A Rare Case of Mixed Connective Tissue Disease (MCTD) with Intricate Features of Lupus, Polymyositis and Rheumatoid Arthritis Presenting with Severe Myositis
Lokesh S1, Kadavanu Tony2, Raghupathy3, Suresh V4, Balakrishna Malepati5
1Associate Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, SBV University, Pillayarkuppam, Puducherry, India.
2Resident, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, SBV University, Pillayarkuppam, Puducherry, India.
3Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, SBV University, Pillayarkuppam, Puducherry, India.
4Resident, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, SBV University, Pillayarkuppam, Puducherry, India.
5Resident, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, SBV University, Pillayarkuppam, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lokesh. S, No.11, Veeramamunivar Street, Dr. Radhakrishnan Nagar, Puducherry-605009, India.
E-mail: lokeshs@mgmcri.ac.in
Mixed connective tissue disease (MCTD) includes clinical and laboratorial manifestations of systemic lupus erythematosus, scleroderma and polymyositis along with high titres of anti-U1RNP antibodies. In the initial phases of the disease, muscle enzyme levels increase but the disease remains generally subclinical. Presentation with myositis is uncommon. Our objective is to report a rare case of a patient who presented with a severe onset of myositis characterized by dysphagia, an increase in myopathy and joint involvement suggestive of RA. The patient was initiated on pulse corticosteroid therapy along with methotrexate in view of her elevated Creatine Kinase levels and biopsy findings that were suggestive of severe myositis. The patient showed clinical and laboratory improvement with this regimen. Though severe myositis and arthritis can occur in overlap syndrome, MCTD evolved as a separate disease entity due to presence of high titres of Anti U1-RNP antibodies. The authors emphasize that this is an extremely rare presentation of MCTD with only two previous cases seen in literature, one of a 13 year old child and the other being an adult female both of whom had evidence of myositis on presentation.
Dysphagia, Methotrexate, Muscle, Myopathy
Case Report
A 52-year-old lady presented with complaints of multiple joint pain since two years and pain in both her lower limbs for six months. She also complained of difficulty in swallowing, recurrent oral ulcers for three months. She had symmetrical joint involvement with the small joints of her hand being involved initially with early morning joint stiffness lasting for at least one hour. She had been prescribed analgesics and steroids on multiple occasions for the same. Her symptoms worsened over a period of one year when she started noticing pain at her wrist and ankle joints along with swelling of her fingers. For last six months she had difficulty in getting up from squatting position and had pain in her thigh muscles. However, she managed to walk without any support. She also had difficulty in swallowing in the past three months, for both solid and liquid feeds. There was no history of skin rashes/photosensitivity/recurrent genital ulcers. She was a known diabetic on oral hypoglycaemic agents. There was no past history of hypertension or seizures. There was no family history of similar complaints, diabetes mellitus, hypertension, epilepsy or asthma.
Examination revealed that she had pallor and angular stomatitis was present along with multiple oral ulcers. She had difficulty in opening her mouth completely and her parotid glands were bilaterally enlarged [Table/Fig-1]. She had hyperpigmentation of both palms and she had pitting pedal edema bilaterally. The fingers showed spindle shaped deformity affecting proximal interphalangeal joints and there was swelling of the metacarpophalangeal joints also. Her pulse was 90/min, regular, normal volume, normal character with no vessel wall thickening and her B.P was 140/ 90 mmHg.
During systemic examination, diffuse tenderness was present over both thighs (L>R), with power of 4+/5 in both lower limb (proximal group). Power in all other group of muscles was 5/5. Reflexes were normal. Rest of the systems was within normal limits. A clinical diagnosis of probable MCTD with varied severity of polymyositis, rheumatoid arthritis and Systemic Lupus Erythematosis was made and further investigated.
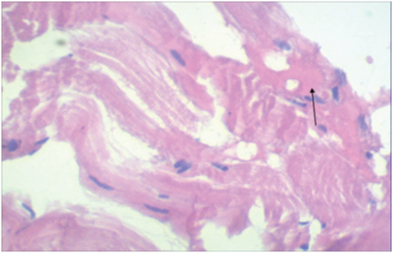
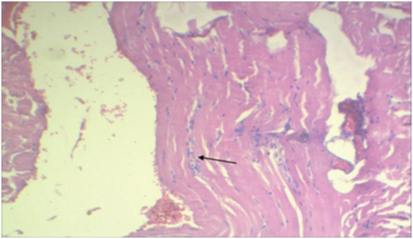
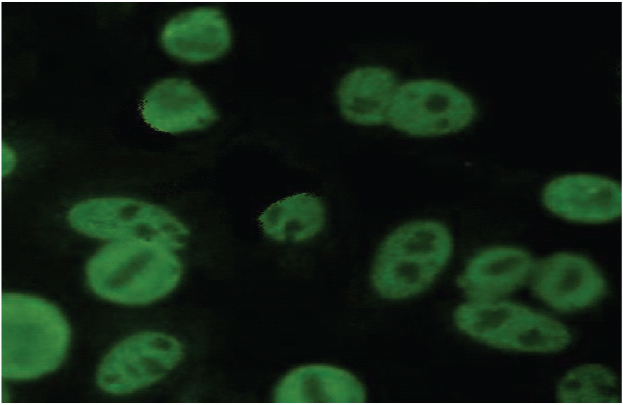
An upper gastrointestinal endoscopy, a barium swallow and a schirmer's test were done which were normal. The proximal symmetric muscle force was shown to be classified as grade II. The investigation results are shown in [Table/Fig-2]. Imaging of the hands showed juxta articular osteopenia suggestive of RA [Table/Fig-3]. A muscle biopsy [Table/Fig-4,5,6] was subsequently taken from left thigh which revealed myonecrosis along with an inflammatory infiltrate in the regions surrounding the normal muscle fibers. Positive antinuclear antibodies having a speckled pattern [Table/Fig-6] were in a titre of 1:118.85. However, the anti-Jo-1, anti-Sm, anti dsDNA, anti-Scl70 and anti-centromere autoantibodies were all negative. Also, serological tests for infectious diseases, including HIV, hepatitis B and C, toxoplasmosis and cytomegalovirus, were all negative. A final diagnosis of MCTD was made.
Pulse therapy was administered with methylprednisolone (1g/day for three days) in view of biopsy findings of myonecrosis and elevated creatinine levels, which resulted in clinical improvement and led to a decrease in the Creatine Kinase level to 512 U/L. Methotrexate was also administered at a concentration of 15 mg/wk and after two months of treatment the patient was characterized by muscle force grade IV and a Creatine Kinase level of 214 U/L. Since last eight months, with the last follow up a month ago patient is asymptomatic with normal muscle strength and Creatine Kinase level of 65 U/L, while continuing treatment on low dose methotrexate (7.5 mg) and prednisolone.
Discussion
In the present study, we have described a rare case of one female patient with MCTD who presented initially with severe myositis. Nearly 60% of patients who have inflammatory myositis present with subclinical myopathy [1] . However, one can achieve quick clinical and laboratory response with low dose corticosteroids [2] .
Contrary to the initial expectations, our patient presented with severe myositis with muscle necrosis on biopsy and elevated creatine kinase levels. It was this observation that made us initiate treatment with high dose corticosteroids and methotrexate.
Our patient had fulfilled the international diagnostic requirements proposed by Kasukawa [Table/Fig-7] for MCTD, after excluding other infectious diseases via serologic tests and after ensuring there was no history of any myotoxic drug intake.
Nearly 72% of patients with MCTD have a subclinical increase in muscle enzyme levels of which, only 2–3% of patients present with myositis in the initial stages. Although 51% of patients eventually develop subclinical myositis, approximatelyonly 6% continue to actively present the symptoms of myositis. When noticeable, these symptoms resemble other inflammatory myopathies, albeit with milder manifestations that can easily be treated with lowto- moderate doses of corticosteroids. Gutierrez et al., [3] had described the association of dysphagia in patients with MCTD and myositis which is mainly due to the involvement of the esophageal striated muscle.
A role of vascular pathology has been suggested in the myositis that is associated with MCTD owing to certain reports demonstrating a reduction in the number of blood vessels and a thickening of the endothelial layer along with a perivascular inflammatory infiltrate. A similar reduction in blood vessel number is seen in the initial phase of dermatomyositis [4,5] . This reduction is seen following deposition of the membrane attack complex of the complement system on blood vessel membranes. The vascular involvement associated with the deposition of immunoglobulin was reported more than 20 y ago in some patients with MCTD where the proliferative vascular lesions were found to have a thicker intimal and medial layer secondary to an inflammatory cell infiltrate [4-6] .
In the literature only one previous report was found that described a severe and refractory case of myositis in an adult with MCTD [7] . Another report [8] described the case of a 13-year-old child with MCTD who presented with muscle weakness and an elevated level of CK and had features on muscle biopsy and electromyography analysis suggestive of severe myositis. Both the cases had high titres of Anti U1-RNP antibodies.
A retrospective review of 174 patients with SLE over 15 y period revealed SLE/myositis overlap syndrome among six patients. All six patients were women and had symmetric proximal muscle weakness. The muscle disease was severe in one case. The muscle biopsy revealed an inflammatory myopathy change [9] . A similar myositis picture was observed in our patient.
In a study on scleroderma overlap syndrome, out of 165 Systemic Sclerosis (SSC) patients, 40 (24.3%) fulfilled the criteria of overlap syndrome. Other connective tissue disorder observed with overlap syndrome was DM/PM in 19 patients, Sjogren’s syndrome in 17 patients, RA in six patients and SLE in two patients. There were three patients with high titres of Anti U1-RNP with signs of SLE, Myositis and SSC who were labelled to have MCTD [10] .
Picture showing bilateral parotid enlargement

| Investigation | Value | Reference Range |
|---|
| Creatine Kinase | 2350 U/L | 26-192 U/L |
| AST | 108 U/L | <31 U/L |
| ALT | 210 U/L | <31 U/L |
| LDH | 786 U/L | 240-480 U/L |
| Aldolase | 42 U/L | < 7.6 U/L |
| ANA | 118.85 eu/ml | <25 eu/ml |
| RF | 256 IU/ml | |
| U1nRNP | 1686 | |
| CRP | 9.6 mg/dl | |
X ray of hands showing juxta articular osteopenia

Muscle biopsy showing areas of muscle necrosis
Muscle biopsy image showing dense leucocytic infiltrates
Slide showing ANA in speckled pattern
Diagnostic Criteria for MCTD
| Kasukawa | Common symptoms | Mixed Symptoms | Requirements for diagnosis |
|---|
| 1. Raynaud’s phenomenon | 1. SLE-like symptoms:i. Polyarthritis ii. Pericarditis or Pleuritis iii. Facial erythema iv. Leukothrombocytopenia v. Lymphadenopathy.
| At least 1 of 2 common symptoms plus positive for anti-RNP plus 1 more of the mixed symptoms in at least 2 of the 3 disease categories. |
| 2. Swollen fingers or hands Anti-RNP antibody positive | 2. Scleroderma-like findings:i. Sclerodactyly ii. Hypomotility or dilatation of esophagus. iii. Pulmonary fibrosis, restrictive changes of lung,or reduced diffusion capacity
| |
| | 3. Polymyositis-like findings:i. Muscle weakness ii. Myogenic pattern on EMG iii. Eleveated serum levels of muscle enzymes (CPK)
| |
Conclusion
This work has reported an extremely rare case of an adult patientwith MCTD characterized by a severe myositis and high titres of AntiU1-RNP levels at presentation that was effectively treated after the administration of high doses of corticosteroids, and methotrexate.
[1]. R Kasukawa, Mixed connective tissue diseaseIntern Med 1999 38:386-93. [Google Scholar]
[2]. I Lundberg, E Hedfors, Clinical course of patients with anti-RNP antibodies. A prospective study of 32 patientsJournal of Rheumatology 1991 18:1511-19. [Google Scholar]
[3]. F Gutierrez, JE Valenzuela, GR Ehresmann, FP Quismorio, RC Kitridou, Esophageal dysfunction in patients with mixedconnective tissue diseases and systemic lupus erythematosusDigestive Diseases and Sciences 1982 27:592-97. [Google Scholar]
[4]. MA Viana, C Borges, EF Borba, MT Caleiro, E Bonfa, S Marie, Myositis in mixed connective tissue disease: A unique syndrome characterized by immunohistopathologic elements of both polymyositis and dermatomyositisArqNeuropsiquiatric 2004 62:923-34. [Google Scholar]
[5]. JR Mendell, TS Garcha, JT Kissel, The immunopathogenic role of complement in human muscle diseaseCurr Opin Neurol 1996 9:226-34. [Google Scholar]
[6]. BH Singsen, VL Swanson, BH Bernstein, A histologic evaluation of mixed connective tissue disease in childhoodAm J Med 1980 68:710-17. [Google Scholar]
[7]. C Bonin, Silva B Santos Pires Da, Mota L, Carvalho J De, Severe and Refractory Myositis in Mixed Connective Tissue Disease: A Description of a Rare CaseLupus 2010 19:1659-61. [Google Scholar]
[8]. S Nakata, K Uematsu, T Mori, Effective treatment with low- dose methotrexate pulses of a child of mixed connective tissue disease with severe myositis refractory to corticosteroidNihon Rinsho Meneki Gakkai Kaishi 1997 20:178-83. [Google Scholar]
[9]. Maazoun Fatma, Frikha Faten, Snoussi Mouna, Kaddour Neila, Hatemmasmoudi Bahloul Zouhir, Systemic lupus erythematosusmyositis overlap syndrome: report of 6 casesClin Pract 2011 1(4):e89 [Google Scholar]
[10]. Balbir-Gurman Alexandra, Braun-Moscovici Yolanda, Scleroderma overlap syndromeIMAJ 2011 13:14-20. [Google Scholar]