Introduction: To study the incidence of hearing loss among children and to determine and confirm the distribution of common risk factors in children with hearing loss presenting at a tertiary care hospital in India.
Materials and Methods: Babies underwent hearing screening using Transient Evoked Otoacoustic Emission (TEOAE) and Automated Auditory Brainstem Response (AABR) from November 2009 to September 2011. It was a cross-sectional study carried out at our institute involving 500 babies (≤2 y). To identify the high risk babies, Joint Committee on Infant Hearing (2007) High risk registry was used.
Results: In our study 110 (22%) babies belonged to high risk category and 11(2.2%) of total screened babies had significant hearing loss. Total number of babies who passed the initial screening with TEOAE was 284 (56.8%). On diagnostic AABR screening of TEOAE REFERRED babies, the babies with no risk factor showed normal AABR tracings whereas from among those with one or multiple risk factors (110 babies), 11(10%) showed different levels of hearing impairment. Hearing loss was highly associated with Neonatal Intensive Care Unit (NICU) admission i.e. 8/11(72.7%), followed by Low Birth Weight (LBW) and hypoxia (6/11 i.e. 54.5% each).
Conclusion: Hearing loss is more common in those babies with risk factors (majority being NICU admission, LBW and hypoxia). OAE and ABR screening of infants at risk for significant hearing loss is a clinically efficient and cost effective approach for early detection of significant hearing loss.
Introduction
Hearing is one of the very important five senses. Normal speech and language development depend upon a child’s ability to hear spoken language. Early infancy is the most appropriate time for a child to acquire the foundation of language and communication. The most important period for language and speech development is generally regarded as the first three years of life. Therefore, early detection and early identification of hearing loss is very important. This should be followed by a timely and effective therapeutic intervention and rehabilitation programs to minimize the negative effects of hearing loss on the development of cognitive, psychosocial and verbal communication skills and social interactions. Early intervention by hearing rehabilitation contributes to positive outcomes in language development. Children undergoing hearing rehabilitation before 11 months of age have a stronger vocabulary and verbal reasoning skills at 5 years of age than those intervened later [1] . Different studies have indicated that early identification followed by proper intervention as early as six months of age results in essentially normal language acquisition later on and minimizes the negative effects of hearing loss [2,3] . In contrast, a delay in detection of up to 2 to 4 years may result in delayed language acquisition. As per World Health Organisation (WHO) Hearing impairment is the inability to hear as well as someone with normal hearing in one or both ears. It can be graded as no, slight, moderate, severe or profound impairment. The World Health Organisation (2005) estimates that 278 million people worldwide have disabling hearing impairment and two-thirds of these people live in developing countries of which about 50 percent can be prevented [4] . As per WHO (2003), Indian population has a disabling hearing impairment prevalence of approximately 6.3% (63 million) with children (up to 14 years) accounting for a major part of it [5] . As per National Sample Survey Organisation [NSSO], 2002, 291 persons per 100,000 Indian population were suffering from severe to profound hearing impairment [6] . Many more have rma4mild hearing difficulties. Hearing loss in newborns and infants are not readily detectable by routine clinical procedures (behavioural observation), although parents often report the suspicion of hearing loss, inattention, or erratic response to sound before hearing loss is confirmed [7] . For the past 20 y, electrophysiological methods are most commonly used which include otoacoustic emission (OAE) which is generated by the biological activity of the outer hair cells of the cochlea and auditory brain stem response (ABR) which is the representation of electrical activity generated by the eighth cranial nerve and brainstem in response to auditory stimulation during first 10 milliseconds. Regardless of the screening method chosen, hearing screening, though critical, is only the first stage of a comprehensive early intervention plan. Screening alone is useless unless appropriate diagnostic testing services and high quality amplification and rehabilitation services are in place and are implemented in a timely fashion. Early screening does not substitute for further periodic childhood hearing screening.
Materials and Methods
The present study “Hearing screening in a tertiary care hospital in India” was carried out in Department of Otorhinolaryngology, Department of Paediatrics (NICU and Paediatric wards) and Department of Obstetrics and Gynaecology, Byramjee Jeejeebhoy Medical College (BJMC) and Hospital, Ahmedabad. The study was a cross-sectional study which involved 500 babies (≤2 y) who underwent hearing screening from November 2009 to September 2011. The aims and objectives was to study the incidence of hearing loss among children (≤2 y),determine and confirm the distribution of common risk factors in children with hearing loss and identify children with possible hearing deficits at the earliest possible stage in order to refer for diagnosis, treatment and rehabilitation, if required. Informed consent was obtained from parents prior to the study. Babies included in the study were those admitted in NICU, babies (≤ 2 y) admitted in paediatric ward, those visiting the Outpatient department and desiring hearing assessment and babies born in the department of Obstetrics and Gynaecology with high risk factors. We excluded babies with active ear discharge / infection by otoscopy and those with associated external ear pathologies in whom ear plug cannot be applied by Bull’s lamp examination. The High Risk criteria are based on the set criteria by the Joint Committee on Infant Hearing (2007) and American Academy of Paediatrics (1994) which included the following [8] :
• Family history of hereditary childhood sensorineural hearing loss.
• In utero infections such as toxoplasmosis, cytomegalovirus, rubella, herpes simplex and syphilis.
• Craniofacial anomalies including those with morphologic abnormalities of the pinna and ear canal.
• Birth weight less than 1500 g.
• Hyperbilirubinemia at serum level requiring exchange transfusion.
• Ototoxic medication.
• Bacterial meningitis.
• Postnatal asphyxia (Apgar ≤5 at 1 min or ≤ 6 at 5 min).
• Mechanical ventilation lasting 5 days or longer.
• Stigmata or other findings associated with syndrome known to include a sensorineural and or conductive hearing loss (National Institutes of Health-NIH, statement 1993).
The screening procedure was done in a sound treated room in the department or in a quiet room adjacent to the respective wards of concerned departments. The Instruments used were Otoacoustic Emission Screener (Emissia, RMS, India) and Auditory Brainstem Response Audiometer (Medulla AD, RMS, India). A 2-stage screening protocol was used which consisted of a preliminary screening with Transient evoked OAE (TEOAE). Participants who were referred during first screening with TEOAE were subjected to further screening with AABR to confirm the presence of hearing loss. All attempts were made to screen the child without sedation, however when participants were not co-operative they were sedated with Syrup Triclofos (Pedicloryl; Dr. Reddy’s Laboratories Ltd., Hyderabad, India) for AABR after obtaining written consent from the parents. The study was approved by the Ethics committee of BJMC and Hospital, Ahmedabad, Gujarat (India). Data was compiled in Microsoft excel 2007 (Microsoft Office 2007; Microsoft, United States) and analysed using SPSS version 20 (IBM Inc., New York, United States). Percentages and proportions were calculated and depicted using bar diagrams.
Results
In our study, the maximum numbers of infants 224 (44.8%) were in the age group of 0-6 months. On primary screening by TEOAE, 284 (56.8%) babies passed. Amongst the remaining 43.2% who had TEOAE REFER, 11.2% and 32% of babies had unilateral and bilateral hearing loss respectively. We had 410 (82%) term infants, of which 76.34 % (313/410) had normal delivery and 23.65% (97/410) had caesarean delivery. The TEOAE REFER was 34.18% and 34.02% respectively in babies with normal and caesarean delivery (CS).
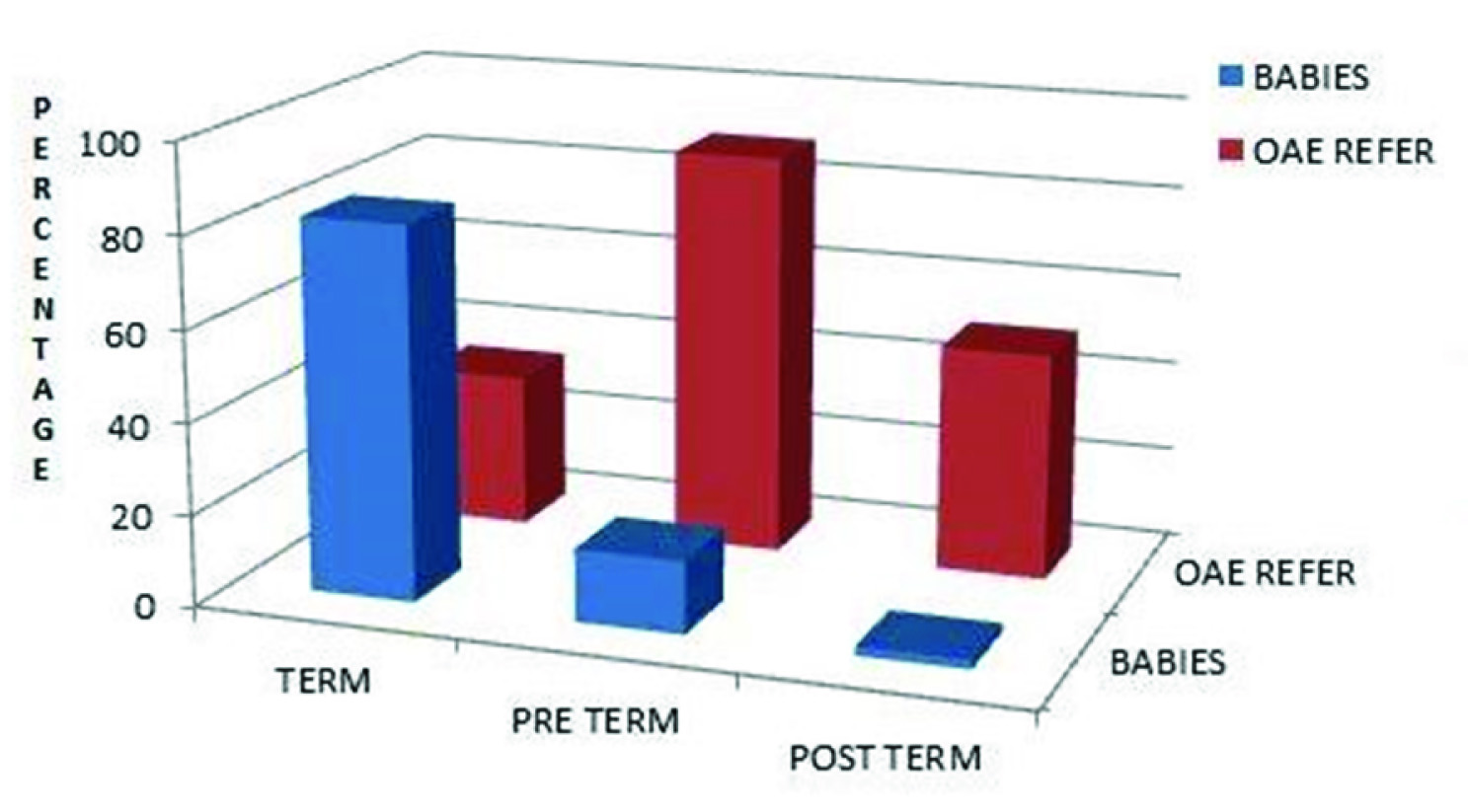
Among term infants 34.1% had OAE REFER. However, in preterm babies (all were LBW and delivered by caesarean section), the TEOAE REFER on primary screening was seen in 88.75% (71/80), whereas in post term (all delivered by CS) the TEOAE REFER was 50% (5/10) [Table/Fig-1].
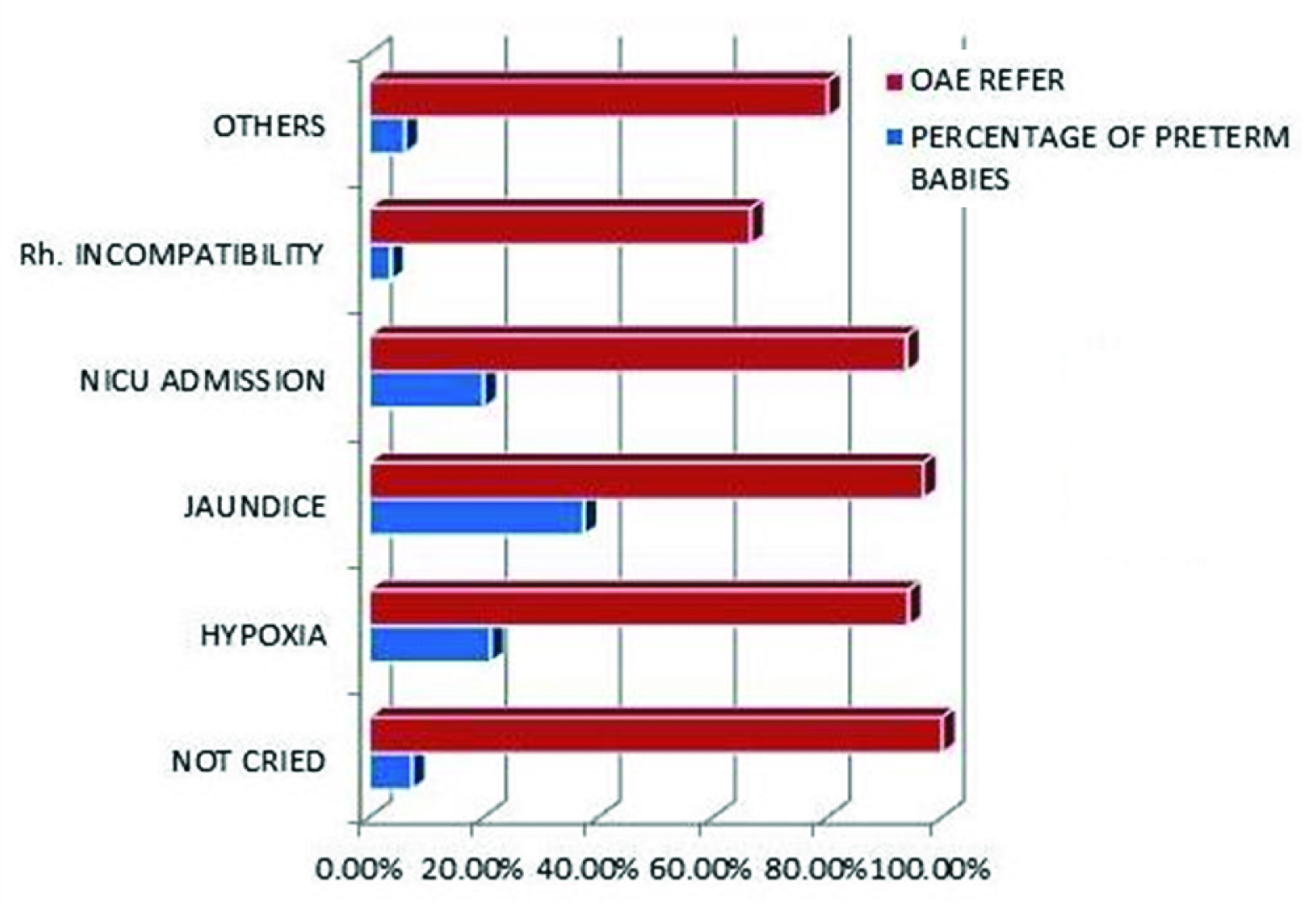
Most number of risk factors was associated with preterm babies. Of the 6 preterm babies who did not cry at birth, all 6 had TEOAE REFER on primary screening. Jaundice accounted for 37.5% (30/80) of cases among preterm of which 96.7% (29/30) showed TEOAE REFER. Hypoxia and NICU admission accounted for 21.75% (17/80) and 20% (16/80) of cases respectively of which TEOAE REFER was 94.1% (16/17) and 93.75% (15/16) respectively. Association of hearing loss with NICU admission in our study after primary screening with TEOAE was 93.75% (15/16). Less common risk factors viz. Rh incompatibility and CNS abnormalities accounted for 3.75% (3/80) and 6.25% (5/80) of total preterm babies of which 66.6% (2/3) and 80% (4/5) showed TEOAE REFER on primary screening respectively [Table/Fig-2].
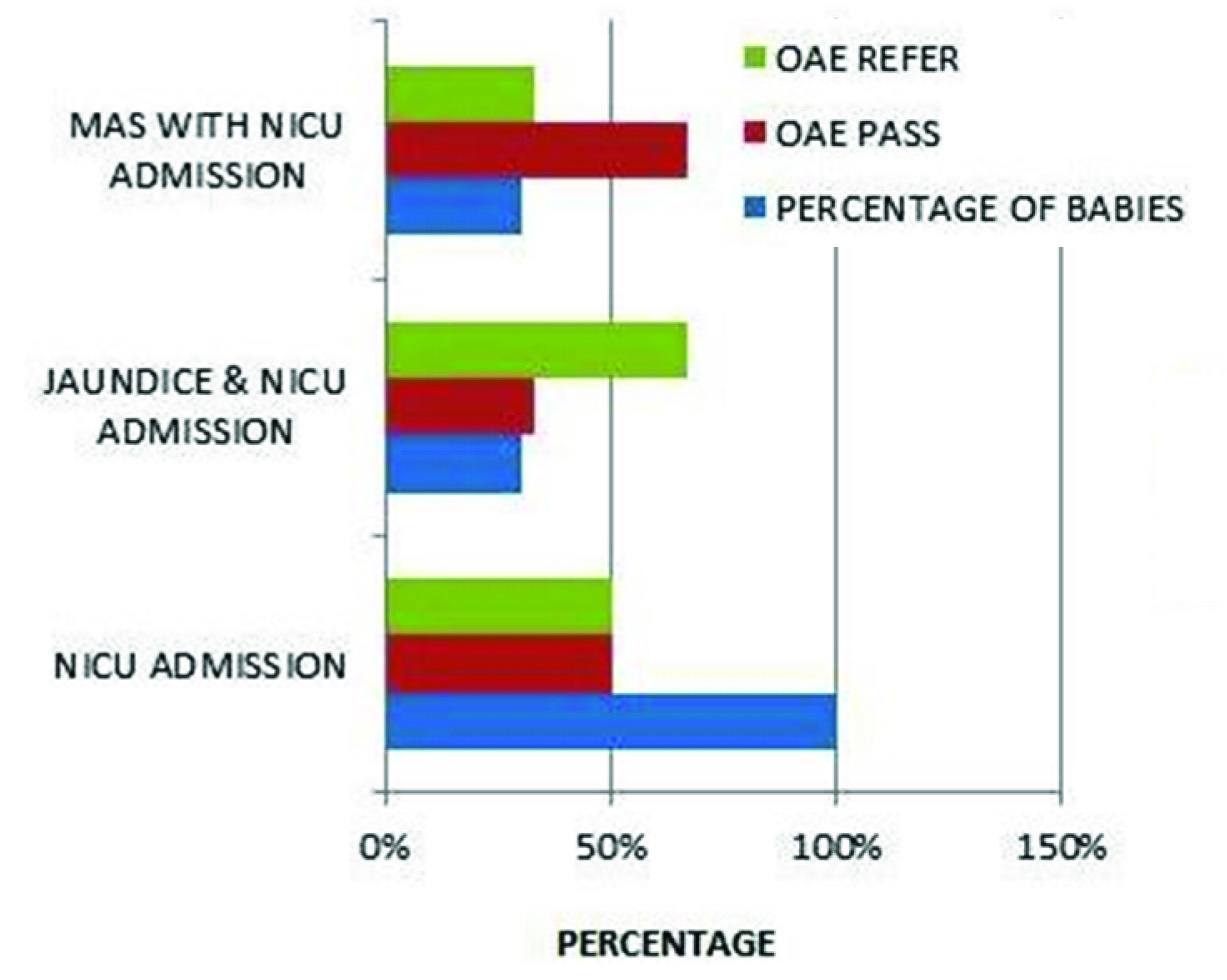
In post term babies, all were admitted in NICU, of which 50% (5/10) had TEOAE REFER on primary screening. However, out of 3 post term babies who were admitted in NICU following an attack of jaundice, 2 had TEOAE REFER. With these findings it is apparent (albeit with a small data) that association of multiple risk factors in a newborn increase the risk of hearing loss. Paradoxically, out of 3 post term babies who were admitted to NICU following Meconium Aspiration Syndrome (MAS), only 1 baby had TEOAE REFER on primary screening; this might be attributable to the relative small number of babies with MAS in my study [Table/Fig-3].
Among the risk factors associated with full term babies, Rh incompatibility was not associated with hearing loss whereas use of ototoxic drugs and Central Nervous System (CNS) affection resulted in 66.6% (4/6) TEOAE REFER respectively. Half (50%) of babies born to mother with previous miscarriage in association to Rh incompatibility showed TEOAE REFER on primary screening. Similar numbers (55%) of babies were referred on primary screening when mother had previous miscarriage without Rh incompatibility.
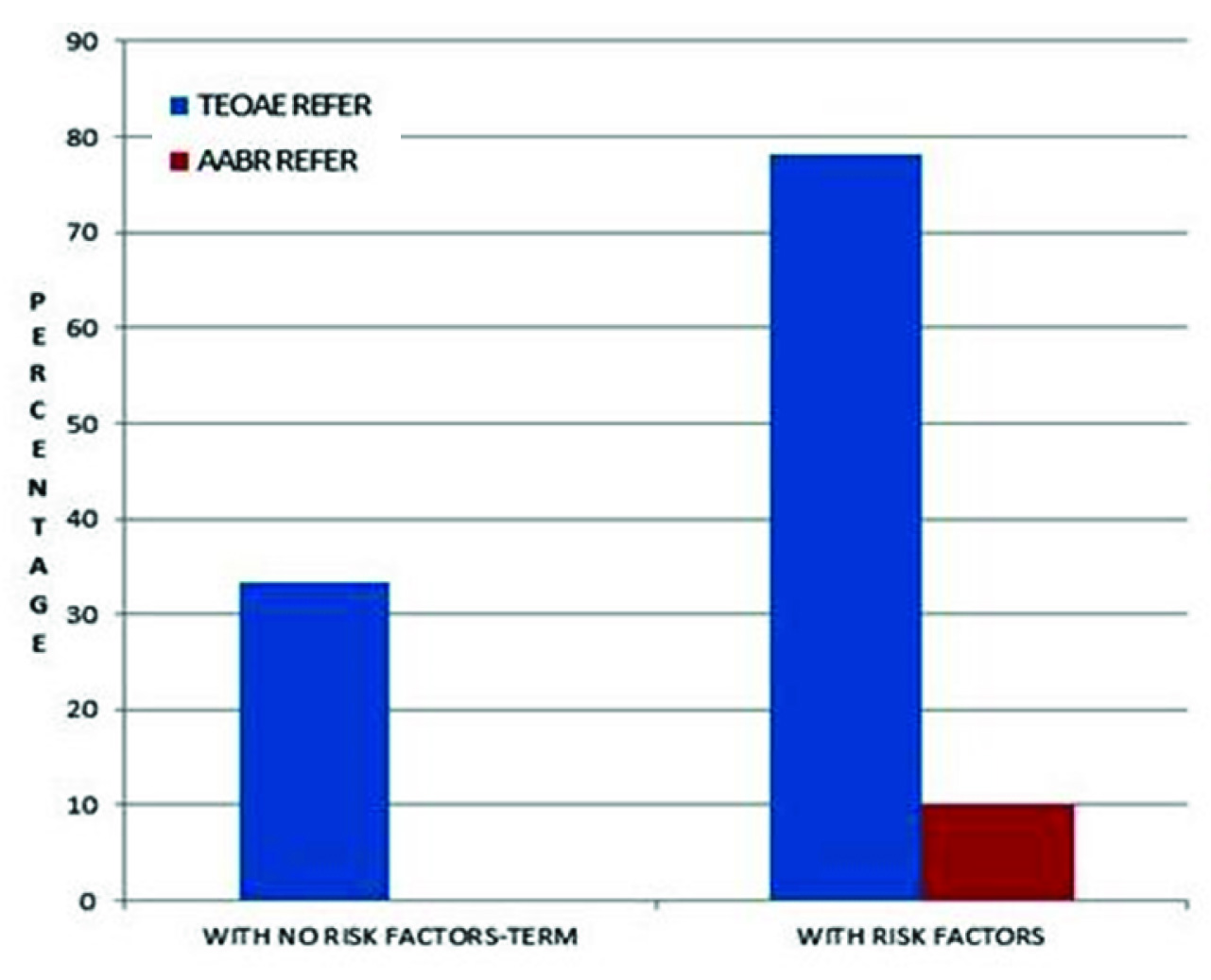
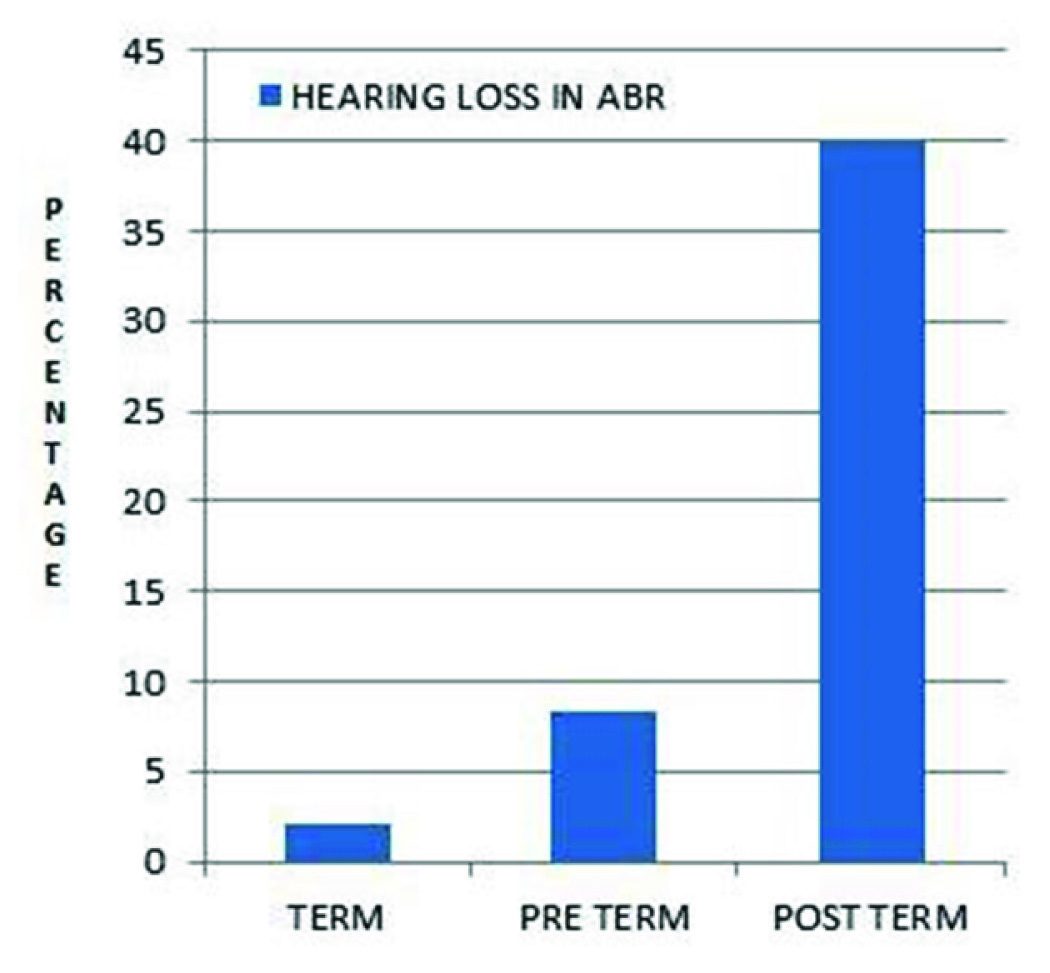
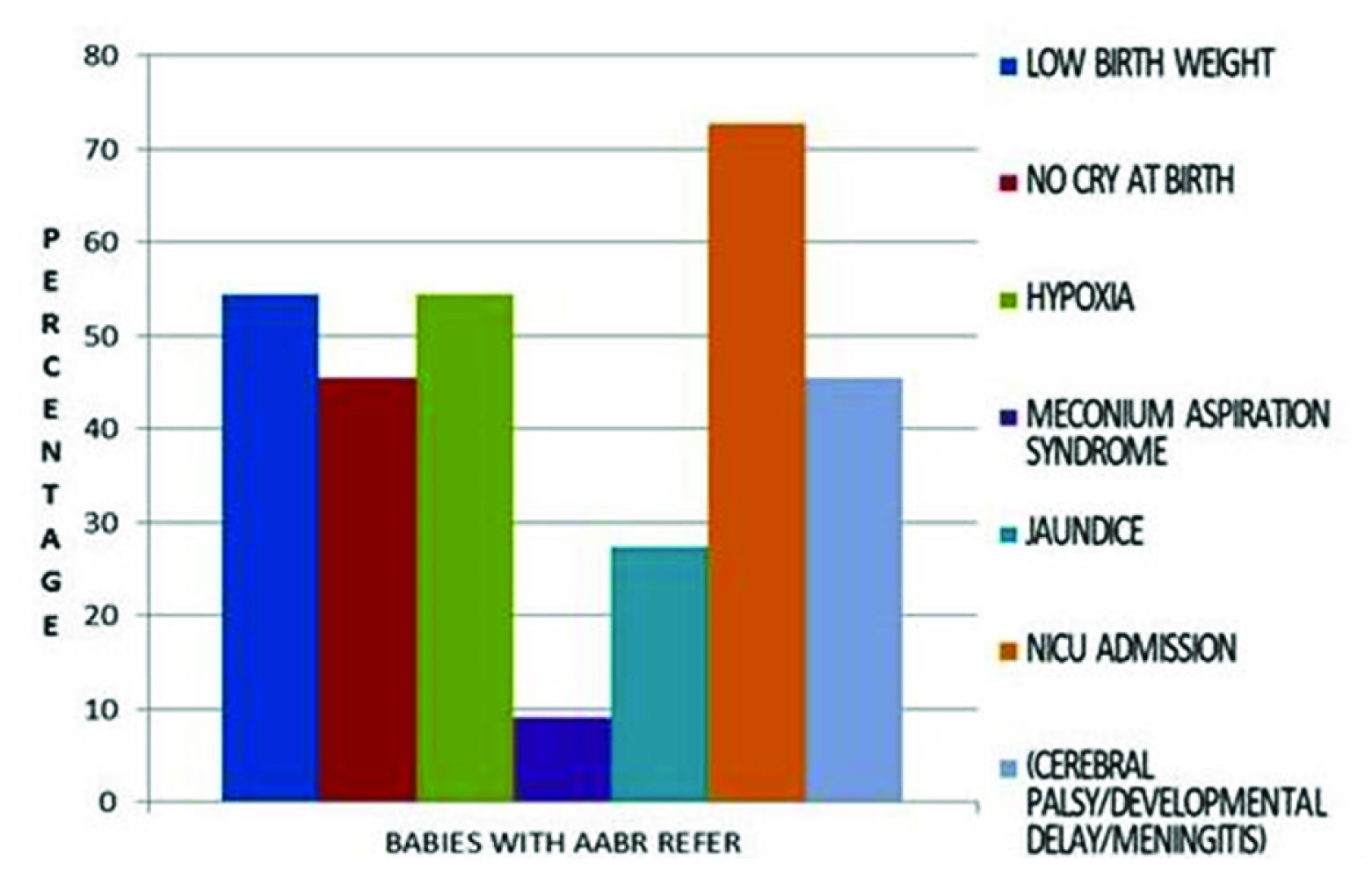
Screening with AABR audiometry was done on all the TEOAE REFER babies. Babies with no risk factors showed normal hearing sensitivity whereas amongst those with associated risk factor 78.18% (86/110) were REFERRED on primary TEOAE screening, and following AABR, 10% (11/110) of babies had REFER result [Table/Fig-4]. In regards to gestational age at birth, hearing loss was seen in 2.14%, 8.4% and 40% respectively for term, preterm and post term babies [Table/Fig-5]. Evidently in our study of Hearing loss when associated with high risk factors, the highest incidence was seen with newborns admitted to NICU (72%), followed by LBW and hypoxia (54.5% in each), no cry at birth and others- cerebral palsy, developmental delay, meningitis (45.5% each) and jaundice (27.3%). MAS showed the least association (9% - mostly due to very low number of MAS babies) [Table/Fig-6].
Discussion
In the age group of 0-6 months, the total screened babies were 44.8% which is desirable but the goal should be to screen 100% children by this age to enable further investigations and interventions in selected cases. There are authors who however screen infants varying between before 3 months of age and others who screen children within five years of age [9-11] . The majority (74%) of the babies who had TEOAE REFER had bilateral hearing loss. A particular study done at Surat showed 24.6% with bilateral hearing loss [11] . The result was comparable to a series by Mehl and Thomson [12] which showed 71% bilateral involvement. Method of delivery (uncomplicated and without any associated risk factor) bore little effect on the incidence of hearing loss. Overall, 22% (110/500) of screened babies had one or multiple risk factors whereas hearing loss was detected in 2.2% (11/500) of the total 500 screened babies. In one series, 54% of screened babies belonged to high risk category and 0.09% of total screened babies had some level of hearing impairment [9] . Another series from Singapore detected hearing loss of varying level in 0.18% of the total screened babies and 38% belonged to the high risk category [7] . Similar results were demonstrated by Mehl and Thomson who reported incidence rate of 0.19% and 47% babies had associated risk factors [12] .
In Connolly, Mississippi, USA study 1.3% of total high risk babies screened were detected with hearing loss [13] . In my study 10% of total high risk babies screened were detected with hearing loss (AABR REFER).
Among TEOAE REFFERED babies with history of NICU admission who were subjected to further investigation using ABR, 53.3 % (8/15) cases had hearing loss. The result was slightly lower when compared to a series by Dalzell et al., [14] which showed presence of hearing impairment in 61% babies who were admitted in NICU.
The reason for the relatively higher incidence of hearing impairment in our study may have been due to inclusion of children up to two years of age.
Incidence of OAE referral in babies depending on maturity at birth
Association of various risk factors woth OAE referral in pre-term babies (100% lbw); “Others” include cerebral palsy, developmental delay and meningitis
Association of various risk factors with OAE referral in post term babies
Comparing TEOAE and AABR results in babies (<2 years) having no risk factors with those having one or more risk factors for hearing loss
Gestational age and hearing loss in ABR
AABR result in TEOAE referred babies (<2 years) and its association with various risk factors of hearing loss
Conclusion
In this era of technology reliable screening tools can be used for early identification of hearing loss in children. The audiologist can get valuable information about hearing loss by OAE and ABR testing and an infant born with a hearing loss could experience normal speech and language development as a result of early intervention.
It can be safely concluded from our study that:
• Hearing loss is more common in those babies with risk factors and there is a relationship between having risk factor(s) for 3hearing loss, not passing a hearing screen, and then later having a confirmed hearing loss.
• Major risk factors are NICU admission, LBW, hypoxia and jaundice.
• Auditory brainstem response hearing screening of infants at risk for significant hearing loss (after initial screening with OAE) is a clinically efficient and cost effective approach to early detection of significant hearing loss as all babies diagnosed with hearing loss following ABR screening had associated high risk factors.
• A follow-up study on those babies that passed their initial screen, but have one or more risk factors for hearing loss would be useful in determining how many cases of progressive hearing loss occur with that particular population.
Recommended Prevention Strategies
• Improving antenatal and perinatal care;
• Avoiding the use of ototoxic drugs unless prescribed by a qualified health care worker and properly monitored for correct dosage;
• Referring jaundiced babies for diagnosis and possible treatment;
• Immunizing children against childhood diseases, including measles, meningitis, rubella and mumps;
• Immunizing women of child-bearing age against rubella before pregnancy;
• Screening and treating syphilis and certain other infections in pregnant women;
• Reducing exposure (both occupational and recreational) to loud noises by using personal protective devices and by engineering noise control.
• Educating the Paediatricians and Gynaecologists regarding early identification of high risk babies and their prompt referral for hearing assessment.
Acknowledgement
To all the patients and their parents who have participated in our study.
Proforma (Used for the Study)
SERIAL NO.: DATE:
NAME: AGE: SEX:
FATHER’S NAME: ADDRESS:
MEDICAL HISTORY
Prenatal History
History of miscarriage; Use of medication; Viral infection; Other illnesses; X-Ray exposure; Others.
Birth History
Premature delivery; Post term delivery; Labour: - Normal, Prolonged,
Instrumental delivery; Caesarean delivery; Birth injuries; Birth weight;
Birth cry.
Hypoxia; Jaundice (in 1st 4-5 days); Rh incompatibility; History of NICU admission; Apgar score: at 1 minute and 5 minutes.
Family History
Local Examination
Ear: RIGHT LEFT
Pre auricular region
Post auricular region
Pinna
EAC
Tympanic Membrane
Nose:
Throat:
SCREENING RESULT
OAE: REFFER/ PASS
BERA: ADVISED/ NOT ADVISED
BERA – Result (If Advised)
[1]. MP Moeller, Early Intervention and Language Development in Children Who Are Deaf and Hard of HearingPediatrics 2000 106(3):e43-52. [Google Scholar]
[2]. C Yoshinaga-Itano, AL Sedey, BA Coulter, AL Mehl, Language of early- and lateridentified children with hearing lossPediatrics 1998 102:1168-71. [Google Scholar]
[3]. R Gopal, SR Hugo, B Louw, Identification and follow-up of children with hearing loss in Mauritius Int J Pediatr Otorhinolaryngol 2001 57(2):99-113. [Google Scholar]
[4]. World Health Organization. Fact sheet. Deafness and hearing impairment. Available at http://www.who.int/mediacentre/factsheets/fs300/en/index.html (accessed on 20 September 2014) [Google Scholar]
[5]. S Garg, S Chadha, S Malhotra, AK Agarwal, Deafness: burden, prevention and control in IndiaNatl Med J India 2009 22(2):79-81. [Google Scholar]
[6]. National Sample Survey Organization.Disabled persons in India, NSS 58th round (July–December 2002) Report no. 485 (58/26/1).New Delhi:National Sample Survey Organization, Ministry of Statistics and Programme Implementation, Government of India, 2003 [Google Scholar]
[7]. KH Arehart, C Yoshinaga-Itano, V Thomson, SA Gabbard, SA Brown, State of the States: The status of universal newborn screening, assessment, and intervention systems in 16 StatesAmerican Journal of Audiology 1998 7:101-14. [Google Scholar]
[8]. Joint Committee on infant hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programsPediatrics 2007 120:898-921.http://dx.doi.org/10.1542/peds.2007-2333 [Google Scholar]
[9]. K Uus, J Bamford, Effectiveness of population based newborn hearing screening in England: Ages of interventions and profile of casesPediatrics 2006 117(5):e887-93. [Google Scholar]
[10]. R Joseph, HK Tan, KT Low, Mass newborn screening for hearing impairmentSoutheast Asian J Trop Med Public Health 2003 34(Suppl 3):229-30. [Google Scholar]
[11]. JA Contractor, PM Vaghmashi, RB Patel, IM Chaudhari, DA Barot, N Jariwala, A study of oto-acoustic emission (OAE) in 130 cases: a screening tool for hearing loss in childrenJournal of otorhinolaryngology and Head and Neck Surgery 2011 8(1):11-13. [Google Scholar]
[12]. AL Mehl, V Thomson, The Colorado newborn hearing screening project, 1992- 1999: On the threshold of effective population-based universal newborn hearing screeningPediatrics 2002 109(1):e7 [Google Scholar]
[13]. JL Connolly, JD Carron, SD Roark, Universal newborn hearing screening: are we achieving the Joint Committee on Infant Hearing (JCIH) objectives?Laryngoscope 2005 115(2):232-36. [Google Scholar]
[14]. L Dalzell, M Orlando, M MacDonald, The New York State universal newborn hearing screening demonstration project: Ages of hearing loss identification, hearing aid fitting, and enrolment in early interventionEar Hearing 2000 21(2):118-30. [Google Scholar]