Cronkhite-Canada Syndrome (CCS)—A Rare Case Report
Subrata Chakrabarti1
1Post Graduate Trainee, Department of General Medicine, Ipgmer, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subrata Chakrabarti, Doctor’s Hostel, AJC Bose Road, Kolkata-700020, India.
E-mail: subratachakrabarti2011@gmail.com
Cronkhite-Canada syndrome (CCS) is an extremely rare non-inherited condition characterized by gastrointestinal hamartomatous polyposis, alopecia, onychodystrophy, hyperpigmentation, weight loss and diarrhoea. The aetiology is probably autoimmune and diagnosis is based on history, physical examination, endoscopic findings of gastrointestinal polyposis, and histology. The disease is very rare; approximately 450 cases of CCS have been reported worldwide. The author reports a case of CCS in an elderly Indian male.
Alopecia, Hyperpigmentation, Polyposis, Onychodystrophy
Case Report
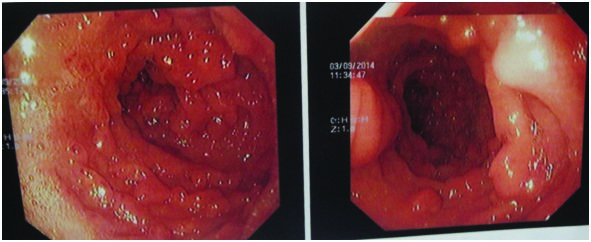
A 68-year-old male presented with weight loss, non-bloody watery diarrhoea, and an altered sense of taste for the past six months. There was no history of fever or abdominal pain. His past history was insignificant. He was non-diabetic and non-hypertensive. He had no relevant family history or that of chronic intake of any drug. On physical examination, he had pallor, hyperpigmentation of both hands and feet involving both soles and feet [Table/Fig-1,2], alopecia, and dystrophic nail changes [Table/Fig-3,4]. However, pigmentation within oral cavity was not noted. Vitals were within normal limits. Signs of vitamin deficiency were noted. His abdomen was soft, non-tender, and non-distended. Rest of the physical examination was non-contributory. Investigations revealed normocytic, normochromic anaemia and hypoalbuminemia. He had occult- blood positive stool. The laboratory parameters including renal and liver function tests, serum electrolytes were within normal limits except hypoalbuminemia (2 g/dl; normal 3.5 -5 g/dl). The patient underwent an upper endoscopy and colonoscopy to further investigate his condition. Endoscopic evaluation revealed multiple sessile polyps in the stomach, small bowel, and colon and rectum [Table/Fig-5,6]. Histopathologic examination of biopsies obtained from these polyps showed cystic dilatation and distortion of glands with inflammatory infiltration, esinophillic predominance and stromal oedema. The findings were consistent with juvenile or inflammatory polyps. CCS was diagnosed based on a combination of clinical features, endoscopic findings and histopathology of polyps. Treatment with oral Prednisolone (started at 1 mg/kg daily with plan for gradual taper based on response), sulindac (150 mg daily) and pantoprazole (40 mg daily) was initiated which partially relieved his symptoms. As the patient was able to take foods orally, total peripheral nutrition (TPN) was not required. He was asked to continue the oral drugs for atleast one year. He was discharged in stable condition and advised to undergo regular annual endoscopic study.
Discussion
CCS is a clinico-pathologic diagnosis based on features of malabsorption in the setting of characteristic clinical, endoscopic, radiologic, and histologic findings. Clinical description of CCS was first made by Cronkhite and Canada in 1955 [1]. However, Jarnum and Jensen first established the term CCS in 1966 [2]. The estimated incidence of CCS is extremely rare-one per million according to the largest study on CCS involving 110 patients. Patients of European or Asian descent are most frequently affected and most of the cases are reported from Japan [3].
CCS can develop in all ethnic groups. A slight male predominance is noted in almost all studies. The disease is sporadic and there is no strong evidence to suggest a familial predisposition. Autoimmune aetiology is probably involved in pathogenesis, given the increased immunoglobulin (Ig)G4 mononuclear cell staining in CCS polyps [4]. Autoimmune diseases such as hypothyroidism, systemic lupus erythematosus, rheumatoid arthritis and scleroderma are often found in increased frequency with CCS. Elevated antinuclear antibody (ANA) and IgG4 levels have also been observed in some patients [5].
Symptomatic disease onset occurs in fifth to sixth decade. Diarrhoea and dysguesia are the most common initial symptoms, with the dermatologic triad of alopecia, hyperpigmentation, and onychodystrophy often occurring later. Gastrointestinal polyposis is closely related to the malabsorption which induced these ectodermal changes [6]. The index patient was a 68-year-old male with characteristic manifestations. Yun et al., reported a case of CCS in a 72-year-old male patient who presented with diarrhoea and weight loss along with both hand and feet nail dystrophy, hyperpigmentation, and alopecia [7]. Kao et al., mentioned a case of a 39-year-old Filipino woman who initially presented with diarrhoea but later developed significant amount of hair loss as well as hyperpigmentation of her palms and soles [8]. Seshadri et al., reported yet another case of CCS in a 78-year-old Chinese man who presented with weight loss, diarrhoea and an altered sense for six months and was found to have hyperpigmentation of both hands, alopecia and atrophic nail changes [6].
Polyps in CCS patients can develop throughout the gastrointestinal tract (except in the oesophagus) and are usually non-neoplastic hamartomas. The pathology of these polyps is similar to that of juvenile or inflammatory type polyps but marked by striking stromal oedema and eosinophilic inflammation [9]. The index patient had similar histopathology. Adenomatous polyps may occasionally develop in CCS patients which are precursor lesions to colorectal cancer [10]. The most common sites for malignancy are the sigmoid colon and rectum [11].
Common complications are gastrointestinal bleeding with anaemia, malabsorption, and rectal prolapsed [5,12]. The index patient had gastrointestinal bleeding with anaemia. Some uncommon complications and concomitant diseases have been noted: recurrent severe acute pancreatitis, myelodysplastic syndrome, cecal intussusception, portal thrombosis, and membranous glomerulonephritis [13-16].
The significant risk of colorectal cancer (around 25%) may warrant aggressive screening in CCS patients. Due to the rarity of the disease, optimal screening protocols have not been developed, although annual endoscopic surveillance has been widely practiced [9].
Differential diagnosis includes a number of polyposis syndromes, including familial adenomatous polyposis, Peutz-Jeghers syndrome, Cowden disease, and juvenile polyposis. CCS is differentiated from other hamartomatous polyposis syndromes by its widespread polyp distribution in the stomach, small bowel, and colon and sparing of oesophagus [17]. Typical endoscopic and clinico-pathologic features including extra-intestinal manifestations of CCS help in its distinction [5].
Optimum therapy for CCS is not known but several treatment options have been described. CSS therapies have included corticosteroids for treatment of protein-losing enteropathy, weight loss, and diarrhea; nonsteroidal anti-inflammatory drugs for suppression of polyps; and proton pump inhibitors for suppression of acid [18]. Combination therapy based on nutritional support including TPN and corticosteroids appears to lessen symptoms. The total treatment period is also unknown; recommendations range from 6 to 12 months of combined therapy [5,18]. The index patient was treated with sulindac, pantoprazole and prednisone which provided him significant relief
Showing hyperpigmentation in hands and feet including palmar surfaces

Showing hyperpigmentation in soles

Showing onychodystrophy in fingers

Showing onychodystrophy in toes

Showing diffuse polyposis in small intestine
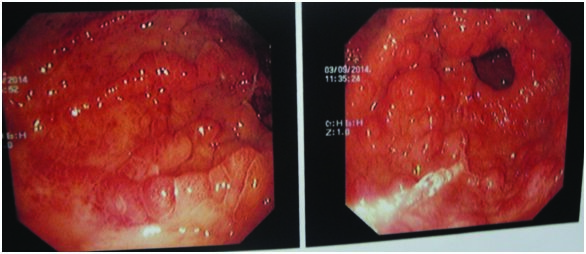
Showing diffuse polyposis in colon
Conclusion
CCS is a rare but serious disease with an increased mortality rate if not diagnosed and managed early. Delay in diagnosis are common primarily due to non-familiarity of physicians with this rare entity, leading to poor outcome. This patient presented with the cardinal manifestations of CCS which led to its early diagnosis. However, to avoid missing a diagnosis of CCS in other cases with not so florid features of CCS, it can be recommended that whenever a physician encounters an unusual number or distribution of polyps during an endoscopy during the evaluation of new onset diarrhoea and malabsorption in an elderly person, it is helpful to analyse the histopathology of the polyps and to search for the presence of characteristic dermatological changes if any.
[1]. LW Cronkhite, WJ Canada, Generalized gastrointestinal polyposis; an unusual syndrome of polyposis, pigmentation, alopecia and onychotrophiaN Engl J Med 1955 252:1011-15. [Google Scholar]
[2]. S Jarnum, H Jensen, Diffuse gastrointestinal polyposis with ectodermal changes. A case with severe malabsorption and enteric loss of plasma proteins and electrolytesGastroenterology 1966 50:107-18. [Google Scholar]
[3]. A Goto, Canada Cronkhite, Epidemiological study of 110 cases reported in JapanNippon Geka Hokan 1995 64:3-14. [Google Scholar]
[4]. S Sweetser, DA Ahlquist, NK Osborn, SO Sanderson, TC Smyrk, ST Chari, Clinicopathologic features and treatment outcomes in Cronkhite-Canada syndrome: support for autoimmunity Dig Dis Sci 2012 57(2):496-502. [Google Scholar]
[5]. S Sweetser, LA Boardman, Cronkhite-Canada syndrome: an acquired condition of gastrointestinal polyposis and dermatologic abnormalitiesGastroenterology and Hepatology 2012 8(3):201-03. [Google Scholar]
[6]. D Seshadri, N Karagiorgos, MJ Hyser, A case of Cronkhite-Canada syndrome and a review of gastrointestinal polyposis syndromesGastroenterol Hepatol (NY) 2012 8:197-2017. [Google Scholar]
[7]. SH Yun, JW Cho, JW Kim, JK Kim, MS Park, NE Lee, Cronkhite-Canada syndrome associated with serrated adenoma and malignant polyp: a case report and aliterature review of 13 cronkhite-Canada syndrome cases in KoreaClin Endosc 2013 46(3):301-05. [Google Scholar]
[8]. KT Kao, JK Patel, V Pampati, Cronkhite-Canada syndrome: a case report and review of literatureGastroenterol Res Pract 2009 2009:619378 [Google Scholar]
[9]. M Nakamura, K Kobashikawa, J Tamura, R Takaki, M Ohshiro, T Hirata, Cronkhite-Canada syndromeIntern Med 2009 48(17):1561-62. [Google Scholar]
[10]. R Malhotra, A Sheffield, Cronkhite-Canada syndrome associated with colon carcinoma and adenomatous changes in C-C polyps Am J Gastroenterol 1988 83:772-76. [Google Scholar]
[11]. J Nagata, H Kijima, K Hasumi, T Suzuki, T Shirai, T Mine, Adenocarcinoma and multiple adenomas of the large intestine, associated with Cronkhite-Canada syndromeDig Liver Dis 2003 35:434-38. [Google Scholar]
[12]. S Jarnum, H Jensen, Diffuse gastrointestinal polyposis with ectodermal changes. A case with severe malabsorption and enteric loss of plasma proteins and electrolytesGastroenterology 1966 50:107-18. [Google Scholar]
[13]. T Yasuda, T Ueda, I Matsumoto, D Shirasaka, T Nakajima, H Sawa, Cronkhite- Canada syndrome presenting as recurrent severe acute pancreatitisGastrointest Endosc 2008 67(3):570-72. [Google Scholar]
[14]. R Suzuki, A Irisawa, T Hikichi, Y Takahashi, H Kobayashi, H Kumakawa, Cronkhite-Canada syndrome associated with myelodysplastic syndromeWorld J Gastroenterol 2009 15(46):5871-74. [Google Scholar]
[15]. E Ishikawa, M Kudo, Y Minami, K Ueshima, S Kitai, K Ueda, Cecal intussusception in an adult with Cronkhite-Canada syndrome relieved by colonoscopyIntern Med 2010 49(12):1123-16. [Google Scholar]
[16]. Y Takeuchi, M Yoshikawa, N Tsukamoto, A Shiroi, Y Hoshida, Y Enomoto, Cronkhite- Canada syndrome with colon cancer, portal thrombosis, high titer of antinuclear antibodies, and membranous glomerulonephritisJ Gastroenterol 2003 38(8):791-95. [Google Scholar]
[17]. AP Burke, LH Sobin, The pathology of Cronkhite-Canada polyps. A comparison to juvenile polyposisAm J SurgPathol 1989 13:940-16. [Google Scholar]
[18]. EM Ward, HC Wolfsen, Pharmacological management of Cronkhite-Canada syndromeExpert OpinPharmacother 2003 4:385-89. [Google Scholar]