The predictability of Osseointegrated oral implants in the treatment of both total and partial edentulism with sufficient bone quantity and quality has been well-documented [1]. A minimum of 10mm of vertical bone height is usually required for predictable implant success [2]. However, the placement of dental implants in the atrophic posterior maxilla is challenging in implant surgery which has been related to bone quality and quantity [3]. Several procedures and materials have been developed to overcome the problem of reduced amount of bone like tilted implants, short implants and vertical bone augmentation. But impredictable success rates have been reported with tilted implants and short implants [4].
Many techniques have been introduced addressing vertical bone augmentation like sinus floor elevation (SFE) from a lateral window or SFE from a crestal approach using osteotomes, onlay graft, guided bone regeneration, appositional bone graft/saddle-graft or combinations of these techniques. Today, two main procedures are used for SFE and implant placement namely the ‘Lateral window approach’, first presented by Tatum in 1977 and the ‘Transcrestal approach’ Techniques which was described by Summers in 1994 [5,6].
Though good implant survival rates are being reported with these procedures, the postoperative morbidity was noticed to be higher with these techniques [7]. Hence, modifications of these techniques have been suggested by various authors and thus the ‘Minimally invasive Techniques’ have come to stay [8,9]. The search towards alternative method for sinus augmentation led to the evolution of the “The innovative implant technology (IIT) Sinu Lift System” one of the minimally invasive indirect sinus lift instrument. This technique becomes more predictable if used in combination with PRP and β –TCP mix which may result in an increased rate of bone formation and sinus augmentation [10,11]. The present study was undertaken to evaluate the clinical and radiological outcomes and postoperative morbidity of sinus floor elevation procedures performed using the minimally invasive surgical technique the Sinu liftsystem, and β- TCP (Cerasorb M) in conjunction with PRP.
Materials and Methods
The protocol of this study was revised and approved by the Department of Periodontics, Ragas Dental College and Hospital, Chennai, India. Written informed consent was obtained from those who agreed to participate voluntarily prior to clinical trial and ethical clearance was obtained from scientific review board (srb) and Institutional review board and independent ethical committee. The study was conducted between March 2008 to April 2012.
Selection of Subjects
The present study group comprised of ten subjects (6 males and 4 females) in the age range of 25-55 y, with referral for fixed restoration (implant placement) in the posterior maxillary edentulous area. Patients were selected using the following criteria.
Inclusion criteria
Partially edentulous jaws with a unilateral or bilateral loss of teeth in the maxillary premolar or molar area.
Patients with acceptable oral hygiene status and no active periodontal disease
Residual alveolar ridge height of 5mm or less, with no buccolingual augmentation;
Systemic and local conditions were compatible with implant placement and SFE procedures.
The exclusion criteria
The presence of uncontrolled diabetes, autoimmune diseases; radiation or chemotherapy to the head and neck region.
Uncontrolled periodontal disease.
Active sinus infection.
Smokers, alcoholic and drug abusers.
Blood disorders.
When the septum is present at the location where sinus membrane lift is desired.
All the subjects selected for the study fulfilled the above criteria.
Overview of Study Design
The study involved selected subjects requiring fixed restoration (implant placement) after sinus lifting. In the context of this study 10 subjects met the above criteria (Total Sample size is n=10)
Statistical Analysis
Level of significance @ 5% (0.05): Power @ 90%
The following methods of statistical analysis have been used in this study: Wilcoxson signed rank test: To compare and correlate preoperative and postoperative CT Scan.
Description Of Sinu Lift System Kit: The sinu lift system disposable kit was used in this study [Table/Fig-1]. It consists of a 3.2mm Sinu start drill that drills the path to the Sinus membrane which disengages upon contact with the membrane to avoid rupture. The 3 mm yellow curette is used to gently separate the sinus membrane from the bone. The 4.2 mm blue curette is used for additional elevation. It also consists of a bone packer, a multifunction handle to help turn wheels and provide additional reach. Front part of handle, pointed tip couples with the holes in the Sinu Drill provides leverage while drilling through the bone with Sinu Drill, whereas the rear part of handle snaps the curette (or) bone packer into the open end of the handle.
Preparation of Subjects: An impression of the maxillary arch was made using alginate impression material (Tulip Alginate Impression Material, Cavex, Holland Bv, Haarlem Holland) and poured in dental stone(Ultrarock, Kalabhai Karson Pvt. Ltd, Mumbai, India).
Radiographic evaluation: The preoperative radiographic evaluation included periapical, panoramic radiography and CT Scan (GE Electricals, Milwakee, WI, U.S.A). Panoramic (or) tomographic x-rays viewed to identify the presence of any septum, and the correct buccolingual inclination was determined. A CT Scan with a metal ball stent was taken to evaluate the vertical height from an arbitrary horizontal line joining the CEJ from the adjacent teeth to the floor of the sinus lining [12]. The following three points were marked on the arbitrary horizontal line joining the CEJ [Table/Fig-2]. This points were marked to find out the “desired area of sinus augmentation”, whether it is Point A or point B or point C and also for the implant placement in that region.
Description of sinu lift kit

Radiographic interpretation of point A,B,C
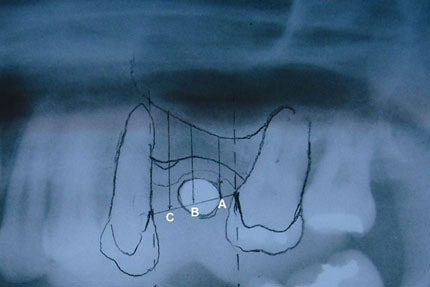
Point A: 2mm from the mesial tooth.
Point B: Midpoint from the line joining point A and C.
Point C: 2mm from the distal tooth.
From the points mentioned above, a vertical arbitrary line was drawn to the floor of the maxillary sinus lining and the values were recorded.
Surgical Phase
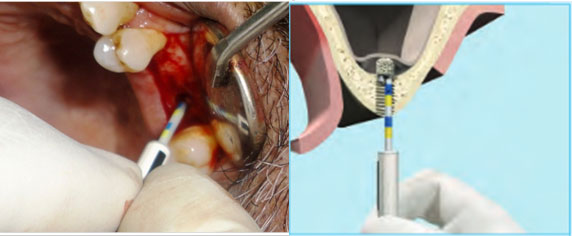
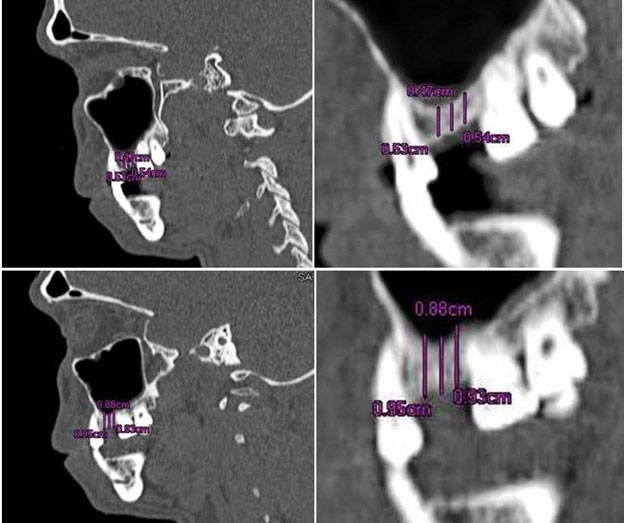
A dose of prophylactic antibiotic, Amoxycillin 2gm one hour before the surgical procedure and rinsing with 0.2% chlorhexidine for two minutes. The sinus augmentation was then carried out according to the surgical protocol. Posterior and middle superior alveolar nerve block along with greater palatine nerve block was given with 2% lignocaine with adrenaline. An incision was made palatal to the mid alveolar crest and connected with a sulcular incision to the adjacent teeth. Mucoperiosteal flap was elevated, and the implant location on the exposed bone with surgical stent in place was marked with the round bur [Table/Fig-3]. A 2mm twist drill advanced to 1-2mm short of maxillary sinus membrane and wherever needed, depth gauge was used to check the orientation and depth of the prepared site by means of RVG (Kodak, care stream india pvt. ltd.) [Table/Fig-4]. The osteotomy site was further enlarged with the 3.2mm Sinu start drill. The Sinu Drill was advanced into the prepared opening using the white wheel until the cutting blade of it is pushed into the Sinu Drill [Table/Fig-5]. This engages the green wheel. Once it engaged by repeated applying the torque on the green wheel in clockwise direction upto 3/4th of full turn, followed by 5 degree-10 degree in counter clockwise direction, the Sinu Drill has been advanced until the cutting blade reaches the sinus membrane and it was confirmed by the releasing of green wheel. After that green wheel got disengaged and rotated freely, by turning the white wheel in a counter clock wise direction the Sinu Drill was removed. The Sinus membrane was elevated gently by first using 3.0 mm curette making sure the tip of the curette was in contact with the bone to avoid membrane rupture and then further elevation was done with the 4.2 mm curette with a flexible tip and guided by ‘color markings’ present on the curette till the desired membrane elevation was obtained [Table/Fig-6]. The space was filled incrementally with pure phase synthetic β-TCP (Curasan AG GmbH, Kleinostheim, Germany) sized 500-1000 μm mixed with PRP (obtained using the proposed technique by Marx RE and Garg AK and coagulation of platelet rich plasma was obtained by adding 1ml Batroxobin and 1ml of 10% Calcium gluconate which was shaken in a sterile tube for approximately 30 sec), by the help of graft material packer and the mucoperiosteal flap was repositioned and closed using simple interrupted sutures (3-0 black silk) [Table/Fig-7]. Postoperative radiograph was obtained after graft placement to evaluate the sinus augmentation site [Table/Fig-8]. Antibiotics and Anti inflammatory analgesics were prescribed for five days and postoperative instructions were given. After six months, CT Scan was taken to evaluate for the gain in vertical bone height, followed by implant placement at the desired area of sinus augmentation [Table/Fig-8]. Patients were followed upto two years.
Pre-operative view and after mucoperioosteal flap elevation

Initial osteotomy prepared with 2mm twist drill
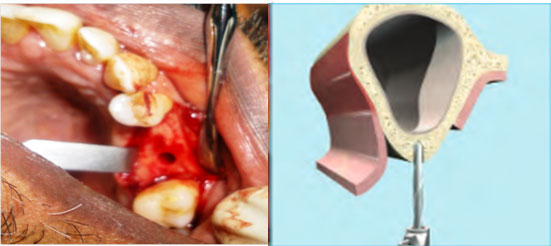
Advancing Sinu Drill in prepared osteotomy

Separating the sinus membrane with curette

Using Bone Packer for membrane graft condensation
Radiographic interpretation of pre and post operative CT Scan
Results
All data were analysed by using the statistical program of social science version 16.0(SPSS Inc, Chicago, USA).Mean duration of the sinus lift procedure was 22.6±7.5min. The mean bone height measurements at reference points A, B and C was 2.85mm, 3.17mm, 1.19mm respectively, as revealed by the CT Scan which was statistically significant (p<0.01) [Table/Fig-9]. The mean bone height at the desired area of sinus augmentation was 4.40mm which is also statistically significant (p < 0.01) [Table/Fig-10].
Comparison of pre operative and post operative mean bone height at three reference points using CT Scan
| Parameters | Pre – Operative (mm) | Post – Operative (mm) | Mean Gain in Bone Height (mm | p- value |
|---|
| Ref.- Point | n | Mean±SD | N | Mean±SD | | |
|---|
| A | 10 | 6.22±1.30 | 10 | 9.07±1.79 | 2.85 | 0.005** |
| B | 10 | 5.53±0.72 | 10 | 8.70±2.74 | 3.17 | 0.005** |
| C | 10 | 6.03±1.07 | 10 | 7.22±2.16 | 1.19 | 0.009** |
*denotes significance at 5% level: **denotes significance at 1% level
Comparison of pre operative andpost operative mean bone height only at the desired area of the sinus augmentation using CT Scan
| n | Pre – Operative (mm) | Post – Operative (mm) | Mean Gain in Bone Height (mm | p- value |
|---|
| Mean±SD | Mean±SD |
|---|
| Bone Height (C T Scan) | 10 | 5.80±0.98 | 10.20±1.68 | 4.40 | 0.005** |
*denotes significance at 5% level: **denotes significance at 1% level
Discussion
Maxillary sinus augmentation surgical techniques as well as the osteoconductive potential of various bone substitutes have evolved greatly allowing the predictable and successful placement of dental implants in the atrophic posterior maxillary region [13,14]. Several studies have reported excellent long term survival rates for implants placed in the augmented maxillary sinuses [15,16].
The most commonly used approach, the lateral window technique had potential complications like membrane perforation (11-56%), tearing of the membrane, bleeding, infection, and sinus obstruction [7].This technique requires considerable surgical skill and time and also often giving rise to unpleasant sequelae such as edema and discomfort. A less invasive alternative was introduced by summers known as the osteotome or bone added osteotome sinus-floor elevation (BAOSFE) technique, but it has been shown to yield only a modest increment in bone height of only 3±0.8 mm [17]. Also, a systematic review by Tan WC et al., [18] reported incidences of membrane perforation ranging from 0% to 21.4% and post-operative infection from 0%to 2.5% after transcrestal SFE by means of various surgical procedures. The episodes of BPPV (Benign paroxysmal positional vertigo) seen in the patients who underwent SFE with osteotome Technique as a result has made it an obsolete therapy [19]. So, current trend centers on the development of minimally invasive techniques, which are designed to minimize postoperative morbidity, while concurrently achieving maximal augmentation.
As the single stage technique was beset with major drawbacks associated with implant stability and parallelism and a host of technical problems and complications, the Two stage delayed approach was planned [20]. Here, the initial bone height was less than 5-6mm necessitating graft incorporation. The first step was the sinus membrane elevation followed by grafting for revascularization and integration. The second step is the implant placement six months later, as this promoted an immediate healing response similar to that of viable bone.
The present study reports a minimally invasive two staged procedure for maxillary bone augmentation using the “Sinu-lift system” utilizing β-TCP in conjunction with PRP. The sinu lift system with the sinu drill, an intelligent self regulating mechanical hand device and the curettes with color codings allow the accurate control of the working length providing the desired membrane elevation, minimizing the risk for membrane perforation and post surgery infections. The mean bone height measurements at reference points A, B and C was 2.85mm, 3.17mm, 1.19mm respectively, as revealed by the CT Scan which was statistically significant (p<0.01) [Table/Fig-9]. The mean bone height at the desired area of sinus augmentation was 4.40mm which is also statistically significant (p < 0.01). Implants were placed after six months in the augmentation site for all the patients. Since the purpose of our study was to prove the minimal invasiveness of sinu lift system, no statistical analysis was performed on parameters regarding implants.
In this study, no complications were observed either during surgical procedure or after the completion of surgery upto six months period of this study. No membrane perforation was recorded during or immediately after the sinus lift procedure when the valsalva maneuver was performed. Postoperatively all patients were seen at regular intervals asked specifically about sinus problems like nasal congestion, pathologic secretion and headache. There was no mucosal redness or oedema or any mucopurulent discharge. CT Scans did not reveal any mucosal thickening, air fluid levels or opacifications postoperatively. Naso endoscopy or nasal decongestants are not necessary since only patients without sinus problems and with no radiographic evidence of sinus pathology were included for the study [7]. This was probably the result of a meticulous surgical protocol and patient selection and the minimal invasiveness of the sinu-lift system. Thus the sinu-liftsystem seems to score here.
A more radiopaque appearance in CT Scan was observed after six months post-operatively revealing that new bone formation (osteogenesis) had occurred replacing the graft material because of the osteoconductive nature of the graft and addition of PRP which would have accelerated this osteogenic process by enriching the bone grafts with the high concentration of growth factors as revealed in previous studies [21,22].
CerasorbM 500-1000 μm was used for the study. The use of bone substitutes becomes more predictable if they are used in combination with PRP [23]. Hence, it was used in combination with CerasorbM here.
Studies published on Indirect osteotome maxillary sinus floor elevations between 1999 and 2010 on patients with a minimum of one year of follow-up were analysed by Romero Millan J et al., Schneiderian membrane perforation was the most frequent complication [24]. In this study, no such complications were recorded. Study done by Kim DY et al., related to evaluation of the effectiveness of a water lift system in the sinus membrane-lifting operation as a sinus surgical instrument reported membrane tearing due to application of excessive hydraulic pressure [25]. Another study on the outcomes of flapless crestal maxillary sinus elevation under hydraulic pressure done by Bensaha T, reported implant loss and post operative complications like prolonged edema in the lower eyelid region [26]. No such complications were observed with the proposed technique. Also, in this study no episodes of BPPV were observed at either the time of sinus lift procedure or seven days after surgery.
Some limitations should be considered like the presence of attachments which cannot be reused, specific equipment and the need for special training and the cost of the procedure.
Conclusion
Thus, it is appropriate to conclude that sinus-floor elevation using the “sinu-lift system” is definitely a reliable tool in achieving maximum sinus lift for augmentation. Future directions should see a more pivotal role to be played by this method of sinus lift prior to implant placement and it has obvious advantages, paving the way for maximal augmentation for successful implant placement, while using minimally invasive techniques. The proposed technique is minimally invasive, decreases the chair time, makes implant dentistry more accurate with predictable out comes and increases the comfort level for implant patients. With preparation, education and experience, it is a procedure which greatly benefits the patient with predictable outcomes. However, a long term evaluation with prospective randomized controlled clinical trials with a greater sample size and histomorphometric analysis would lend more credibility to this study by scientific evidences.
*denotes significance at 5% level: **denotes significance at 1% level
*denotes significance at 5% level: **denotes significance at 1% level