and that calculated from a regression formula: IGAc=0.508 x ( GA-15.7) [11] by computer assisted cephalometric means. C Millet et al., [17] in their study compared the swallowing technique with Niswonger’s method and found that the VDO determined with the swallowing method was, on average, 2.0 mm higher than VDO obtained with the use of Niswonger’s method. However, there were no statistically significant differences in their study. In our study the VDO determined with the Swallowing method (Sub Group B3) was on average 1.2 mm higher than VDO obtained with the use of phonetics method (Sub Group B2) and 1.8 mm more from Niswonger’s method (Sub Group B1). Significant difference was found between Niswonger’s and Swallowing threshold method. (p<0.01) [Table/Fig-7]. These results coincide with the observations made in previous studies [18,19]. In our study, there was stability in the skeletal VD, corroborating that the proportion of 0.7 ± 0.2 was present between N-ANS and ANS-Me in both the Groups A and B. The results coincided with those recorded in studies carried out in the dental literature [20-22].
Phonetics method (Sub Group B2) showed more comparable values with the dentulous group (Group A) [Table/Fig-6]. The ratio of Middle facial and Lower facial heights in dentulous and edentulous subjects at vertical dimension of occlusion was comparable at 0.75 +_ 0.02. Taking these comparisons into conclusion within the limits of our study, it can be safely suggested that the LFH can be relatively predicted from the MFH and therefore help in predicting the VDO in the edentulous through cephalometric measurements and later also its clinical correlation.
In edentulous subjects, changes in the mandibular bone after tooth extraction include a chronic and progressive resorption of the residual ridge and may also present as a widening of the Gonial angle [1,18]. In the present study the edentulous subjects (Group B) recorded a mean Gonial angle of 128.4 than the dentulous subjects (Group A) who recorded a mean of 123.70 [Table/Fig-9]. There was a difference of an average of 4.73 between Groups A and B. The difference in the mean Gonial angles recorded in this study coincides nearly with the results recorded by Engstriimeta who compared 50 dentulous subjects with 50 edentulous subjects at various ages and found that the Gonial angle was 5° larger in the edentulous groups [23].
JD Orthlieb [11] found a simple regression from 505 adults, which was calculated between the Inferior Gonial Angle that estimates the lower facial height and the mandibular Gonial angle. It was possible to estimate, by calculation, the patient’s VDO using the regression formula IGA= 0.508 x (GA-15.7) where ‘IGA’ is the Inferior Gonial Angle and ‘GA’ is the mandibular Gonial angle. Many authors [11,24] suggested to record the VDO from Inferior Gonial Angle.
In our study the Inferior Gonial Angle was measured from the Mandibular Gonial angle cephalometrically using the PRO-CEPH V3 software (IGAm) and its value also calculated (IGAc) from Orthlieb’s regressional equation. It was seen that there was a mean difference of approximately 2.3 degrees (SD 1.5) between the IGAm and IGAc within each group irrespective of the sub groups [Table/Fig-10]. It was found that with 10 change in the IGA there was 1.05mm increase in the linear measurement of VDO. Correlations were more interesting than mean values because they were more specifically related to the patient. The concept of a vertical comfort range is generally accepted. Tryde et al., [25], in determining the VDO in edentulous patients, coined the term “comfort zone" for the range within which patients can tolerate VDO changes. The average comfort zone was relatively narrow i.e., 1.3mm. Dawson [26] recommend changing the VDO only if absolutely necessary to provide space for restorative materials and then by only the minimal amount required 1 to 1.5mm in a dentulous or partially edentulous patients. This suggests that both the values of the IGA with a small difference of 20 are comparable and that the Gonial angle can be used as a cephalometric means of predicting the IGA and therefore the VDO relatively consistently. However, this has to be evaluated over a larger sample size than that used in our study to conclusively state if the Regression formula can be used in the Indian populace to predict the VDO cephalometrically from the GA. If these calculated values indicate the same direction (increase the VDO, for example), the corroborating facts could help the clinical decision concerning the vertical dimension. This new hypothesis must be tested in future research.
Several methods, some physiological, some radiographical and some merely based on experience are taken upon by the practitioner to get him close to VDO in the edentulous patients. No single method can however claim to be the perfect answer. Various studies show that the VDO is not a fixed numerical figure but is interposed in a “comfortable functional range”. Therefore from the findings of our cephalometric study it is possible to assess the VDO from the middle facial height using the MFH:LFH proportion and also that the VDO can be inferred from the IGA calculated from the regressional formula using the Mandibular Gonial Angle therefore helping in predicting and clinically correlating the VDO in the edentulous.
Conclusion
Cephalometric study of the subjects with dentulous group included in this study provided important and specific parameters for optimal reconstruction of vertical dimension of occlusion in the treatment of edentulous patients. The indigenously developed software PRO-CEPH V3 is capable of making both the linear and angular measurement and therefore provide with relative credibility information regarding the possible VDO in the edentulous patients through cephalometric radiography. The use of the digital software minimizes the manual errors and provides precicional values of measurements in determining vertical dimensions in edentulous patients. Choosing a smart way to work saves clinician time as well as provides sophistication at clinical work.
Cephalometric measured value and Calculated value from Regressional formula