Ameloblastomatous Calcifying Cystic Odontogenic Tumour: A Rare Variant
Rama Raju Devaraju1, Lakshmi Srujana Duggi2, Ramlal Gantala3, Shylaja Sanjeevareddygari4, Abhinand Potturi5
1 Professor ad HOD, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Mahabubnagar, Telangana, India.
2 Post Graduate Student, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Mahabubnagar, Telangana, India.
3 Associate Professor, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Mahabubnagar, Telangana, India.
4 Professor, Department of Oral and Maxillo Facial Pathology, SVS Institute of Dental Sciences, Mahabubnagar, Telangana, India.
5 Reader, Department of Oral and Maxillo Facial Surgery, SVS Institute of Dental Sciences, Mahabubnagar, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramlal Gantala, Associate Professor, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Appanapally, Mahabubnagar, Telangana, 509002, India. E-mail : dr_ramlal@yahoo.com
Calcifying Cystic Odontogenic Tumor (CCOT) was previously described by Gorlin et al., in 1962 as Calcifying odontogenic cyst. CCOT is a rare lesion which accounts for 2% of all odontogenic pathological changes in the jaws. One of the variants, Ameloblastomatous proliferating type of CCOT is even more rare and very few cases have been reported in the light of literature review. This case report is an effort to bring forth a case of ameloblastomatous proliferating type of CCOT in a 65 year male, who presented with a painful swelling in the right jaw crossing midline causing facial asymmetry and confirmed by histopathological evaluation.
Ameloblastomatous proliferations, Calcifying odontogenic cyst, Ghost cells, Odontogenic tumours
Case Report
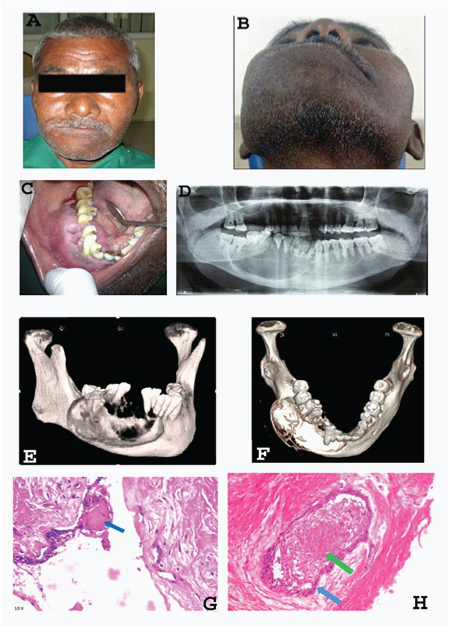
A 65-year-old male presented with a swelling in the right lower jaw since four months. History revealed a slow progressive, painful swelling associated with watery discharge on chewing hard foods. Extra orally, gross asymmetry was detected [Table/Fig-1A-B]. Intra oral examination revealed well defined, tender, soft, fluctuant swelling extending from 32-47, obliterating right buccal, lingual and labial vestibules [Table/Fig-1C]. Grade II & III mobility noticed with 31,32 and 41-46 respectively. Provisional diagnosis of Ameloblastoma was given. Differential diagnosis of CCOT, central giant cell granuloma and calcifying epithelial odontogenic tumour were considered. OPG revealed well defined radiolucency from 32-47 region with mixed internal appearance [Table/Fig-1D]. CT, 3D CT revealed hypodense area extending from 32-47 region [Table/Fig-1E-F]. Microscopically, cystic lumen lined by stratified squamous epithelium with basal ameloblast like cells and superficial stellate reticulum-like tissue intermixed with few ghost cells. At focal areas epithelium also exhibits intramural proliferations. Within the connective tissue, few ameloblastomatous islands with peripheral flattened to tall columnar cells having hyperchromatic nuclei placed away from basement membrane and central stellate reticulum like tissue and focal areas of squamous metaplasia are also evident. Connective tissue also exhibits focal areas of hyalinization. Final diagnosis of, “Calcifying cystic odontogenic tumour type 3” was given [Table/Fig-1G-H]. Patient was chalked out for surgical enucleation under general anesthesia but the patient showed reluctance towards the treatment.
A,B. Extra oral photographs showing swelling causing facial asymmetry in the right mandible; C.Intra oral photograph showing indentations of the opposing teeth over the swelling with supra eruption of 44 and 45. D. Radiolucent lesion with displacement and divergence of roots with 44-45.Root resorption with 32,41-46. E,F. Reconstructed 3D views showing a large, expansile lesion with lysis of right buccal & lingual cortices. G. H & E section (10 x) showing ghost cell with in the odontogenic epithelial component (blue arrow). H. H & E section (10 x) showing ameloblastomatous island (blue arrow) with central areas of squamous metaplasia (green arrow) surrounded by delicate to dense connective tissue
Discussion
Early literature states that, Gorlin et al., considered CCOT as a separate histopathological entity, owing to the presence of “ghost cells” [1]. Since its first description controversy and confusion have prevailed regarding its nature which propelled various taxonomical classifications and nomenclatures [2]. After many break throughs in the presentation and behaviour of Calcifying odontogenic cyst, finally it secured a place in the group of Odontogenic tumours. In 2005, WHO proposed a Histological classification of Odontogenic tumours in which Calcifying odontogenic cyst was renamed as “Calcifying cystic odontogenic tumor” (CCOT) by Ledesma-Montes [3] due to its neoplastic behavior [Table/Fig-2].
Classification of the Ghost cell odontogenic tumours [3]
| Calcifying cystic odontogenic tumour (CCOT), includes peripheral and central cases CCOT type 1. Simple cystic CCOT. Includes pigmented and clear cell variants CCOT type 2. Odontoma-associated CCOT CCOT type 3. Ameloblastomatous proliferating CCOT CCOT type 4. CCOT associated with benign odontogenic tumours other than odontoma |
| Dentinogenic ghost cell tumour (DGCT) DGCT type 1. Central, solid, aggressive variant DGCT type 2. Peripheral, less aggressive variant |
| Ghost cell odontogenic carcinoma (GCOC). Three pathogenic mechanisms 1. GCOC arising ‘de novo’. Not associated with a previous DGCT or CCOT, but with areas suggesting DGCT 2. GCOC ex-CCOT. GCOC arising from a previous CCOT 3. GCOC ex-DGCT. GCOC arising from a previous DGCT |
Hong et al., reported 92 cases of CCOT, of which only 11 were ameloblastomatous type [4]. To the best of our knowledge, only 30 ameloblastomatous CCOT cases are reported in the literature. Of which 12 cases presented as painless swellings, two cases presented without any symptom, information is not available for 14 cases [5] and only 2 cases reported by Kamboj and Manish [5,6] and Abikshyeet et al., [4] presented as painful swellings similar to present case. According to the available literature on ameloblastomatous CCOTs, it occurs only intraosseously [7] over a wide age range from 11 to 63 yrs, with a slight female predilection [5]. Premolar molar region of the mandible is the most commonly affected site, but a case reported by Kamboj and Manish [6] showed the involvement of ramus extending upto the condyle and coronoid process [6]. In present case, the lesion is involving right mandible crossing the midline, similar presentation was noticed in the cases reported by Yuwanati et al., [5] and Abikshyeet et al., [4].
Radiographically, initially it appears as a unilocular radiolucency and in later stages a mixed radiolucent-radioopaque appearance can be seen referred as “salt and pepper type of pattern” [8]. Root resorption is the most important radiographic feature [7] which is also noticed in the present case.
Definitive diagnosis of the present case is made based on histopathological features like cystic lumen lined by basal ameloblast-like cells, superficial stellate reticulum like tissue associated with ghost cells and focal intramural ameloblastomatous proliferations. Histopathologically, Ameloblastomatous CCOT shares common features with unicystic ameloblastoma except for the ghost cells and calcifications. Ameloblastoma ex CCOT represents an ameloblastoma arising from the cystic lining epithelium of CCOT. Ameloblastomatous CCOT can be differentiated from ameloblastoma ex CCOT by lack of histopathologic criteria suggested by Vickers and Gorlin. According to Yoshida et al., immunohistochemical studies suggested greater mean Ki-67-LI in ameloblastomatous CCOTs than in those without these histological features, representing a high proliferation potential associated with ameloblastomatous proliferation. Out of seven cases of ameloblastomatous CCOT, six cases (86%) showed expression of Bcl-2 protein [9]. Conservative surgical enucleation is the treatment of choice [5] as prognosis is good with no recurrence, indicating non neoplastic nature of the lesion [2]. Of all the reported cases only one case reported by Yuwanati et al., showed recurrence after six yrs [5].
Conclusion
The present case represents the classic features of ameloblastomatous CCOT, which comes under the category of CCOT type 3 (according to Ledesma Montes et al.,) which is a very rare odontogenic lesion. Such cases highlight the varied presentation of CCOT and throws light towards its behaviour.
[1]. Archana S, Sabane V S, Rajeev D, Calcifying Ghost Cell Odontogenic Cyst: Report of a Case and Review of LiteratureCase Rep Dent 2011 10:1-5. [Google Scholar]
[2]. Samuel S, Sreelatha S V, Venkatesh S, Nair Preeti P, Ameloblastomatous calcifying odontogenic cyst: a rare histological variantBMJ Case Rep 2013 doi:10.1136/bcr-2013-009137 [Google Scholar]
[3]. Ledesma-Montes C, Gorlin R J, Shear M, Praetorius F, Mosqueda-Taylor A, Altini M, International collaborative study on ghost cell odontogenic tumours: Calcifying cystic odontogenic tumour, dentinogenic ghost cell tumour and ghost cell odontogenic carcinomaJ Oral Pathol Med 2007 37:302-08. [Google Scholar]
[4]. Abikshyeet P, Venkatapathy R, Balamurali PD, Dhanuja M, Calcifying Odontogenic Cyst Associated with AmeloblastomaIndian J Stomatol 2012 3(4):275-77. [Google Scholar]
[5]. Yuwanati MB, Jagdish Vishnu T, Shubhanghi M, Avadhani A, Pradnya J, Ameloblastomatous calcifying ghost cell odontogenic tumor: A case reportIJCRI 2012 3(9):21-25. [Google Scholar]
[6]. Kamboj M, Manish J, Ameloblastomatous Gorlin’s cystJ Oral Sci 2007 49(4):319-23. [Google Scholar]
[7]. Harkanwal PS, Madhulika Y, Sandeep KB, Ameloblastomatous calcifying ghost cell odontogenic cyst - a rare variant of a rare entityAnn Stomatol (Roma) 2013 4(1):156-60. [Google Scholar]
[8]. Regezi Joseph A, Sciubba James J, Jordan Richard CK, Cysts of the jaws and neckOral Pathology Clinical Pathologic Correlation 2008 5th ednChinaElsevier:249-50. [Google Scholar]
[9]. Yoshida M, Hiroyuki K, Kiyoshi O, Hideaki M, Histopathological and immunohistochemical analysis of calcifying odontogenic cystsJ Oral Pathol Med 2001 30:582-88. [Google Scholar]