Septicemia means a severe form of infection in which bacteria multiply and release toxin into the blood stream. Neonatal septicemia is a clinical syndrome occurring in the first 30 days of life characterized by symptomatic systemic illness due to infectious agents [1]. Septicemia arises from various infections, including those of the skin, lungs, abdomen, and urinary tract [2].
Septicemia in newborns remains a significant cause of morality in developing countries. The fulminant nature of neonatal septicemia and its high mortality rate has always posed a challenge to the skill of a paediatrician. In general, 2% of infants are infected during intra uterine life and 10% during delivery. However, inflammatory lesions were found in about 25% newborn autopsies [1]. Previous studies on neonatal septicemia in south India [3] revealed that neonatal septicemia has contributed for the infant mortality (14.40%).
The newborn infants host resistant mechanism particularly that of preterm infant may be immature and easily overcome by invading organisms. Infection therefore becomes fulminant and causes death within few hours or days. A variety of organisms including bacteria, viruses, fungi and protozoa are the etiological agents. Etiological agents vary in different geographical area [4].
In this study we adopted, Acridine orange which is a fluorochrome stain, particularly for the demonstration of bacteria in blood and binding with the nucleic acid occurs in both living and dead bacteria, also other microorganisms [5]. Bacterial and yeast cells will appear as brilliant orange against a black, light green or yellow background [6]. CRP is an acute phase protein produced by the liver and its interaction with the complement system, in response to inflammation, infection and tissue injury [7]. CRP is useful in detecting the early infection of neonatal septicemia/meningitis and urinary tract infection by using semiquantitative latex-agglutination as a rapid screening method [8]. This CRP test is highly sensitive, but when compared with Buffy coat smear examination, it is easy, cheep, time saving, rapid and also can be performed in remote centers, where there is a no well equipped laboratory available [9].
This study was undertaken to compare and evaluate the gram stain, acridine orange stain and CRP results with blood culture reports and with each other so as to provide a feasible method to diagnose neonatal septicemia even at primary health centre level. Antibiotic susceptibility of various pathogenic bacteria isolated in neo-natal septicemia were also tested.
Materials and Methods
Samples were taken from neonates admitted in the sick neonatal ward at Government Rajaji Hospital, attached to Madurai Medical College, Madurai, India, and study was carried out during December - 2013 to September -2014.
Sample Collection and Selection Criteria of Neonates
Blood Samples was taken from 70 clinically suspected cases of neonatal septicemia. Babies suffering from septicemia selected for this study had one or the other following symptoms described below: refusal of feeds, lethargy, diarrhea, vomiting, poor cry, abdominal distention, fever, respiratory distress, convulsion, hepatomegaly, jaundice, sclerema, boils, umbilical sepsis etc., and exclusion criteria as listed below: Patients with spina bifida, Anencephaly, other neural tube defects and in very sick neonates, after initial stabilization.
C - reactive protein (CRP) Test
CRP was estimated by using standard kit marketed by TULIP Diagnostic P.Ltd., Goa. There are two types of slide methods namely: (1) Qualitative method, (2) Semi quantitative method [10].
(1) Qualitative Method
One drop serum was placed on the glass slide and added one drop of Rhelax CRP latex reagent to the test specimen on the slide. Using a mixing stick, the serum and Rhelax CRP latex reagent was mixed uniformly over the entire circle. The slide was rocked gently back and forth, observing for agglutination macroscopically after two minutes.
(2) Semi Quantitative Method
Using isotonic saline, serial doubling dilutions of the serum sample was prepared as follows: 1:2, 1:4, 1:8, 1:16, 1:32, and 1:64. Each dilution of the serum sample was pipetted into separate reaction circles. The same procedure as under qualitative method was continued for each dilution.
Buffy Coat Smear Examination
One ml of blood was transferred into sterile wintrobe tube and centrifuged at 2500 rpm for 30 minutes. The plasma was removed and buffycoat was taken for smear preparation [11]. One smear was stained by Gram’s technique and other one was stained by Acridine orange. The smears were fixed by methanol.
Gram’s staining
The fixed smear were flooded with crystal violet stain for minute and washed with water. The gram’s iodine was added and allowed for one minute. After that acetone was added for not more than five seconds and washed with water. Then dilute carbol fuchsin was added and allowed for one minute and washed with water. Finally the smear was air dried and the slide was examined under oil immersion microscope. The gram positive organisms appeared violet in colour and the gram negative organisms pink in colour.
Acridine orange staining
According to Brain Lauer et al., [12], the buffy coat smear was air dried and fixed by methanol. The fixed smears were flooded with acridine orange stain and left for five minutes followed by washing with water. The acridine orange stained smears were examined with incident light fluorescence at 600X magnification and confirmed at 1500X magnification. The bacteria appeared orange or orange red in colour [13].
Blood Culture Methods
Blood collected aseptically was transferred to a culture bottle containing brain heart infusion broth. The culture bottle was incubated at 37°c for 18 to 24 hours, after which sub culturing on the following plates were done using sterile technique. (a) Nutrient agar plate; (b) Blood agar plate; (c) Mac conkey agar plate. Plates were incubated at 37°c for 18 to 24 hours aerobically and growth in the plates observed. The colony size, shape, edge, margin, consistency were noted. Broth was examined for any turbidity, pellicle formation and deposit. The colonies were identified by following techniques; (1) Gram stain-to identify gram positive and gram negative organism. (2) Hanging drop- to find out motile and non motile organism. (3) Oxidase, catalase test- to rule out Enterobacteriaceae. (4) Coagulase test to identify Staphylococcus aureus and Coagulase negative staphylococci. Member of species was identified by bio chemical reactions using sugar fermentation, Indole, methyl red, voges proskauer, citrate, and urease and hydrogen sulphide production.
Kirby Bauer- disc diffusion technique
After isolation of the organism antimicrobial sensitivity test was done to select the antimicrobial drugs. Disc diffusion technique was used to identify the zone inhibition of bacterial strains [14]. In this study we used ampicillin, Gentamycin, co-trimoxazole, cefatoxime and amikacin for all isolates and in addition cloxacillin for gram positive agents.
Results
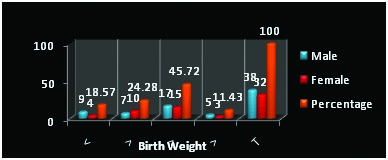
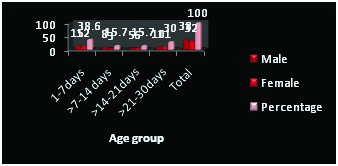
In the present study 70 cases of neonatal septicemia were taken. There were 38 males (54.29%) and 32 females (45.71%) percentage respectively. So it is inferred that males are more affected by septicemia than females. The breakup details in relation to sex, birth weight and age are given in [Table/Fig-1,2] respectively. From [Table/Fig-3], it could be inferred that out of 70 cases studied for septicemia, most of the infants 62 (88.57%) belonged to lower birth weight of less than 2.5 kg. The clinical symptoms and signs of these 70 neonates with septicemia are furnished in the [Table/Fig-3].
Birth weight of the neonates in relation to sex
Age and sex distribution in 70 neonates
Clinical features of neonates with septicemia
| Clinical Features | Numbers* | Percentage |
|---|
| Gastro intestinal tract symptoms |
| Refusal of feeds | 50 | 71.42 |
| Vomiting | 12 | 17.4 |
| Diarrhoea | 8 | 11.42 |
| Abdominal distension | 9 | 12.85 |
| Hepatomegaly | 42 | 60 |
| Jaundice | 8 | 11.42 |
| Upper respiratory tract symptoms |
| Respiratory distress | 34 | 48.57 |
| Central nervous system symptoms |
| Lethargy | 33 | 47.14 |
| Poor cry | 32 | 47.71 |
| Convulsion | 4 | 5.71 |
| Other manifestations |
| Fever | 13 | 18.57 |
| Skin manifestation | 1 | 1.43 |
* Many newborn had more than one manifestation
From 41 samples one or other bacteria was isolated. It was inferred that among the organisms isolated Klebsiella pneumonia ranked first accounting for 68.29% followed by Escherichia coli and Coagulase negative staphylococcus (9.75% each). The antimicrobial sensitivity was furnished in [Table/Fig-4].
Results of antimicrobial sensitivity of the organisms isolated
| Drugs | Klebsiella pneumoniae | Escherichia coli | Proteus | Pseudomonas aeruginosa | Coagulase -ve staphylococcus |
|---|
| S | R | S | R | S | R | S | R | S | R |
|---|
| Ampicillin | 12 | 16 | 3 | 1 | 1 | 1 | 1 | 2 | 1 | 3 |
| 42.90% | 57.10% | 75% | 25% | 50% | 50% | 33.30% | 66.70% | 25% | 75% |
| Gentamycin | 21 | 7 | 3 | 1 | 2 | 0 | 2 | 1 | 2 | 2 |
| 75% | 25% | 75% | 35% | 100% | — | 66.70% | 33.30% | 50% | 50% |
| Cefatoxime | 26 | 2 | 3 | 1 | 2 | 0 | 2 | 1 | 4 | 0 |
| 92.90% | 7.10% | 75% | 25% | 100% | — | 66.70% | 33.30% | 100% | — |
| Amikacin | 28 | 0 | 4 | 0 | 2 | 0 | 3 | 0 | 4 | 0 |
| 100% | — | 100% | — | 100% | — | 100% | — | 100% | — |
| Cotrimoxazole | 15 | 13 | 2 | 2 | 1 | 1 | 1 | 2 | 0 | 4 |
| 53.60% | 46.40% | 50% | 50% | 50% | 50% | 33.30% | 66.70% | — | 100% |
| Cloxacilin | — | — | — | — | — | — | — | 4 | 0 | — |
| | | | | | | 100% | — | |
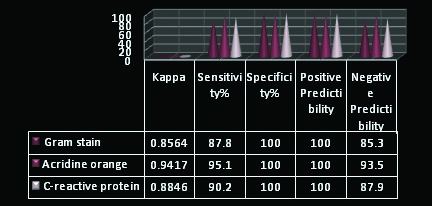
Isolation of microbes is the gold standard test in patients with septicemia. In this study, the gram stain, acridine orange stain and CRP results were compared with blood culture reports and with each other. It was found that 37 culture positive cases had elevated CRP, 36 culture positive cases had positive response to gram staining, 39 of the 41 culture positive cases were also positive for acridine orange. The details are provided in the [Table/Fig-5]. The sensitivity and specificity of the staining technique and CRP in comparison with blood culture was analyzed statistically (correlation) and results were presented in [Table/Fig-6]. Positive and Negative predictability studies to find the association between blood culture and staining as well as CRP did not reveal any superiority of these staining or serology over blood culture.
Results of blood culture, serum C-reactive protein and buffy coat smear by gram stain and acridine orange stain
| Investigation | Clinical Septicemia Neonates |
|---|
| Positive (%) | Negative (%) |
|---|
| Blood culture | 41(58.57) | 29(41.42) |
| Serum CRP | 37(52.85) | 33(47.14) |
| B.C.S.Gram stain | 36(51.42) | 34(48.57) |
| B.C.S. acridine orange stain | 39(55.71) | 31(44.28) |
Note- B. C.S- Buffy Coat Smear.
Result of statistical analysis
Discussion
In this study bacteriological agents were isolated from 41 of the 70 patients. Gram negative bacteria were isolated in 37 (90.24%). Among them Pseudomonas aeruginosa was isolated in 3 (7.31%), Proteus genus in 2 (4.88%), Escherichia coli in 4 (9.76%) and Klebsiella in 28 (68.29%), gram positive organism was isolated in another 4 (9.76%) cases and it was Coagulase negative staphylococcus. Thus in this study 90.24% of neonates were affected by gram negative organisms and 9.76% by gram positive organisms. This report is supported by the study of Vaidya et al., [15].
Klebsiella was the predominant organism (68.29%) in this study, which also correlates with the study of Bhutta et al., [16] and Daoud et al., [17] in whose studies Klebsiella was the commonest etiological agent for the neonatal septicemia. Sanghvi and Tvdehope [18] reported that Group B streptococcus contributed to 52% of septicemia in developed countries, but in this study there was no isolation of Group B streptococcus.
In this study, the gram negative organisms like Klebsiella pneumoniae, Escherichia coli, Proteus mirabilis, and Pseudomonas aeruginosa were highly sensitive to cefatoxime and amikacin. Gentamycin was moderately sensitive to both gram positive and gram negative organism. Coagulase negative staphylococcus isolated in this study was sensitive to amikacin, gentamycin and cloxacillin. Gupta et al., [19] also reported coagulase negative staphylococcus was sensitive to amikacin. This finding also coexist with the study of Vaidya et al., [15] who described that the gram negative organisms were highly sensitive to cefatoxime and moderately sensitive to gentamycin and kanamycin.
Jha et al., [20] studied the out of 150 cases of childhood septicemia of age group 0-14 years, 83 had positive (CRP >6ìg/ml), 70 were positive for BBCS and blood culture was positive only in 83 cases, where predominant organism being Klebsiella species followed by Staphylococcus species. CRP test showed 100.0% sensitivity and 87.30% specificity, where BBCS showed 76.5% sensitivity and 91.2% specificity. This study also related to our finding.
Rajendra et al., [21] studied the 200 cases, from that 95 (47.5%) were blood culture positive. Gram negative isolates were 70.53% and Gram positive 29.47%. Buffy coat had specificity of 86.1% and sensitivity of 55.3%. CRP test had 87.37% sensitivity and 71.43% specificity. Usefulness of buffy coat smear, Gram positive and Gram negative isolates, during present study is also identical. In this study, Buffy coat had specificity of 100% and sensitivity of 87.8%.
In this present study, showing the Sensitivity and specificity and positive predictive valve of CRP are 90.2% 100% and 100% respectively. The report was coincided to the Sucilathangam et al., [22] which is 50%, 69% and 38.8% respectively.
Kumar [23] studied 22 cases were bacteriologically positive. Most common isolated organism was Escherichia coli followed by Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, Proteus mirabilis, Group B Streptococcus and Streptococcus fecalis. This study endorsed by the present work and common organisms isolated was Klebsiella species followed by Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis and Coagulase negative Staphylococcus.
In this study, we inferred that out of 70 cases Studied for septicemia, most of the infants 62 (88.57%) belonged to lower birth weight of less than 2.5 kg. The clinical presentation of sepsis, 41% cases were blood culture positive and 29% cases were blood culture negative. This finding correlated with the findings of Desai et al., [24] studies, Out of 60 total cases of proven neonatal sepsis was higher in low birth weight (≤2500 gms) infants (65%). Amongst 100 neonates with clinical presentation of neonatal sepsis, 52% cases were blood culture positive and 28% cases were blood culture negative.
Conclusion
In this present study, male neonates (54.29%) were more affected than female neonates (45.71%). Accordingly, we conclude that serum CRP and Buffy Coat Smear Examination is simple method for diagnosis of childhood septicemia. These tests are also helpful to rule out child infection and their treatment can be started by clinician as soon as possible within one hour, which is not only in tertiary care centers but also in remote area primary health care centers, unlike conventional methods that take upto seven days for blood culture for diagnosis of infection and septicemia. The isolated organisms were found to be highly sensitive to cefatoxime and amikacin. Hence, these antibiotics can be considered as the first drug of choice for neonatal septicemia.
* Many newborn had more than one manifestation
Note- B. C.S- Buffy Coat Smear.