Prompt Diagnosis and Management of Cervical Necrotizing Fascitis
Shivakshi Chansoria1, Harsh Chansoria2, P.V. Wanjari3, Sumeet Jain4, Pushkar Gupta5
1 Senior Lecturer, Department of Oral Medicine Diagnosis & Radiology, Index Institute of Dental Sciences, Indore, Madhya Pradesh, India.
2 Lecturer, Department of Prosthodontics, Government College of Dentistry, Indore, Madhya Pradesh, India.
3 Professor and Head, Department of Oral Medicine Diagnosis & Radiology, Modern Dental College and Research Centre, Indore, Madhya Pradesh, India.
4 Professor, Department of Prosthodontics, Sri Aurobindo College of Dentistry, Indore, Madhya Pradesh, India.
5 Reader, Department of Prosthodontics, Hitkarini Dental College & Hospitals, Jabalpur, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shivakshi Chansoria, G-101, Orchid,Ocean Park, Near Delhi Public School, Nipania, Indore-452016, Madhya Pradesh, India. E-mail : shivakshi17@gmail.com
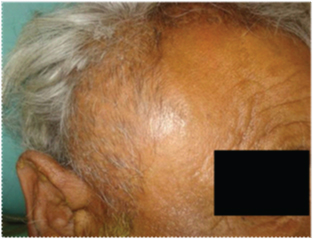
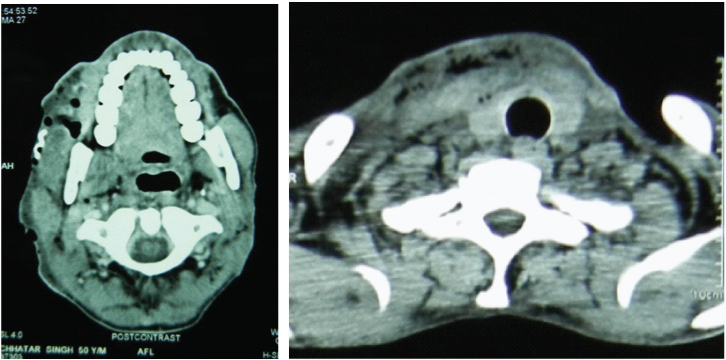
Necrotizing fasciitis is a rapidly progressing inflammatory infection of the fascia, with secondary necrosis of the subcutaneous tissue. It is uncommon and difficult to diagnose, and it causes progressive morbidity until the infectious process is diagnosed and treated medically and surgically [1]. Smith et al., stated that the mortality rate of necrotizing fasciitis can be upto 34%. Monomicrobial necrotizing fasciitis is caused by the betahemolytic streptococcus normally seen in healthy persons with the previous history of wound infection [2]. Necrotizing fasciitis is also known as Flesh eating disease, Gangrenous erysipelas, Hospital gangrene, Non-closteroidal crepitant cellulitis, Streptococcal gangrene, Meleney’s cellulitis [3]. A 50-year-old male was admitted with history of pain and swelling of cervical and temporal region since four days. The patient presented with cervical and temporal abscess upon physical examination [Table/Fig-1]. The overlying skin showed multiple haemorrhagic areas [Table/Fig-2] varying in size from 2 cm to 4 cm. Computerized Tomography (CT scan) of the head and neck region [Table/Fig-3] showed collection of air in the pretracheal, retrotracheal regions. A diagnosis of cervical necotizing fasciitis along with temporal abscess secondary to grossly decayed 48 was made. The following differential diagnoses were considered, Necrotizing fasciitis, Ludwig’s angina, Erysipelas, Progressive bacterial gangrene. Microbiolgical analysis of the pus revealed staphylococcus aureus. Intravenous antibiotic therapy consisted of Injection cefotaxime with salbactum (1.5 gm eight hourly) and Injection levofloxacin 100 ml 24 hourly. Incision and drainage of the cervical and temporal abscess was done followed by vigorous debridement of fascia, subcutaneous tissue and necrotic skin [Table/Fig-4]. Neomycin and cutacill dressing was done [Table/Fig-5]. Reconstruction was done after three weeks using split thickness graft from the thigh region [Table/Fig-6,7].
Swelling of cervical region with multiple haemorrhagic areas

Swelling of the temporal region,
CT scan showing air spaces
Debridement of fascia & subcutaneous tissue

Neomycin and cutacill dressing

Healing after three weeks

Healing one month after the graft placement

[1]. Gonlugur Ugur, Guclu Oguz, Karatag Ozan, Mirici Arzu, Derekoy Sefa, Cervical necrotizing fasciitis associated with descending necrotizing mediastinitisMultidisciplinary Respiratory Medicine 2011 6(6):387-89. [Google Scholar]
[2]. Smith Necrotizing fasciitis following saphenofemoral junction ligation with long saphenous vein stripping: a case reportJournal of Medical Case Reports 2010 4:161 [Google Scholar]
[3]. Richard Edlich F, Necrotizing fasciitis. Medscape drug, disease and procedure reference 2014References 2010 17(1):121-23. [Google Scholar]