Familial Adenomatous Polyposis (FAP)—A Case Study and Review of Literature
Santosh Bhimrao Dalavi1, Tanwar Harshwardhan Vedpalsingh2, Sanket Subhash Bankar3, Mohd Hamid Shafique Ahmed4, Dattatray Nivrutti Bhosale5
1Associate Professor, Department of Surgery, Government Medical College, Miraj, Mharashtra, India.
2Ex-Registrar, Department of Surgery, Government Medical College, Miraj, Mharashtra, India.
3Ex-Registrar, Department of Surgery, Government Medical College, Miraj, Mharashtra, India.
4Assistant Professor, Department of Surgery, Government Medical College, Miraj, Mharashtra, India.
5Assistant Professor, Department of Surgery, Government Medical College, Miraj, Mharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanket Subhash Bankar, Ex-Registrar, Department of Surgery, Government Medical College, Miraj-416416, Maharashtra, India.
E-mail: sanketbankar23@gmail.com
Familial adenomatous polyposis (FAP) is a syndrome characteristically having numerous (hundreds to thousands) polyps in the epithelium of the large intestines with an autosomal dominant inheritance caused by germ line mutations in adenomatous polyposis coli (APC) gene in chromosome 5q21. Most FAP patients have a family history of colorectal polyps and cancer but 25-30% of them are "de novo", without any clinical or genetic evidence of FAP in family members. Prophylactic proctocolectomy is required in almost all patients since all affected patients inevitably develop cancer. We report a case of a 32-year-old man who presented with vague abdominal complaints without any family history, which on evaluation as found to have multiple colorectal polyps and underwent a prophylactic proctocolectomy with end continent ileostomy. Two of his children were evaluated and found to have multiple colorectal polyps on colonoscopy and have been advised regular follow up annually. In conclusion, patients with FAP may present with vague abdominal complaints and without any family history, hence need to be carefully evaluated. Good patient compliance is of prime importance in deciding the treatment and surveillance modality subsequently determining the prognosis of patients with FAP.
Colonoscopy, Colorectal polyps, Proctocolectomy
Case Report
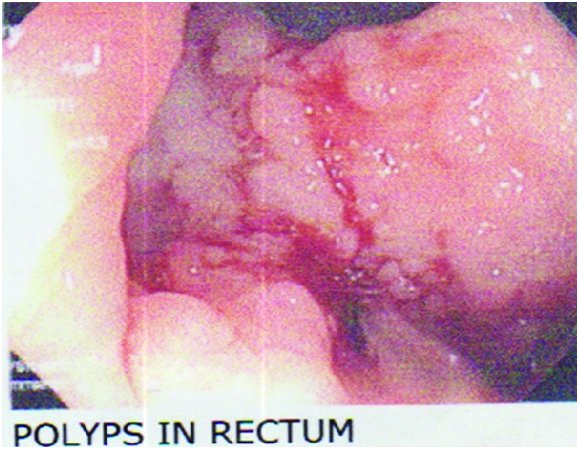
A 32-year-old man, farmer by occupation, presented with altered bowel habits, decreased appetite, intermittent per rectal bleed and increased flatulence since six months. No other family members had similar health complaints. On digital rectal examination (DRE), a polypoidal mass was felt at fingertip on posterior rectal wall approximately 6cm from anal verge. On proctoscopy there were numerous small polyps surrounding the large polyp circumferentially. No haemorrhoids or any rectal ulcer was noted. His blood investigations were within normal limits. On contrast enhanced computerized tomographic (CECT) scan of abdomen showed a 4.6cmx 3.3cmx 4.3cm enhancing polypoidal mass in distal transverse colon. The sub mucosal region in vicinity also showed early enhancement. Rest of the colon had patchy nodular areas. On colonoscopy, polyps of more than 1cm size were seen over entire rectum up to anal canal [Table/Fig-1]. Multiple biopsies were taken. Splenic flexure, transverse colon, hepatic flexure, ascending colon and caecum also showed multiple polyps. biopsies were taken.
Terminal ileum had normal mucosa. Histopathological reports (HPRs) of biopsies revealed tubular adenomas in transverse colon and rectum with no evidence of dysplasia or malignancy.
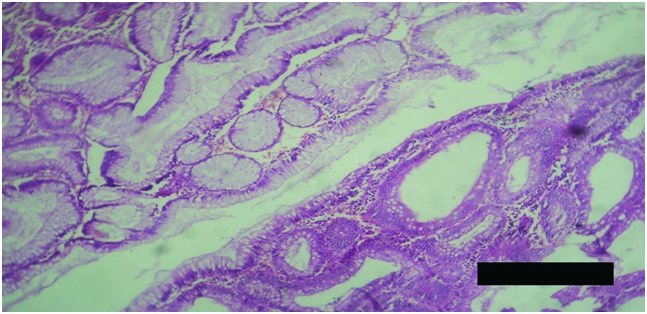
Patient was investigated for FAP associated lesions and no other significant finding was noted except on fundoscopy there were early changes of Congenital hypertrophy of retinal pigment epithelium (CHRPE). Patient was planned for prophylactic total anoproctocolectomy. Patients consent was obtained for surgical management and permanent ileostomy was opted by the patient and the patient was subsequently operated and recovered well. The proctocolectomy specimen showed multiple polyps [Table/Fig-2]. HPR confirmed the presence of multiple tubular adenomas with no evidence of dysplasia or malignancy [Table/Fig-3]. Screening was done for his 7year and 10 year old male children by colonoscopy, which revealed multiple polyps in the entire colon up to caecum of both the screened members. HPR of Multiple colonoscopic biopsies were suggestive of multiple tubular adenomas with no dysplasia or malignant transformation. The children have been advised regular follow-up with annual sigmoidoscopy.
Discussion
FAP is a syndrome characteristically having numerous (hundreds to thousands) polyps in the epithelium of the large intestines with an autosomal dominant inheritance caused by germ line mutations in APC gene in chromosome 5q21 [1]. Its prevalence being 3–10/100,000, affecting both sexes equally, with development of symptoms by the late teens and in the twenties. Most FAP patients have a family history of colorectal polyps and cancer but 25-30% of them are "de novo", without any clinical or genetic evidence of FAP in family members [2]. Patient’s family history was insignificant. Majority of the patients develop polyps in the childhood, which gradually increase in size and number throughout the colon until adolescence. Nearly fifty percent of patients develop adenomas by the age of 15 years and 95% by the age of 35 years. Malignancy begins to develop approximately 10 years after the appearance of polyps [3]. Other common clinical features in patients with FAP include multiple gastric fundic gland polyps, duodenal, periampullar or ampullar adenomas, while extra intestinal features are desmoid tumours, congenital hypertrophy of the retinal pigment epithelium (CHRPE), epidermoid cysts, osteomas and thyroid cancer [4]. This patient had CHRPE.
Prophylactic surgery is recommended before the age of 25years. The main surgical options for patients with FAP are (1) total proctocolectomy with Brooke ileostomy; (2) subtotal colectomy with ileorectal anastomosis, and (3) restorative proctocolectomy with the formation of an ileal reservoir and ileoanal anastomosis. The decision to remove the rectum depend upon the number of rectal polyps and the family history. For few polyps in the rectum, total colectomy with ileorectal anastomosis is recommended. In rectal involvement, a restorative proctocolectomy with ileal pouch-anal anastomosis is the treatment of choice [5]. Prophylactic surgery improves the outcome of patients with FAP significantly and it is recommended in late teens or early twenties [6]. The risk of developing rectal adenomas and carcinomas after ileorectal anastomosis is approximately 13 to 59%, after 25 years mandating a lifelong rectal surveillance [5]. Proctocolectomy with pouch formation and ileoanal anastomosis is the preferred surgical procedure as it completely removes large bowel mucosa as potential site for origin of cancer, minimizing the risk of malignancy and also preserving the bowel function [7]. Patients undergoing proctocolectomy, an annual endoscopic surveillance of the pouch and transitional anal zone is important because premalignant changes and invasive adenocarcinomas are found in the ileoanal pouch after restorative proctocolectomy [8]. Because of reluctance of the patient for further surveillance, patient opted for a permanent ileostomy. The American Gastroenterology Association recommends annual sigmoidoscopy in patients with classic FAP and at-risk relatives starting at the age of 10-12 years. Patients with adenomatous polyps found on sigmoidoscopy require a full colonoscopy and biopsy [9]. Use of nonsteroidal antiinflammatory drugs such as sulindac for primary treatment of FAP is not supported and prophylactic colectomy remains the treatment of choice to prevent colorectal cancer in patients with FAP [10]. Both children of this patient were advised annual sigmoidoscopy.
Colonoscopic image showing Polyps in the rectum
Multiple polyps in proctocolectomy specimen

Histopathology report:Tubular adenomas
Conclusion
Patients with FAP may present with vague abdominal complaints and without any family history, hence need to be carefully evaluated. Good patient compliance is of prime importance in deciding the treatment and surveillance modality subsequently determining the prognosis of patients with FAP.
[1]. SQ Matsumoto, SQ Lida, SQ Kobori, SQ Mizuno, SQ Nakamura, SQ Hizawa, Genetic predisposition to clinical manifestations in familial adenomatous polyposis with special reference to duodenal lesionsAm J Gastroenterol 2002 97:180-85. [Google Scholar]
[2]. E Half, D Bercovich, P Rozen, Familial adenomatous polyposisOrphanet J Rare Dis 2009 4:22 [Google Scholar]
[3]. GM Petersen, J Slack, Y Nakamurass, Screening guidelines and premorbid diagnosis of familial adenomatous polyposis using linkageGastroenterology 1991 100:1658-64. [Google Scholar]
[4]. DA Anaya, GJ Chang, MA Rodriguez-Bigas, Extracolonic manifestations of hereditary colorectal cancer syndromes Clin Colon Rectal Surg 2008 21:263-372. [Google Scholar]
[5]. O Aziz, T Athanasiou, VW Fazio, RJ Nicholls, AW Darzi, J Church, Metaanalysis of observational studies of ileorectal versus ileal pouch-anal anastomosis for familial adenomatous polyposisBr J Surg 2006 93(4):407-17. [Google Scholar]
[6]. RKS Phillips, AD Spigelman, Can we safely delay or avoid prophylactic colectomy in familial adenomatous polyposis?Br J Surg 1996 83:769-70. [Google Scholar]
[7]. AJ Campbell, RAJ Spence, TG Park, Familial adenomatous polyposisBr J Surg 1994 81:1722-33. [Google Scholar]
[8]. DP Hurlstone, BP Saunders, JM Church, Endoscopic surveillance of the ileoanal pouch following restorative proctocolectomy for familial adenomatous polyposisEndoscopy 2008 40:437-42. [Google Scholar]
[9]. S Winawer, Gastrointestinal Consortium Panel. Colorectal cancer screening and surveillance: clinical guidelines and rationale – update based on newevidenceGastroenterology 2003 124(2):544-60. [Google Scholar]
[10]. FM Giardiello, Primary chemoprevention of familial adenomatous polyposis with sulindac N Engl J Med 2002 346(14):1054-59. [Google Scholar]