It is a well-known fact that the extraction of teeth results in significant dimensional changes in the jaw bone. The rate of change and the magnitude of these changes have been widely studied, both in various human and in animal studies [1].
Bone is a dynamic organ that can regenerate and bone grafting is a dynamic phenomenon. The two types of bone grafts frequently used in are autografts and allografts. Autograft bone is transplanted from another part of the recipient’s body. Autologous bone remains the gold standard, but requires a second surgical site that can result in additional pain and complications, is limited in quantity and increases the cost of the procedure. The bone grafted from genetically non identical members of the same species is known as Allograft bone. Its advantage is that it obviates the morbidity with donor-site complications and is readily available in the desired size, shape and quantity [2]. Fresh-frozen or demineralized freeze dried allograft bone has also been used, however due to rapid rate of resorption does not make it ideal for large bony defects. Recently, xenograft materials are gaining more popularity with good success rate as bone graft substitutes [1]. These grafts are procured from one individual and transplanted into another individual of a different species and are usually derived from porcine, coral, and bovine sources [3].
Three biologic processes are involved in new bone formation within a bone graft - Osteogenesis, Osteoconduction and Osteoinduction [4].
The main purpose of this present study was to radiologically assess and compare the regenerative potential of hydroxyapatite with Collagen (G-Graft) & hydroxyapatite (G-Bone) and to evaluate the clinical usefulness of these materials to enhance bone healing in third molar extraction sites through bone formation.
The hypothesis of the current study was that, the composite of hydroxyapatite & Collagen (G-Graft) may lead to earlier bone regeneration and greater density of the mature bone. The purpose of this study was to radiologicaly assess & compare the regenerative potential of Hydroxyapatite (G-Bone) & Hydroxyapatite with Collagen (G-Graft), and to evaluate the clinical usefulness of these materials to enhance bone healing in third molar extraction sites through of bone formation.
G-Graft is, made of natural low crystalline hydroxyapatite with collagen, both derived from natural sources i.e. bovine origin. It is available in form of granules, dowels and blocks. The shape can be changed by using Gigli saw and bone nibblers [5]. Calcium hydroxyapatite in highly crystalline form is used to make G-Bone modified hydroxyapatite granules and blocks. The body absorbs this form very slowly. It is derived from Bovine Bone which is sintered at +500 Celsius and this high temperature leaves only pure inorganic structure and thus removes the risk of transmission of any disease [6].
Materials and Methods
The study was carried out in the Department of Oral & Maxillofacilal Surgery within the period of ten months with effect from February to November 2011. A total of 63 patients aged 18 to 30 y (mean age of the patients was 27.33 ± 7.24 y), 45 (71.43%) males and 18 (28.57%) females, who came to the Department of Oral Surgery for the extraction of mandibular third molar were selected randomly for the study. A thorough clinical examination was done and recorded on standard proforma. Patients were advised an Intraoral periapical (IOPA) radiograph or Orthopantamogram (OPG) and laboratory investigations if needed. A preoperative assessment was carried out and recorded Impactions were classified based on WINTER’S classification of impaction. Also the amount & status of soft tissue covering of the third molars was noted. After clinical history, examination and reviewing, patients were equally divided into three groups. The rationale for assigning the patients to the groups was strictly random:
Group I – G-Graft (Hydroxyapatite with Collagen) was used as Bone graft material
Group II – Bone graft material used was G-Bone (Hydroxyapatite)
Group III—Control group (no grafts was used)
All selected patients of 3 groups were prepared by doing thorough oral prophylaxis. Patients were extensively informed about the procedures, including the uncertainties of using a new bone regenerative material. They were asked for their full cooperation during treatment and research on a voluntary basis. A signed written informed consent was taken. A formal ethical clearance to conduct this study was obtained by the ethical committee of the institute. The patient’s face was prepared with povidone- iodine and patient were draped. Patients were asked to rinse their mouth thoroughly with povidone- iodine mouth wash before any operative procedure was undertaken.
All surgeries were performed under local anaesthesia. Inferior alveolar nerve block, lingual nerve block and long buccal nerve block were administered using 1.8ml, 2% lignocaine hydrochloride with vasoconstrictor [1:80000]. All patients were operated on by the same surgeon using a standard operating technique. A horizontal incision in the gingiva was given. An envelop mucoperiosteal flap was raised, extension of which varied in each case depending upon the access required. Where indicated, number 703 straight fissure carbide bur incorporated in straight handpiece attached to physiodispenser was used to remove the bone on the buccal and distal aspect of the third molar under constant sterile 0.9% saline irrigation. Tooth elevation, crown removal and or root division were carried out as and when needed. 0.9% sterile saline was used to meticulously rinse the surgical field after removal of the tooth. Graft material was taken and packed in the extraction socket in group I (G- Graft) and II (G- Bone). The wound were closed by placing 3-0 braided silk interrupted sutures which were removed at 7th postoperative day.
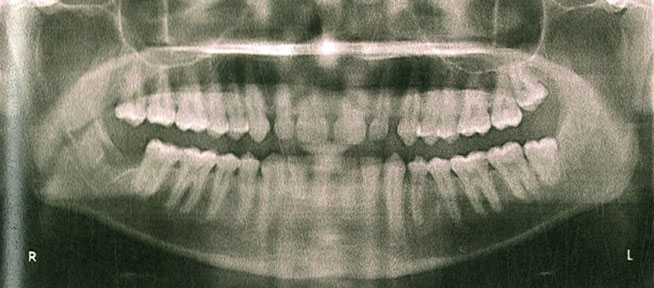
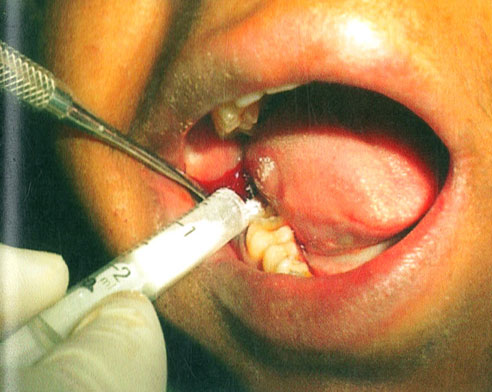
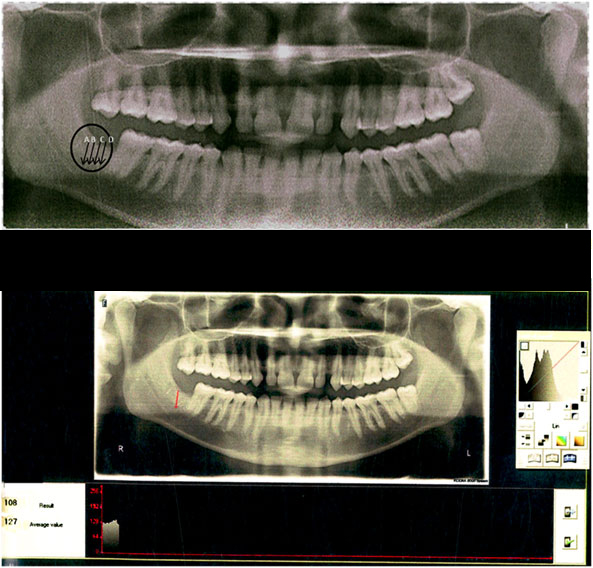
Orthopentomogram (OPG) images were taken intra-operatively, just after extraction in the Group III (control), after extraction but before graft placement [Table/Fig-1,2] in Group I & II (study groups) and postoperatively at the end of first month [Table/Fig-3] and third month [Table/Fig-4]. Bone density of the postextraction sockets was measured at four random areas where graft was placed within the extraction socket through ‘densitometric analysis’ software in the OPG program (Kodak 8000C Digital Panoramic System, Eastman Kodak Company). From the four obtained values, an average value was recorded through the software [Table/Fig-5].
Postopertaive OPG before placement of graft
Graft placement after removal of tooth


Bone density of the post-extraction sockets was measured at four random areas (A,B,C,D) through ‘densitometric analysis’ software in the OPG program (Kodak 8000C Digital Panoramic System, Eastman Kodak Company) and an average value was recorded at each review
The data were collected and entered into a Microsoft Excel Worksheet and analysed using SPSS (version 7.5) statistical package. Pearson’s correlation test(r) was applied to find the correlation between two variables.
Results
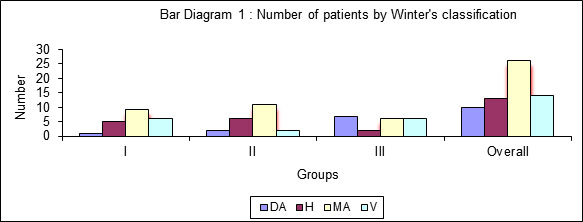
The radiographic analysis showed that most of the third molar, 41.26% (26) were mesioangualr impactions, followed by vertical 22.22% (14), horizontal 20.63% (13), and distoangular 15.87% (10) [Table/Fig-6,7].
Shows preoperative angulation of the third molars (Distribution according to Winter’s classification)
| Group | Winter’s classification |
|---|
| Distoangular (DA) | Horizontal (H) | Mesioangular (MA) | Vertical (V) | Overall |
|---|
| I(G GRAFT) | 1 | 5 | 9 | 6 | 21 |
| II(G BONE) | 2 | 6 | 11 | 2 | 21 |
| III(Control) | 7 | 2 | 6 | 6 | 21 |
| Overall | 10 | 13 | 26 | 14 | 63 |
Bar diagram showing number of patients classified as according to Winter’s classification
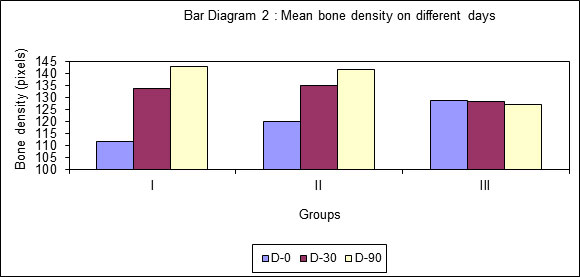
Bone density was measured by digital orthopentomogram (OPG) (in pixels), orthopentomogram (OPG) images were taken intraoperatively, just after extraction in the Group III (control), after extraction but before graft placement in Group I & II ( study groups) and postoperatively at the end of first month and third month.
The intraoperative mean measurement for group I (G Graft) was 111.57 ± 16.63 (82- 140), for group II (G Bone) was 120.23 ± 14.34 (90 – 136) and that for Group III (Control) was 128.85 ± 15.62 (103 – 165). At the end of 1st post-operative month, the mean measurement for Group I was 133.57 ± 21.55 (80 -162), for Group II, it was 135.0556 ± 13.97 (110 - 154), and for Group III, it was 128.5238 ± 16.47 (115 – 170). At the end of 3rd post-op month, the mean measurement for group I was 142.74 ± 15.32 (125 - 165), for Group II, it was 141.55 ± 11.67 (122 – 156), and for Group III, it was 127.14 ± 14.23 (107 - 162) [Table/Fig-8,9].
Mean Bone density on different days
| Group | Days |
|---|
| 0 | 30 | 90 |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| I(G GRAFT) | 111.5714±16.63001 | 133.5789±21.55436 | 142.7368±15.32551 |
| II(G BONE) | 120.2381±14.34191 | 135.0556±13.97255 | 141.5556±11.67311 |
| III (Control) | 128.8571±15.62461 | 128.5238±16.4761 | 127.1429±14.23477 |
Bar diagram showing mean bone density after extraction but before graft placement, at the end of first and third month postoperatively
The percentage increase in bone density at the end of 1st month postop was 19.22 ± 11.98 in Group I (G Graft), 12.77 ± 8.69 in Group II (G Bone), while that of Group III was found to be -0.20± 5.19.
The percentage increase in bone density at the end of 3rd month postop was, 27.73 ± 14.42 in Group I (G Graft), 17.72 ± 10.59 in Group II (G Bone), while that Group III (control) was found to be -1.14 ± 4.0569. The percentage increase in bone density between 1st month & 3rd month was 7.55± 12.43 in group I (G Graft), 4.41± 5.4859 in group II (G Bone), while that Group III (control) was found to be -0.82 ± 3.96 [Table/Fig-10]. The bone density increase was found to be statistically highly significant (p<0.01) between all groups.
Percentage increase in bone density
| Group | %increase-0-30 days | %increase-0-90 days | %increase-30-90 days |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| I(G Graft) | 19.22±11.98 | 27.73±14.42 | 7.55±12.43 |
| II(G BONE) | 12.77±8.69 | 17.72±10.59 | 4.41±5.48 |
| III(control) | -0.20±5.19 | -1.14±4.05 | -0.82±3.96 |
Discussion
Osteogenetic cells to facilitate bone reconstruction, osteoinductive factors to induce bone formation and an osteoconductive matrix to stimulate bone deposition are the prime components for ideal bone graft substitute. Osteoconductive materials although have no potiential to induce bone formation but they act as an interconnected biocompatible scaffold, which local osseous tissue can employ for the regeneration of living bone. Whereas osteoinductive materials promote new bone formation by allowing cells in the adjoining area to undergo phenotypic transformation to osteoprogenitor cell types that are capable of bone formation and osteogenic is a graft material that has the inherent capacity to form bone, which reveals that it has cells such as osteoblasts or osteocytes which makes it capable of producing new bone [7].
There have been various studies carried out in the recent past to evaluate the bone density at the grafted site which shows the acceptance of the graft by the host. Standard radiography is the most common imaging method used to assess bone healing [8,9] because it is widely available, cheap, and relatively safe. However, that assessment of bone healing by radiography is a subjective method, thus the chances of error are more [10].
Therefore, other imaging technologies and methods are being investigated that help quantify bone healing, which include dual energy X-ray absorptiometry, single energy X-ray absorptiometry, radiographic absorptometry, ultrasound and quantitative computed tomography. But, these techniques are costly and have radiation hazards except ultrasound [11].
In our study we used the Densitometric Analysis software for the assessment of bone healing by densitometric comparisons between digital orthopantogram (OPG) taken intra-operatively, just after extraction in the Group III (control), after extraction but before graft placement in Group I & II (study groups) and postoperatively at the end of first month and third month. Bone density of the post-extraction sockets was measured at four random areas through ‘densitometric analysis’ software in the OPG program (Kodak 8000C Digital Panoramic System, Eastman Kodak Company) and an average value was recorded at each review.
The objective of this present study was to radiologically assess and compare the regenerative potential of hydroxyapatite with collagen (G-Graft) & hydroxyapatite (G-Bone) from digital orthopantogram (OPG) using the Densitometric Analysis software and to evaluate the clinical usefulness of these materials to enhance bone healing in third molar extraction sites through of bone formation. Both materials are indicated for a wide range of bone grafting procedures.
Our results regarding interpretation by using densitometric analysis were similar to the study carried out by Khalid et al., who concluded that software analysis could be used to test the changes following bone augmentation procedures [11].
There are a number of fabricated bone graft substitutes based on hydroxyapatite or other calcium phosphate minerals that have been developed for these applications. These materials are available either as porous or dense granules of various sizes and are analogus to the natural mineral found in human bone in many ways. They have osteoconductive properties, biocompatibile and can be easily sterilized and used in the clinic. The calcium phosphate materials exhibit a higher solubility whereas hydroxyapatite materials demonstrate a low solubility, and thus are thought of as resorbable bone graft materials [1].
Collagen when used in conjugation with other osteoconductive carriers like hydroxyapatite or tricalcium phosphate and further when these composites are combined with autologous bone marrow, it acts as an osteoinductive material. The autologous bone marrow provides osteoprogenitor cells and other growth factors required for inducing new bone formation [12].
Hydroxyapatite is a highly crystalline form of calcium phosphate procured through a high-temperature reaction. It exhibits a chemical resemblance with the mineralized phase of bone and this similarity elucidate the excellent biocompatibility and osteoconductive capacity of this ceramic [12].
Wahl DA et al., proposed that, the composite of Hydroxyapatite & Collagen (G-Graft) may lead to earlier bone regeneration & greater density of the mature bone [13].
Skeletal bones mainly consist of collagen and carbonate substituted hydroxyapatite, both osteoconductive in nature and thus the implant fabricated from such costituents is likely to act in a similar way. Studies have shown that collagen type I and hydroxyapatite enhances osteoblast differentiation, but in combination, they accelerates osteogenesis. A composite matrix embedded with human-like osteoblast cells showed better osteoconductive properties compared to monolithic HA and produced calcification of identical bone matrix [13].
The present study demonstrated that the G-Graft has a definite regenerative potential and can be used in bony defects to enhance the bone healing and indicates that the defects treated with G-Graft attain more density initially and enhances bone healing in early stage. Therefore, G-Graft can be used for healing of an extraction socket where early implant placement is planned. All this was confirmed by a digital orthopantogram (OPG) using the Densitometric Analysis software, which favoured the Group I (Hydroxyapatite with Collagen) as compared to the group II (Hydroxyapatite) and III (no grafts was used).
The results of our study showed that the bone density readings in first and in third post-operative month had statistically highly as well significant difference in healing of the defects treated with G-Graft as compared to the control group. Araujo M et al., also found de novo hard tissue formation after 3 months, particularly in the cortical region of the extraction site using of hydroxyapatite/collagen composite (Bio-Oss Collagen) on healing of an extraction socket of dogs [14].
The results of our study also showed that bone density readings in the first as well as in third post-operative month had statistically significant difference in healing of the defects treated with G-Bone as compared to control group. The above findings, thereby providing enough evidence to prove that hydroxyapatite has the ability to facilitate osteogenesis. Our results are concurrent with the results of study conducted by Reddy R et al., who also reported increased bone density using G bone as compared to control sites [8].
While comparing measurements of bone density between the Group I (G Graft) and Group II (G Bone), it was noted that the third month postoperative results showed statistically significant difference in favour of G- Graft. Our results are concurrent with the result of study conducted by Johnson KD et al., who in their study, also reported better results with Collagen-hydroxyapatite composite in comparison to tricalcium phosphate, and hydroxyapatite used alone, in healing 2.5 cm bony defect created surgically in a canine radius model [15].
Hydroxyapatite is the one of the most extensively studied graft material but it is not clinically as preferable because of inadequate interaction with host tissues and improper fixation. Alternatively, the rapidly evolving technology has developed complexes such as hydroxyapatite plus collagen derivatives which imitate biochemical and biomechanical properties of natural bone in order to enhance osteointegration and graft healing for potential biomedical uses [16].
Recently, studies have been performed to demonstrate the efficacy of Bone Morphogenic Proteins in accelerating bone regeneration and fracture healing. For clinical use, rhBMP-2 (dibotermin alfa), is supplied within a bovine collagen sponge carrier with the product names InductOs® (UK) and InFUSE (US). The other clinically used BMP, rhBMP-7, are supplied in 1 g bovine collagen carrier in granular form with the brand names Osigraft® (UK) and OP-1 Putty (US). Platelets contain appreciable amounts of BMPs and the treatment of fractures with PRP is at least in part based on BMPs [17]. Calori et al., showed, however, that the application of rhBMP-7 as a bone-stimulating agent is superior compared to that of PRP with regard to their clinical and radiological adequacy [17,18].
Limitations
The main limitation of the present study was the small sample size on basis of which the role of collagen-hydroxyapatite composite in acceleration of bone healing cannot be fully ascertain though it was statically significant at 1 month and 3 month ( p <0.01)in study groups. Another limitation was in term of short duration of study i.e. 3 month. Longer study period are required for providing better assessment of graft healing and incorporation.
Conclusion
The present study was carried out to quantify changes in density during the healing phase and concluded that G-Graft has a definite regenerative potential and is better than G-bone and can be used in bony defects to enhance the bone healing without provoking any significant inflammatory process. The study also indicates that defects treated with G-Graft attain more density initially and that G-Graft enhances bone healing in early stage. Therefore, G-Graft can be used for healing of an extraction socket where early implant placement is planned. All this was confirmed by a digital orthopantogram (OPG) using the Densitometric Analysis software, which favoured Group (I) compared to the control Group II & III.