Embryonal Rhabdomyosarcoma (RMS) of Retroperitoneum in Young Child
R.G. Naniwadekar1, Mayank A. Vekariya2, S.R. Kulkarni3, Akshay S. Pednekar4, Vaibhav Gupta5
1Associate Professor, Department of General Surgery, Krishna Institute of Medical Sciences University and Research Centre, Karad, Maharashtra, India.
2P.G. Resident, Department of General Surgery, Krishna Institute of Medical Sciences University and Research Centre, Karad, Maharashtra, India.
3Professor, Department of General Surgery, Krishna Institute of Medical Sciences University and Research Centre, Karad, Maharashtra, India.
4 P.G. Resident, Department of General Surgery, Krishna Institute of Medical Sciences University and Research Centre, Karad, Maharashtra, India.
5 P.G. Resident, Department of General Surgery, Krishna Institute of Medical Sciences University and Research Centre, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mayank A. Vekariya, Room no. 29, IHR Boys Hostel, Krishna Hospital Campus, Malkapur, Karad-415110, Maharashtra India.
E-mail: dr.mayankvekariya@ymail.com
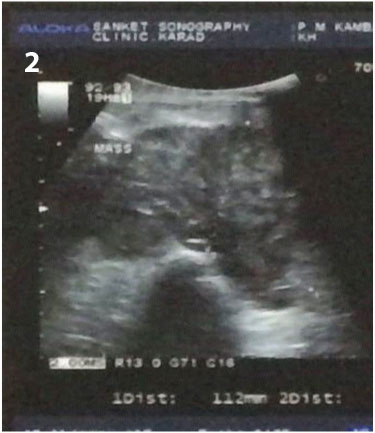
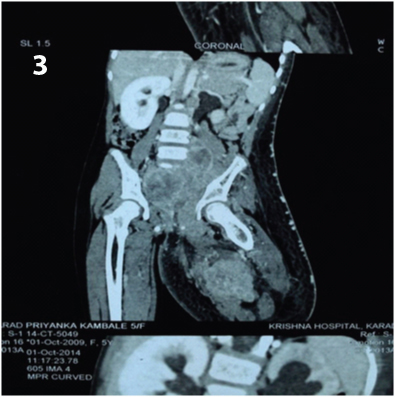
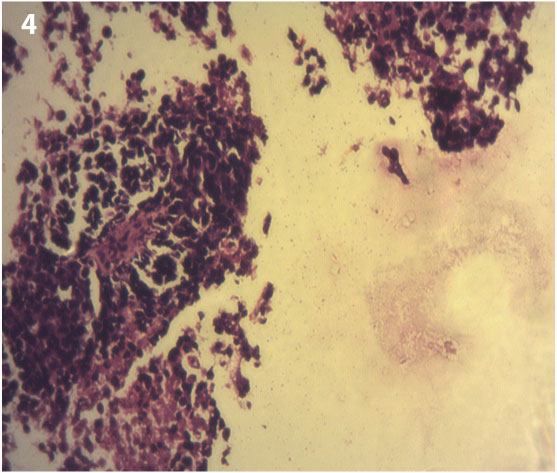
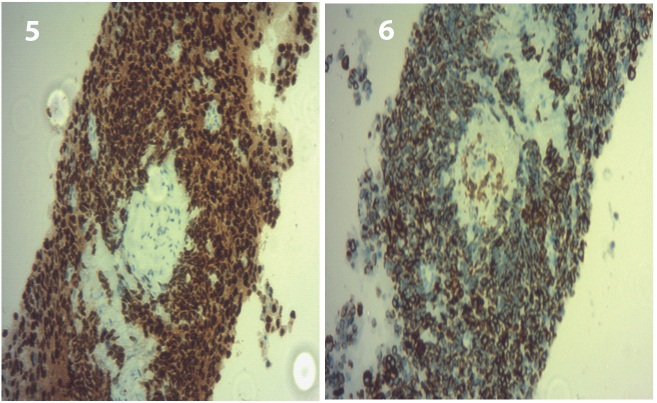
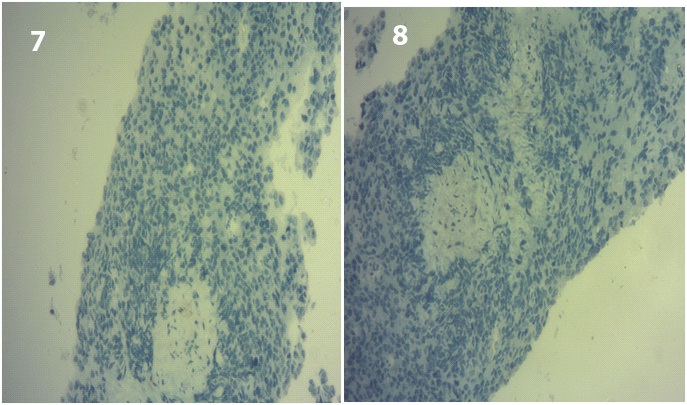
A 5-year-old female child was brought by parents to General Surgery department of Krishna hospital with complaints of fullness in left lower abdomen and swelling over left thigh since last 15 days. Since 15 days patient had fullness in left iliac fossa which rapidly increased in size and was associated with pain. Gradually patient had developed swelling over left thigh [Table/Fig-1]. On general examination patient was well built and nourished and apatite was not reduced only pallor was present. On examination of abdomen there was a palpable mass of 15 X 5 cm in left iliac fossa which was fixed to underlying tissues, hard in consistency. The swelling on the left thigh also was fixed to underlying tissues and hard in consistency. All peripheral pulses were palpable. Based on above findings our clinical diagnosis was mass arising from abdomen and extending into the left thigh. Ultrasonography of abdomen and pelvis suggestive of a large illdefined, isoechoic, solid, retroperitoneal mass [Table/Fig-2] of indeterminate origin in pelvis, posterior to bladder measuring about 112 x 60 x 88 mm in size with fixity to adjacent pelvic vasculature. Few retroperitoneal nodes were enlarged. Computed tomography scan of abdomen suggestive of large, ill defined, lobulated pelvic mass extending to left thigh [Table/Fig-3] causing mass effect with lymphadenopathy. USG guided tru-cut biopsy from abdominal and left thigh mass done which showed malignant small blue round cell tumour [Table/Fig-4]. Immunohistochemistry performed which showed that tumour cells exhibit immunopositivity for myogenin/desmin [Table/Fig-5,6] and are immunonegative for TdT/CD99 [Table/Fig-7,8] which confirmed the diagnosis of Embryonal Rahabdomyosarcoma. As mass was fixed to pelvic vasculatures, it was impossible to operate so patient was refered for chemotherapy and Radiotherapy. Chemotherapy regime VAC (Vincristine, Actinomycine-D and Cyclophosphamide) was started along with Radiotherapy. Last follow up was done after one month and patient was doing well.
Discussion
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma of childhood and adolescence. RMS is a malignant tumour of mesenchymal tissue. It shows varying degree of differentiation [1]. RMS is the most common soft tissue tumour of childhood [2]. It is commonly affect in the head and neck region, genitourinary tract, retroperitoneum and, to a rare extent, the extremities [3]. RMS of extremities are fast growing and carry very poor prognosis.
RMS is a common childhood malignancy, commonly seen in age 3 to 12 y. It is present in 50% of the all soft tissue sarcoma in children. Rhabdomyosarcoma is a malignant tumour of mesenchymal tissue. RMS can occur at any site, although it has a predilection for the head and neck, genitourinary organs, retroperitoneum, and extremities [4]. The embryonal subtype is the most common, representing up to 60-80% of tumours at above sites. Alveolar tumours are more common among adolescents, often arise in the extremities and carry a worse prognosis. On immunohistochemistry embryonal RMS may express vimentin, desmin, actin, myoglobin, myosin, creatine kinase M, titin, dystrophin and acetylcholine receptor antigen [5]. There are four types of RMS histologically, Embryonic, Botryoid, Alveolar and Pleomorphic or anaplastic. Out of this Embryonic subtype presents in more than 70% of all patients of RMS. Embryonic subtypes of RMS rarely involves the regional lymph nodes. RMS most often present as an expanding mass, resulting in pain and symptoms related to the compression of nearby structures [6].
The identification of RMS and its histological subtypes is important because alveolar RMS has been reported to have a poor prognosis and it is associated with a higher rate of disseminated metastases. The diagnosis of most pediatric solid tumours require extensive immunohistochemical markers because they often exhibit a nonspecific small round cell tumour phenotype [7].
RMS is treated by a combination of surgery, chemotherapy, and radiation. If tumour is surgically inoperable then initially radiotherapy and chemotherapy given to shrink the tumour followed by wide surgical excision of the tumour performed. Chemotherapeutic agents commonly used are vincristine, cyclophosphamide, dactinomycin, adriamycin, ifosfamide, VP-16. With combined modality of treatment - chemotherapy, radiation therapy, and surgery - the overall survival rate for all pediatric RMS is 71% [8].
Clinical photograph of mass in lower abdomen extending into left thigh

Showing Ultrasonographic image of mass in lower abdomen and left thigh
Showing Coronal section of computerized tomography scan showing mass in pelvis extending into left thigh
Showing microphotograph of biopsy from mass showing multiple blue round tumour cells
Microphotograph of IHC with myogenin and desmin stain shows immunopositivity to tumour cells
Showing ultrasonographic image of mass in lower abdomen and left thigh
[1]. Duraes Gabriela Versiani, Jham Bruno Correia, Mesquita Ana Terezinha Marques, Santos Cassio Roberto Rocha dos, Miranda Joao Luiz, Oral embryonal rhabdomyosarcoma in a child: A case report with immunohistochemical analysisOral oncology extra 2006 42(3):105-08. [Google Scholar]
[2]. G Pastore, Bonet Peris, M Caril, Childhood soft tissues sarcomas incidence and survival in European children ( 1978 -1997 ): report from the automated children cancer information system projectEur j cancer 2006 42:2136 [Google Scholar]
[3]. Peters E, Cohen M, Altini M, Murray J, Rhabdomyosarcoma of the oral and paraoral regionCancer 1989 63(1):963-66. [Google Scholar]
[4]. WA Newton, EA Gehan, BL Webber, HB Marsden, AJ van Unnik, AB Hamoudi, Classification of rhabdomyosarcomas and related sarcomas. Pathologic aspects and proposal for a new classification: An Intergroup Rhabdomyosarcoma StudyCancer 1995 76:1073-85. [Google Scholar]
[5]. A Rosenberg, Bones, joints and soft tissue tumors. In: Cotran R, editor. Robbins Pathologic Basis of DiseaseTetracyclineTeratology 1999 6th EditionPhiladelphiaWB Saunders:1215-68. [Google Scholar]
[6]. NG Wendy Kar Yee, Embryonal Rhabdomyosarcoma in a Young BoyMcgill J Med 2007 10:16-19. [Google Scholar]
[7]. NJ Sebire, Myogenin Malone M, Myo D1 expression in paediatric rhadomyosarcomasJournal of Clinical Pathology 2003 56:412-16. [Google Scholar]
[8]. MB Mc Carville, SL Spunt, AS Pappo, Rhabdomyosarcoma in Pediatric PatientsAmerican Journal of Roentgenology 2001 176:1563-69. [Google Scholar]