Paget’s Disease in Mandible: A Rare Occurrence in an Indian Sub-Continent
P. Srinivas Chakravarthi1, Ranjit Kumar Peravali2, Vivekanand Kattimani3
1 Professor, Department of Oral and Maxillofacial Surgery, SIBAR Institute of Dental Sciences, Guntur, Andhra Pradesh, India.
2 Reader, Department of Oral and Maxillofacial Surgery, SIBAR Institute of Dental Sciences, Guntur, Andhra Pradesh, India.
3 Assistant Professor, Department of Oral and Maxillofacial Surgery, SIBAR Institute of Dental Sciences, Guntur, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vivekanand Kattimani, Assistant Professor, Department of Oral and Maxillofacial Surgery, SIBAR Institute of Dental Sciences, Guntur, Andhra Pradesh -522509, India.
E-mail: drvivekanandsk@gmail.com
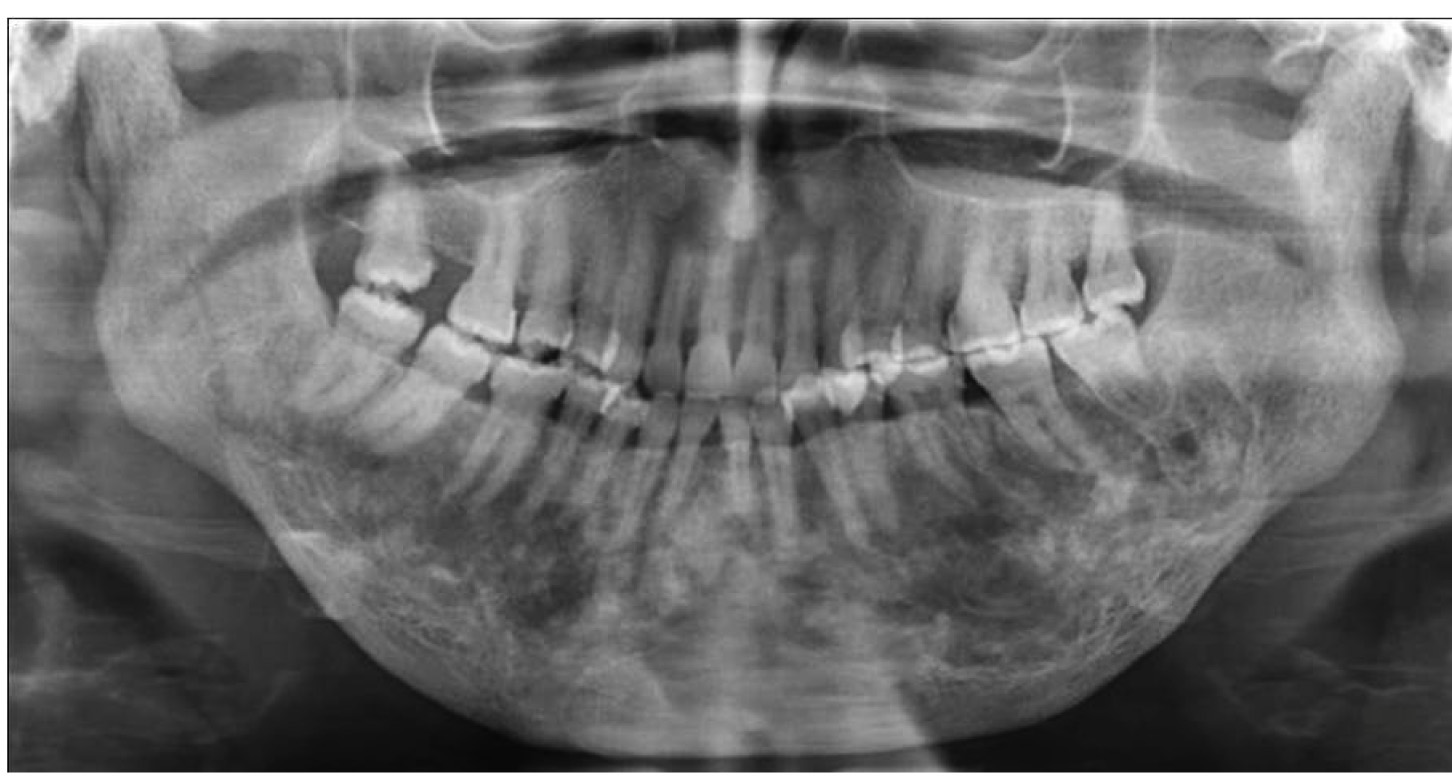
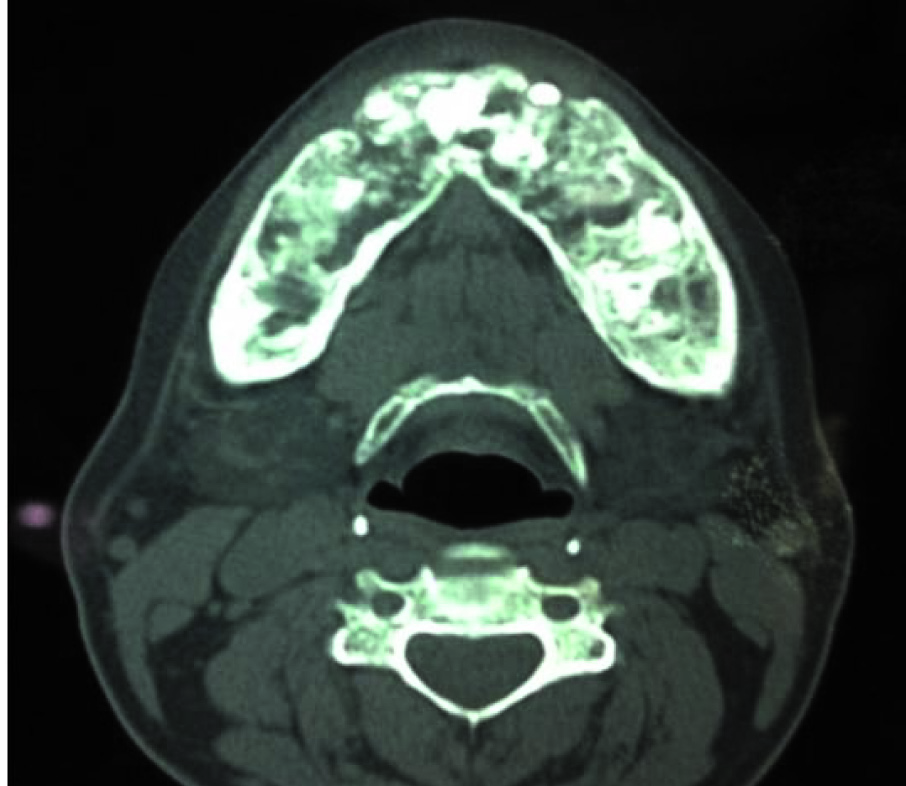
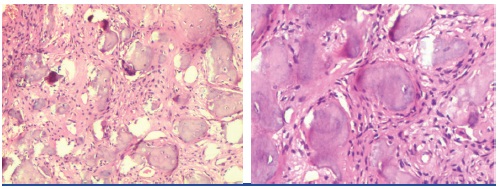
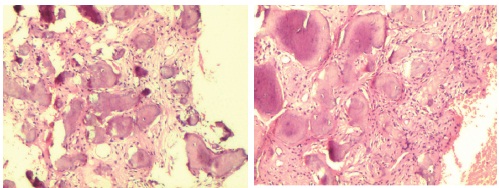
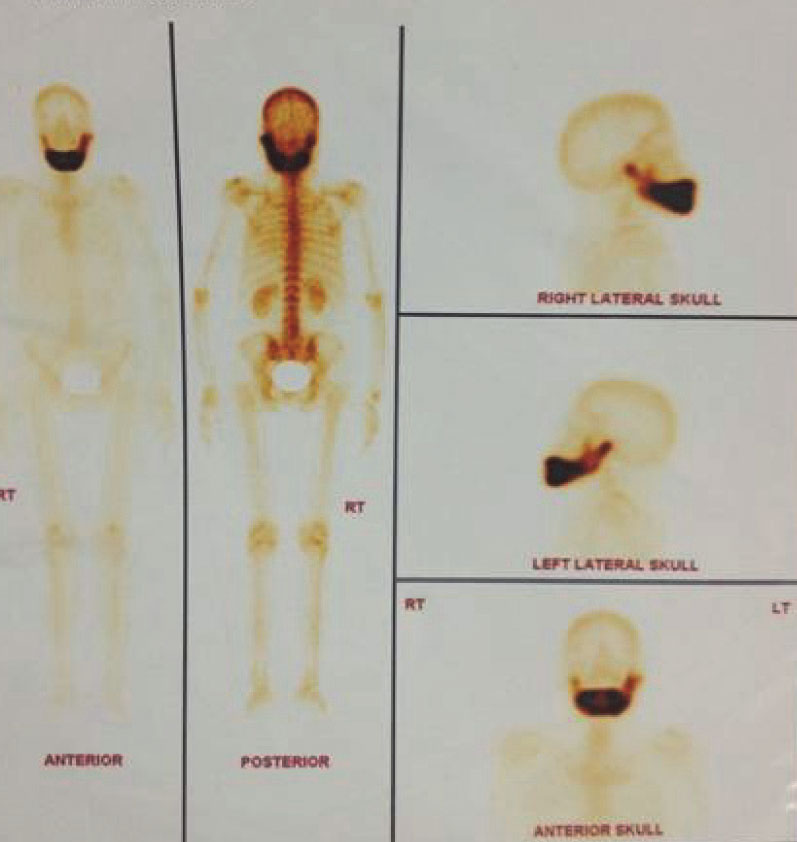
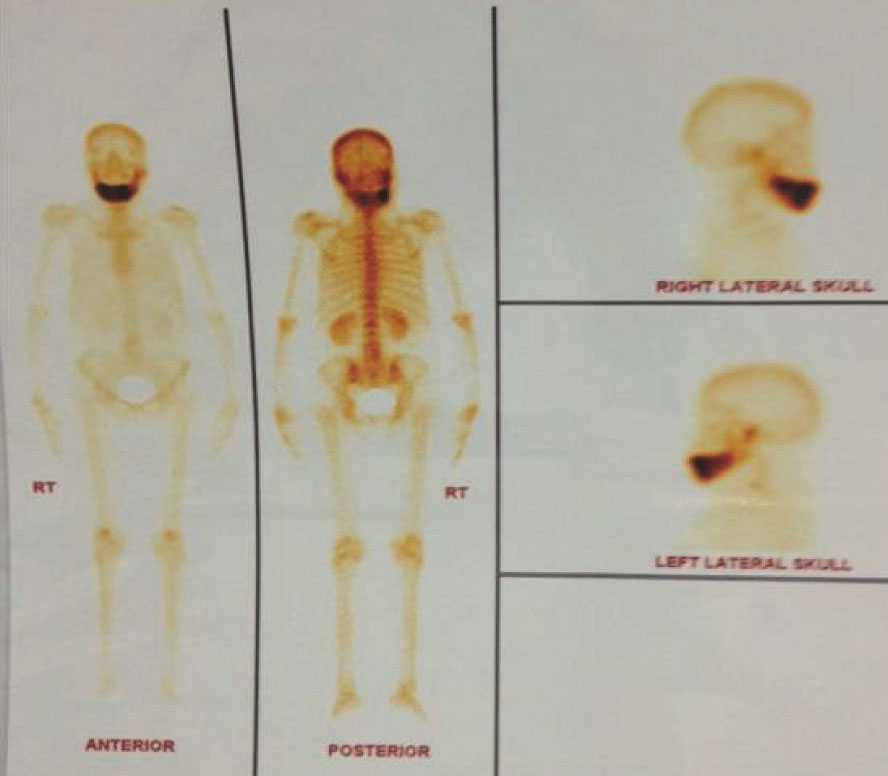
Bisphosphonates, Osteitis Deformans, Osteodystrophia deformans, Residronate
Female patient aged 50-year-old reported an extra oral swelling of lower jaw since 7 months. Broadening and widening of lower third of the face, with thick & incompetent lower lip seen [Table/Fig-1]. Swelling was nontender in the anterior alveolar bone with expanded cortical plates & no mobility of tooth felt after palpation [Table/Fig-2]. Orthopantomogram (OPG) showed irregular radiolucent areas with interspersed radio opacities confined to the anterior and body of mandible, hypercementosis of lower anterior teeth and resorption of roots [Table/Fig-3]. CT scan showed enlarged entire mandible with irregular intra medullary lytic lesion suggestive of fibrous dysplasia/ Paget’s disease [Table/Fig-4]. Incisional biopsy showed features of PD. The presence of irregular areas of bone formation with osteoblastic rimming of bone seen with haematoxylin and eosin stain at 10x and 20x magnifications [Table/Fig-5a,b]. The haematoxyphilic reversal lines seen within most of the areas of bone formation with vascular fibrous connective tissue with amount of inflammatory cell infiltrate at 10X and 20X magnifications [Table/Fig-6a,b]. Whole body bone scintigraphy performed using injection of 20m Ci Tc-99m MDP confirming increased tracer uptake in the mandible only [Table/Fig-7]. Mild increase in alkaline phosphatase (173 IU/L) seen. Based on these facts diagnosis of PD rendered and referred to an endocrinologist for medical management. Treatment was started with Tab. Risedronic acid 35mg orally once every day for two months. Posttreatment scintigraphy showed decreased tracer uptake in the mandible suggestive of good response to treatment [Table/Fig-8]. Patient followed up for more than 20 months successfully. Every six months patient asked for further follow up.
Pre-treatment frontal photograph showing facial asymmetry

Pre-treatment Intraoral view showing expanded cortical plates

Orthopantomogram showing irregular radiolucent areas with interspersed radio opacities
Computerised tomography scan of axial view of mandible showing irregular intra medullary lytic lesion
Haematoxylin and eosin staining of Biopsy specimen at 10X & 20X magnification showing irregular areas of bone formation respectively
Microscopic picture of biopsy specimen showing haematoxyphilic reversal lines with fibrous vascular connective tissue. At 10X & 20 X magnification respectively
Pretreatment bone scintigraphy showing increased tracer uptake
Post-treatment bone scintigraphy showing reduced tracer uptake
PD is disorder of the skeleton results in enlarged & deformed bones. PD showed predilection of male-to-female (3:2) ratio. PD is rare in India, China and Malaysia [1]. Some studies suggested an association of Vitamin D deficiency [2] & viral infection inclusion bodies resembling paramyxovirus nucleocapsid particles in Paget’s osteoclasts [3]. It may present as a coincident with hyperparathyroidism. The bone shows ground glass appearance during early osteolytic stage, later during osteoblastic stage bone gives ‘cotton wool ’ appearance on X-ray film [3]. Pulp chambers of tooth may be calcified, loss of lamina dura and hypercementosis of roots seen [4]. On the other hand during lytic phase of PD root resorption may occur associated with loosening of teeth [5].
Diagnosis is based on clinical, radiographic, bone scintigraphy and histologic features. Deformity involving skull or bowing of long bones which may result in fracture and neurological signs like deafness, cranial nerve palsies and even neoplastic transformation should be examined by plain radiographs [6]. The biochemical values of total plasma alkaline phosphatase activity is elevated in 85% of patients with untreated PD [7] but in our case marginal increase seen.
Management mainly aimed at symptomatic (pain control) and specific treatment (Calcitonin, Bisphosphonates). Intravenous bisphosphonates pamidronate, oral alendronate, oral residronate [8] normalize high levels of bone alkaline phosphatase. In our patient residronate 30mg/day for 2months was advised followed by whole body bone scan which showed marked decrease uptake of isotope and biochemical values are within normal limits. Residronate appeared to have excellent safety profile and well-tolerated [8].
PD is considered to be very rare in Indian subcontinent. Its typical clinical features when it involves the maxillofacial region should lead to a high degree of suspicion to arrive at a diagnosis with unknown aetiology. Residronate appeared to have excellent results. Physicians should be aware of the potential for hypocalcemia when patients with polyostotic PD and markedly elevated indicators of bone remodelling are initiated with powerful anti-resorptive therapy.
[1]. Joshi SR, Ambhore S, Butala N, Patwardhan M, Kulkarni M, Pai N, Paget’s disease from western IndiaJ Assoc Physicians India 2006 54:535-38. [Google Scholar]
[2]. Karunakaran K, Murugesan P, Rajeshwar G, Sharlenesara Babu S, Paget’s disease of MandibleJournal of oral and maxillofacial pathology 2012 (16):107-09. [Google Scholar]
[3]. Wen-Chen Wang, Yi-Shing Lisa Cheng, Chung-Ho Chen, Paget’s disease of bone in a Chinese patient: A case report and review of the literatureOral Surg Oral Med Oral pathol Endo 2005 99(6):727-33. [Google Scholar]
[4]. Rosario Carrillo, Antonio Morales, Jose Luis Rodriguez-Peralto, Benign fibro-osseous lesion in PD of jawsOral Surg Oral Med Oral Pathol 1991 71:588-92. [Google Scholar]
[5]. Barnett F, Elfenbein L, Paget’s disease of the mandible: A review and report of a caseEndod Dent Traumatol 1985 1:39-42. [Google Scholar]
[6]. Kanis JA, Pathophysiology and Treatment of Paget’s disease of Bone 1998 2nd EdLondonMartin Dunitz:110-38. [Google Scholar]
[7]. Eastell R, Biochemical markers of bone turnover in Paget’s disease of boneBone 1999 24(5):49-50S. [Google Scholar]
[8]. Brown JP, Chines AA, Myers WR, Eusebio RA, Improvement of Pagetic Bone Lesions with Residronate Treatment: A Radiologic StudyBone 2000 26(3):263-67. [Google Scholar]