The CVJ refers to a bony enclosure where the occipital bone surrounds the foramen magnum, the atlas & the axis vertebrae. Because of the complex structures, CVJ instability is associated with diagnostic and therapeutic problems. Posterior CV fusion procedures have evolved a lot over the last couple of decades. Modern instrumentation using screw rod constructs have become the norm, compared to the ancient wiring techniques using contoured rods and bone grafts due to their better biomechanical profile [1]. CV Junction fusion procedures have over years remained a domain of few experienced Neurosurgeons with very few young Neurosurgeons being able to make a significant stride in this subspeciality of Neurosurgery. This may be largely attributed to the highly unforgiving nature of vital neurovascular structures in this region, where a small error could prove devastating in a highly compromised and compressed neurovascular tissue. Complex vascular anatomy with fairly common congenital bony and vascular anomalies has added to the complexities [2]. Adding to this is the question regarding what surgical procedure to choose in each patient. There has been a lookout for one such surgical procedure which would be inherently safe, simple, easily reproducible and biomechanically sound.
The current study is a descriptive analysis of the cases of CVJ instability treated by us with instrumentation using O-C1-C2 screw and rod construct fusion technique.
Materials and Methods
We conducted a retrospective, analytical study in which nine cases of CV junction instability treated and operated by first author at various hospitals in Mangalore, India during the time from January 2010 to March 2014 were analysed using various clinical, radiological and outcome parameters. The data was collected, analysed and evaluated using objective criteria. All patients underwent a thorough history taking, clinical evaluation and detailed perioperative imaging which included dynamic CV junction X-rays, CT scan and MRI scan preoperatively. Intra operatively, care was taken to avoid intubation and positioning related spinal cord compromise by using Fiber optic intubation and avoiding muscle relaxants during intubation and positioning. Clinical evaluation parameters included the comparison of preop and postop neck pain (Visual Analog Score (VAS) 1-10), muscle power (Grade 1-3/4/5), Tone (Modified Aschworth Score1-5) and functional outcomes using Karnofsy Outcome Score and Ranawat Classification (Grade 1/2/3A/3B). Radiological evaluation parameters included C2 pedicle diameter, Preop and postop Craniometric [3] measurements based on CV junction X-rays and CT scan (Clivus Canal Angle, Chamberlin’s line, Mac Rae’s line and Anterior Atlantodental interval), MRI evaluation to look for Myelomalacia, X-ray CVJ flexion and Extension studies to look for reducibility of Atlanto axial Dislocation. Other parameters that were analysed included the duration of surgery, intraoperative blood loss, any intraop vascular injury, postop wound complications and any postop mortality. Serial clinical evaluation was done and documented during follow-up. The follow-up duration ranged from 6- 24 months. Postoperatively X-ray and CT CV junction was done in all patients before discharge and serial X-ray CVJ (Open mouth AP & Lateral) were done at 3 months, 6 months and 1 year follow-up. Patients were advised neck immobilization using Philadelphia/ Hard Cervical collar for three months and to avoid outdoor contact sports and strenuous activities for 6-12 months.
Results
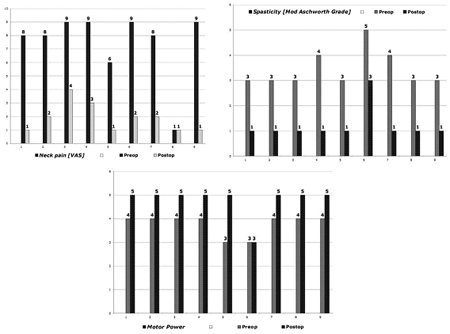
Most of the patients were in the 10-60 y age group. Congenital etiology was the most common. Other etiological factors were Degenerative, Rheumatoid and Post trauma. All patients presented with hypertonia. Neck pain was the second common symptom. Radicular pain was present in only two patients. All the patients presented with Myelomalacia which clinically and radiologically clearly evident. Syringomyelia was seen in four patients. Postoperatively, all the patients showed considerable reduction in neck pain (measured by Visual Analog Scale of 0-10) [Table/Fig-1]. Similarly, there was considerable reduction in Spasticity (Measured using Modified Aschworth Score) in all patients. All except one patient regained normal motor power postoperatively. The patient who did not improve in motor power postoperatively had Grade 5 spasticity, severe cord compression and significant restriction of respiratory capacity preoperatively. This patient became quadriplegic immediate postoperatively. He improved to preoperative status (Power 3/5) after IV Methyprednisolone infusion (as per NASCIS 3 protocol). We have used intraoperative prophylactic loading dose of IV Methylprednisolone (1 gm in adults and 500 mg in paediatric age group) in all our patients. The thickness of C2 pedicle is an important criteria in determining the feasabilty of C2 pedicle screw placement [4]. In our study the C2 pedicle diameters ranged from 2.5 mm to 6.5 mm. We could safely place 3.5 mm diameter pedicle screws in all of them using the technique described by Goel et al., [5] & Harm et al., [6]. The surgical procedures employed for Basilar invagination with irreducible AAD was C1-C2 joint distraction and placement of titanium spiked spacers [7] filled with autologous bone grafts harvested from spinous processes of cervical spine. Occipito cervical fixation was done using Occipital plate and bilateral C2 pedicle screws with or without C1 lateral mass screws. Only C1-C2 rod and screw fixation was done in reducible AAD. In AAD secondary to Rheumatoid arthritis we extended the C1-C2 fusion cranially to include the occiput as this being a progressive pathology, involvement of Occipito-atlantal joints at a later date can result in Basilar invagination. We have performed limited removal of posterior foramen magnum rim before C1-C2 joint opening and manipulation followed by C1 posterior arch excision after successful placement of screw and rod construct. We have not used iliac/fibular/rib bone graft as we feel that it adds to the morbidity and hampers early mobilization due to local pain at the donor graft site. Extending the surgical incision caudally to harvest spinous process grafts of lower cervical spine usually gives adequate volume of bone graft. C2 ganglionectomy followed by C1-C2 Joint opening was done in all (except 1) patients. We have liberally used bipolar electrocautery during C2 ganglionectomy, as a result of which all (except 1) patients had minimal (below 100 ml) blood loss. The Clival canal angle became more obtuse in all except 1 patient in whom C1-C2 joints were not opened [Table/Fig-2]. There was reduction in atlantodental interval in all (except one) patients postoperatively. C1-C2 joint spacers with bone graft were placed in six patients, whereas only bone grafts were placed in the joints in three cases of reducible AAD. The mean duration of surgery was 5.22 h.
Shows comparison of preop and postop neck pain, spasticity and motor power. Postoperatively there is visibly obvious reduction in neck pain and spasticity with improvement in motor power in most of the patients.
Shows preoperative and postoperative anterior atlantodental interval, clivus canal angle and the postoperative change seen. One can note the reduction in postoperative anterior atlantodental interval and increased clivus canal angle in most of the patients

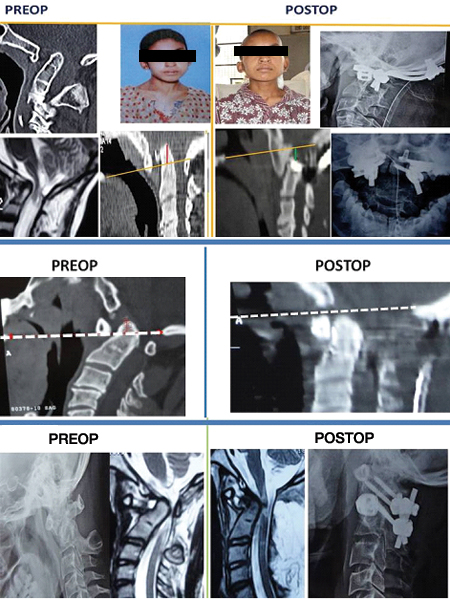
CASE 1: [Table/Fig-3] A 19-year-old female with Basilar invagination, rotatory AAD, torticollis, Occipitalised CI, Chiari 1 malformation with syringomyelia. She underwent bilateral Occipito C2 pedicle screw and rod fixation with placement of bilateral C1-C2 joint spacers.
Shows radiological comparison of preoperative and postoperative status. There is an evident downward migration of odontoid tip post atlanto axial joint jamming and posterior instrumentation. The spinal canal stenosis has been relieved as seen in the postoperative MRI. Postoperative resolution of torticollis is noted when compared to the preoperative photograph
CASE 2: A 6-year-old male child who had AAD, Os Odontoideum and torticollis. He underwent bilateral Occipito- C2 pedicle screw fixation.
CASE 3: An 11-year-old female with Os Odontoideum and reducible AAD. She underwent bilateral C1 lateral mass screws, bilateral C2 pedicle screws and rod fixation.
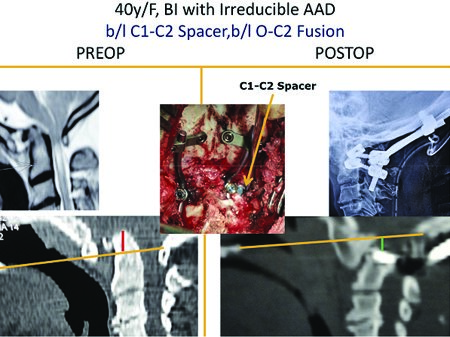
CASE 4: [Table/Fig-4] A-40-year-old female with irreducible AAD and Basilar invagination. She underwent bilateral C1-C2 joint distraction, placement of bilateral C1-C2 joint spacers and fixation using bilateral C2 pedicle screws, rods and occipital plate and screws.
Shows Occipito C2 instrumentation with joint jamming using spacers in the C1-C2 joints. The odontoid tip is seen migrated downwards postoperatively
CASE 5: A 19-year-old female with short stature, very short neck, Cervicodorsal scoliosis, fused vertebrae, hand atrophy on one side (right), basilar invagination, CV Junction severe compression and myelopathy. She underwent foramen magnum decompression, excision of C1 posterior arch, bilateral Occipito- C2 pedicle screws and rod fixation with placement of spacer in the right C1-C2 joint. Left C1-C2 joint was already fused.
CASE 6: A 62-year-old female, a known case on Rheumatoid Arthritis on irregular treatment, had reducible AAD, poor respiratory reserve. She underwent Bilateral Occipital, right C1 lateral mass and bilateral C2 pedicle screw and rod fixation with placement of bone graft within C1-C2 joints.
CASE 7: A 55-year-old male with Basilar invagination, irreducible AAD, poor respiratory reserve and severe canal compromise. He underwent bilateral Occipito-C2 pedicle screw and rod fixation with placement of bilateral C1-C2 joint spacers. He had a stormy postop course and slow recovery over 1 month.
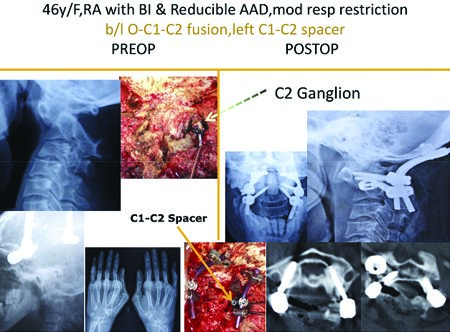
CASE 8: [Table/Fig-5] A 46-year-old female, a known case of Rheumatoid arthritis, had Basilar invagination, irreducible AAD and moderate respiratory restriction. She underwent bilateral C1-C2 joint distraction, placement of spacer within left C1-C2 joint and fixation using bilateral Occiput, C1 lateral mass and C2 pedicle screw and rods. Right C1-C2 joint was eroded due to which it had to be filled with bone graft.
Showing intraoperative photos of the C2 ganglion and instrumentation using the screw rod construct and spacers. Also shown is the radiological depiction of the rod screw construct and the C1-C2 joint spacers resulting in CV junction realignment
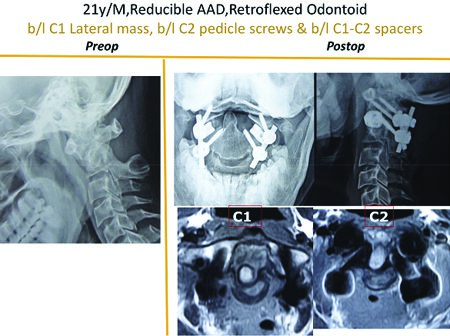
CASE 9: [Table/Fig-6] A 21-year-male presented with reducible AAD, retroflexed odontoid and compressive myelopathy. He underwent bilateral C1 lateral mass, bilateral C2 pedicle screw and rod fixation with placement of spacers in the C1-C2 joints.
Shows CVJ realignment as demonstrated in the postoperative imaging compared to the preoperative image following placement of C1-C2 screw rod construct and joint spacers
Wound complications in the form of Occipital pressure sores were seen in four patients. There were however no implant infections requiring re-exploration or implant removal. In one patient the tip of the occipital end of the rod was poking the overlying scalp. All these pressure related complications could be explained due to postop C2 hypoesthesia. We have been wiser in our last five patients who were nursed strictly in lateral position postoperatively which avoids pressure on the occipital scalp. As the occipital end of Philadelphia collar itself can itself lead to pressure sore, changing over from Philadelphia collar to a simple hard cervical collaralong with early postoperative mobilization have ensured no wound complications in our last five patients. All patients were found to have good bony fusion at followup (6-24 months) imaging. There were no delayed implant related complications.
Discussion
Surgical techniques for stabilizing the CV junction have seen major overhaul over the last two decades. Fixation techniques using Stainless steel rod, sublaminal wires and rib grafts have given way to rod and screw constructs. Occipito cervical fusion using occipital screws, C1 lateral mass screws and C2 pedicle screws is a well established surgical technique. Biomechanical studies have proven the superiority of screw rod constructs over the older systems [8]. C1-C2 transarticular screws as a stand alone procedure have been found to be biomechanically less sturdy that a screwrod construct [9]. Reinforcing it with C1-C2 sublaminar wiring and bone bicortical bone graft may not always be possible if there is severe stenosis at C1 level warranting C1 posterior arch excision. Transarticular screws have an inherent risk of Vertebral artery injury in 2.6% and 4.1% of cases due to abnormal Vertebral A anatomy [10]. C2 pedicle screws have twice the pullout strength of C2 pars screws after cyclical loading [11]. However, this procedure needs careful evaluation of the course and location of vertebral artery, as a high riding vertebral artery is prone to get injured [12]. One needs to accurately measure the length of screw that can be used as the tip of C2 pars screw points towards the vertebral artery foramen. C1-C2 joint distraction can virtually reduce any irreducible AAD [13], except obviously those in which the C1-C2 have fused anteriorly. The rationale behind C1-C2 joint distraction and placement of bone graft or bone graft filled spacer is that, the lax ligaments holding the CVJ bones become taut and provide instant stability. The spacers act as a fulcrum over which compression and extension is provided, which then corrects the AAD. Since the procedure involves movements of distraction, compression, and extension, it can be termed as Distraction, Compression, and Extensive Reduction (DCER) technique [13]. This also facilitates global 360o fusion. Preoperative and intraoperative traction provides some degree of alignment and stability for the spine during shifting, intubation and positioning and also helps in loosening the ligaments wherein the manipulation during surgery becomes easier and more bloodless. Use of muscle relaxants is better avoided as protective neck muscle tone is crucial in preventing overmanipulation and protecting the already compromised spinal cord during intubation and positioning [14]. Radiological grade of severity of myelomalacia can predict the postoperative outcome [15].The fusion rate for rigid implant fixation of CV Junction has been excellent (90-100 %).
Conclusion
Occipito - C2 pedicle screw/ Occipito - C1 lateral mass – C2 pedicle screw and rods/ C1 lateral mass- C2 pedicle screw and rods with opening of C1-C2 joints with elective C2 ganglionectomy and placement of bone graft/ spiked spacer filled with bone graft is the most ideal, safe, effective and biomechanically sound operative technique in the management of CV Junction instability due to AAD and Basilar invagination. This is applicable across all age groups and all aetiopathological conditions.