Oncocytic Lipoadenoma of Submandibular Gland: A Case Report
Harshad V. Parmar1
1 Assistant Professor, Department of General Pathology, Christian Medical College, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Harshad V. Parmar, Assistant Professor, Department of General Pathology, 4th Floor, ASHA block, Christian Medical College Hospital, Ida Scudder Road, Vellore, Tamil Nadu -632004, India.
E-mail: harshadmdp@hotmail.com.
Lipomatous tumours of salivary glands are very uncommonly diagnosed and reported tumours. Majority of these tumours present as painless masses which grow slowly over many years. On the histological grounds, they can be subclassified into “monophasic” (lipoma component only) and “biphasic” (lipoma component+epithelial component) tumours. A handful of biphasic tumours contain oncocytic component and they have been omitted from the WHO classification of salivary gland tumours so far and this has remained a matter of persistent confusion and controversy over many years. Other rare variants of monophasic tumours include fibrolipoma, sialolipoma, angiolipoma, sialadenosis and very rarely a liposarcoma can also occur in salivary glands. Pre-operative imaging can help in picking up the fatty component of the tumours and guide in accurate classification. FNAC may not be accurate in diagnosis of these tumours. We report a case of 45-year-old gentleman presenting with submandibular gland swelling for which submandibular gland excision was done. A final diagnosis of oncocytic lipoadenoma was made. We present this rare entity to add to the few cases reported to date and hence, to increase recognisation and understanding of these rare tumours, which may help in establishing a reproducible subclassification. We have discussed the pathological aspects with review of literature of this very rare entity.
Benign, Salivary gland tumours, WHO
Case Report
A 45-year-old gentleman presented to ENT outpatient clinic, Christian Medical College, Vellore, India with complaints of gradually progressive, painless, left sided neck swelling since past one year. It had increased in size over the past two months. There was no history of dryness of mouth, no intraoral discharge,dysphagia, fever, loss of weight or appetite or any comorbid medical illness. Neck examination revealed a 5 x 6 cm, well-defined, mass below the left angle of mandible with smooth surface and without any scars or sinuses over it. On palpation, the inspectory findings were confirmed. The swelling was non-tender, having well-defined borders with soft to firm consistency and was not fixed to overlying skin. There were no palpable lymph nodes in the neck. There was no intraoral swelling on bimanual examination. Based on these clinical findings a clinical diagnosis of salivary gland neoplasm was made, FNAC of the swelling was done but was inadequate for proper evaluation. Other possibilities of a soft tissue tumour and rare low grade lymphoma were kept in mind. Sialography was not indicated in this case and hence it was not carried out.
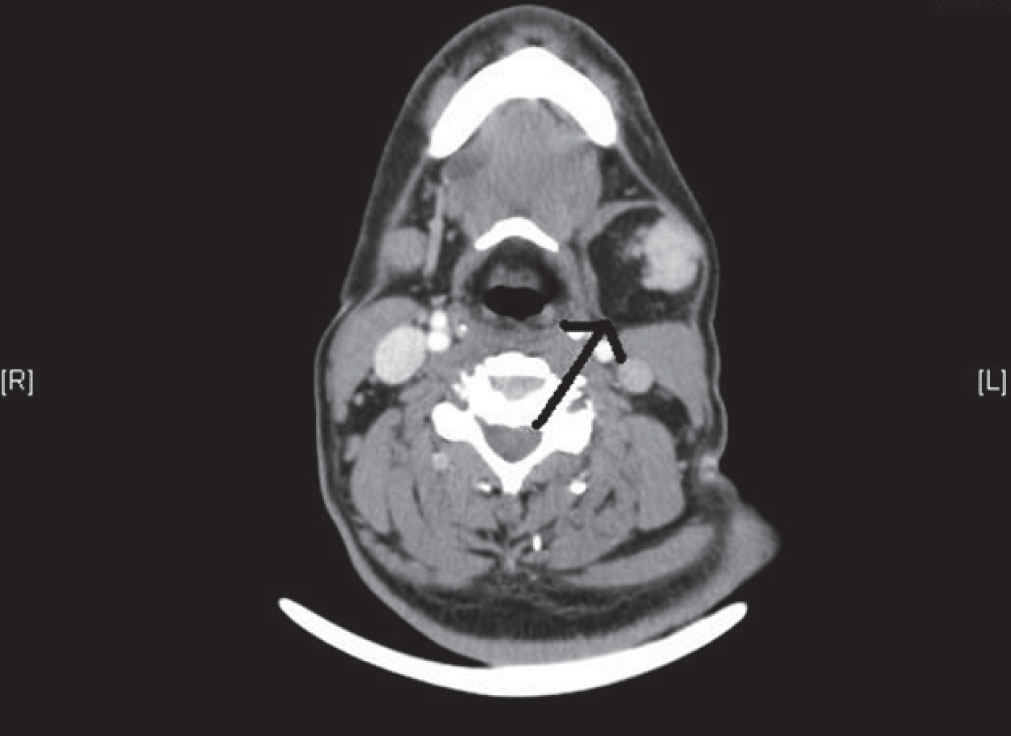
CT Findings
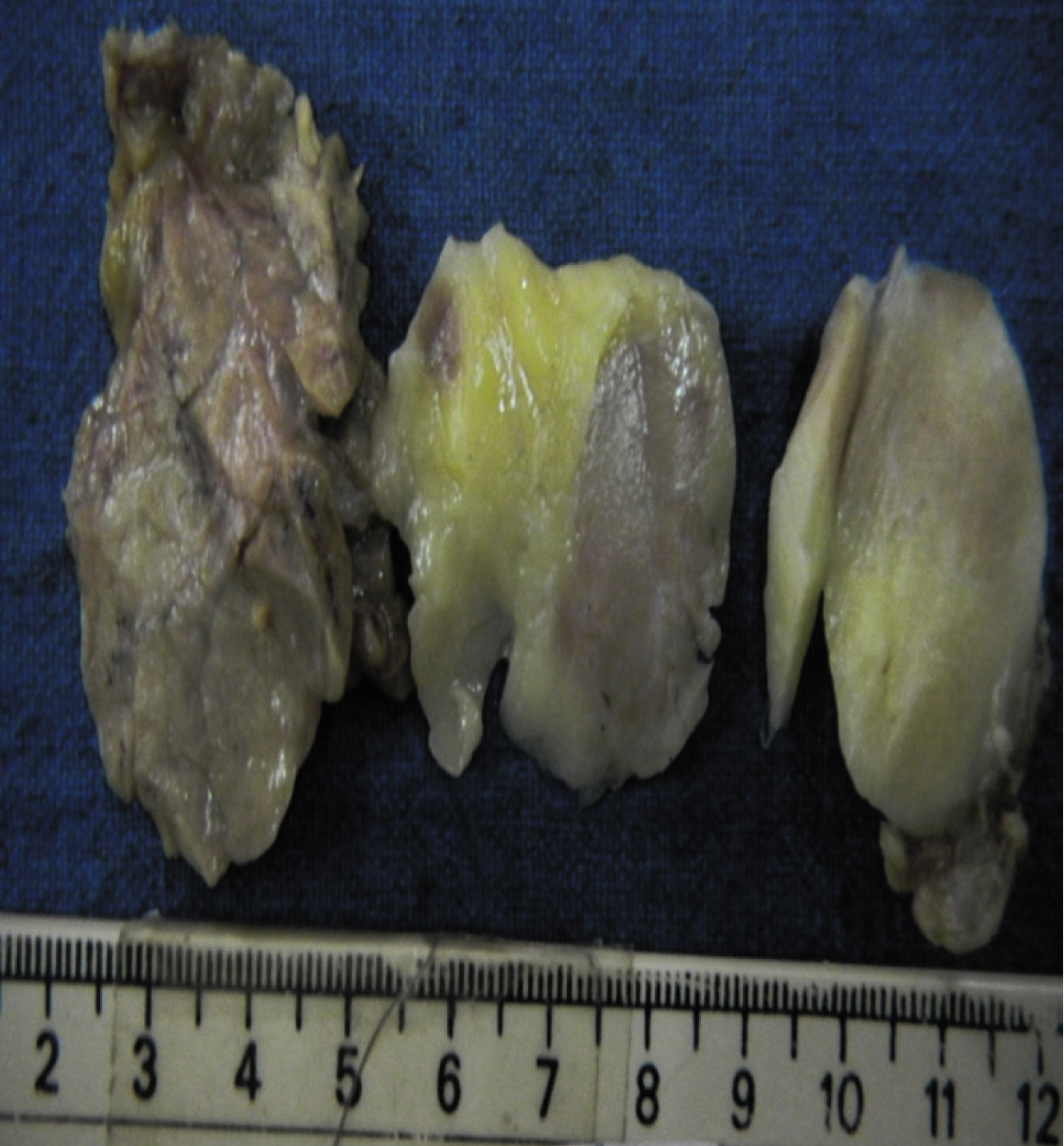
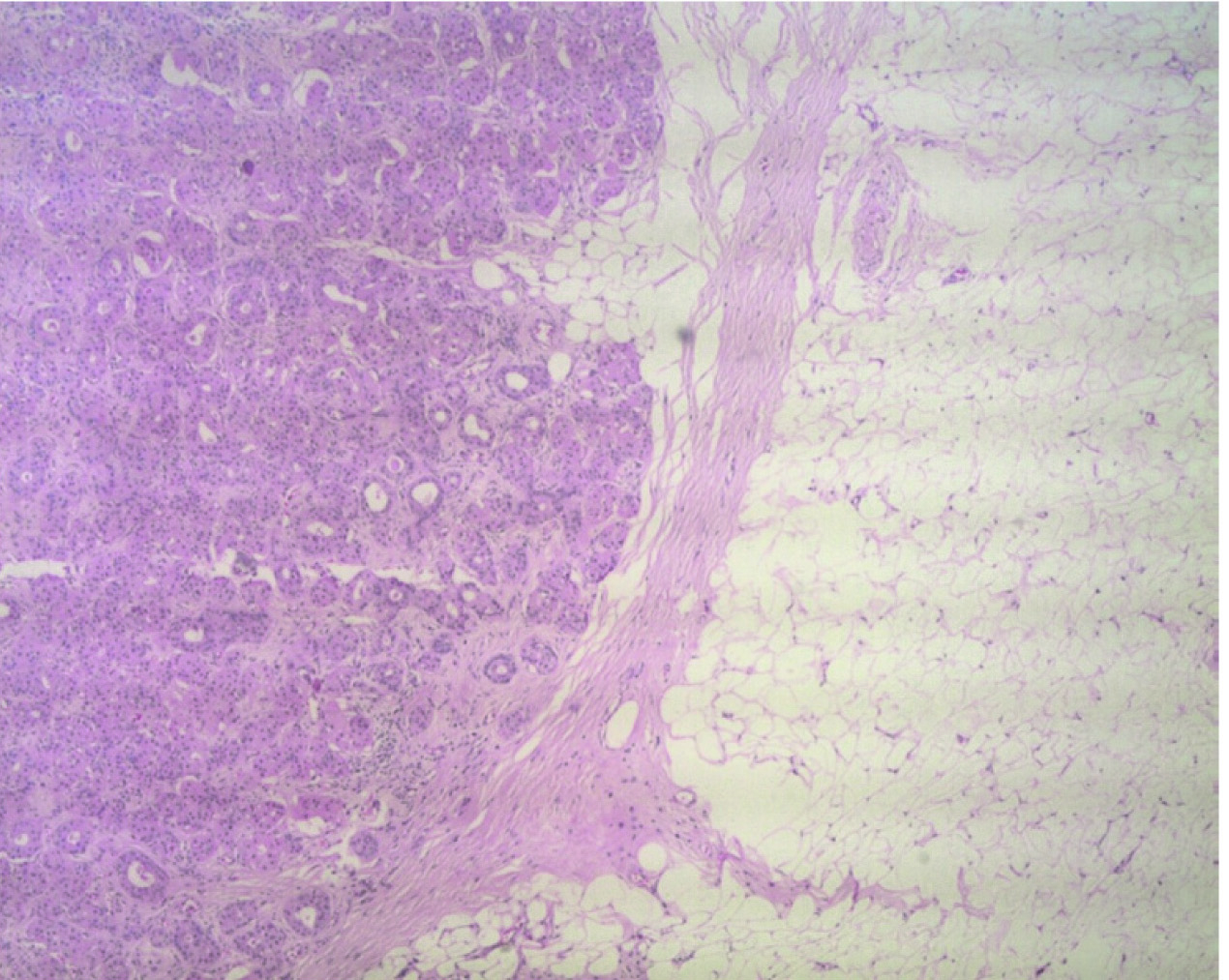
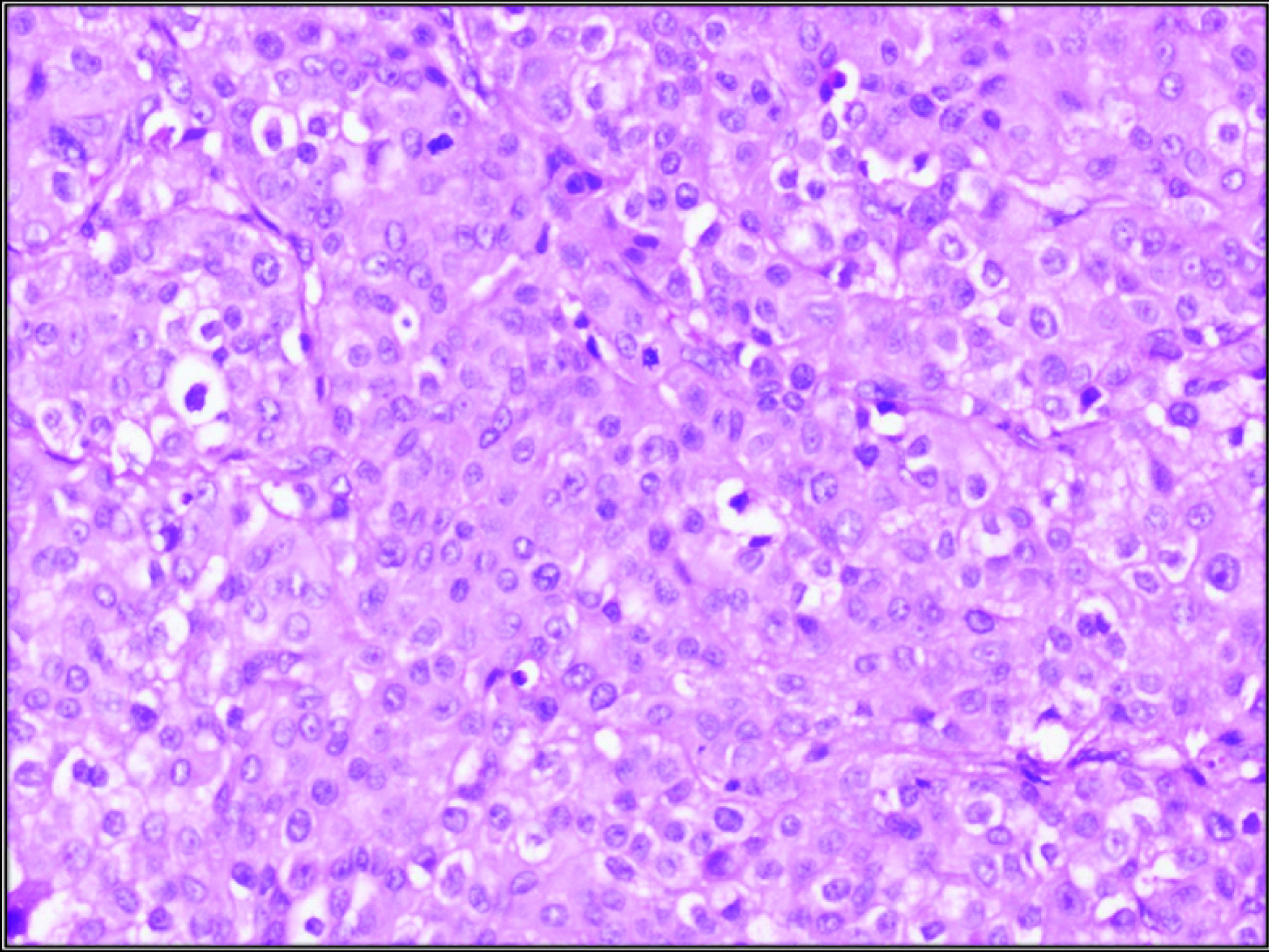
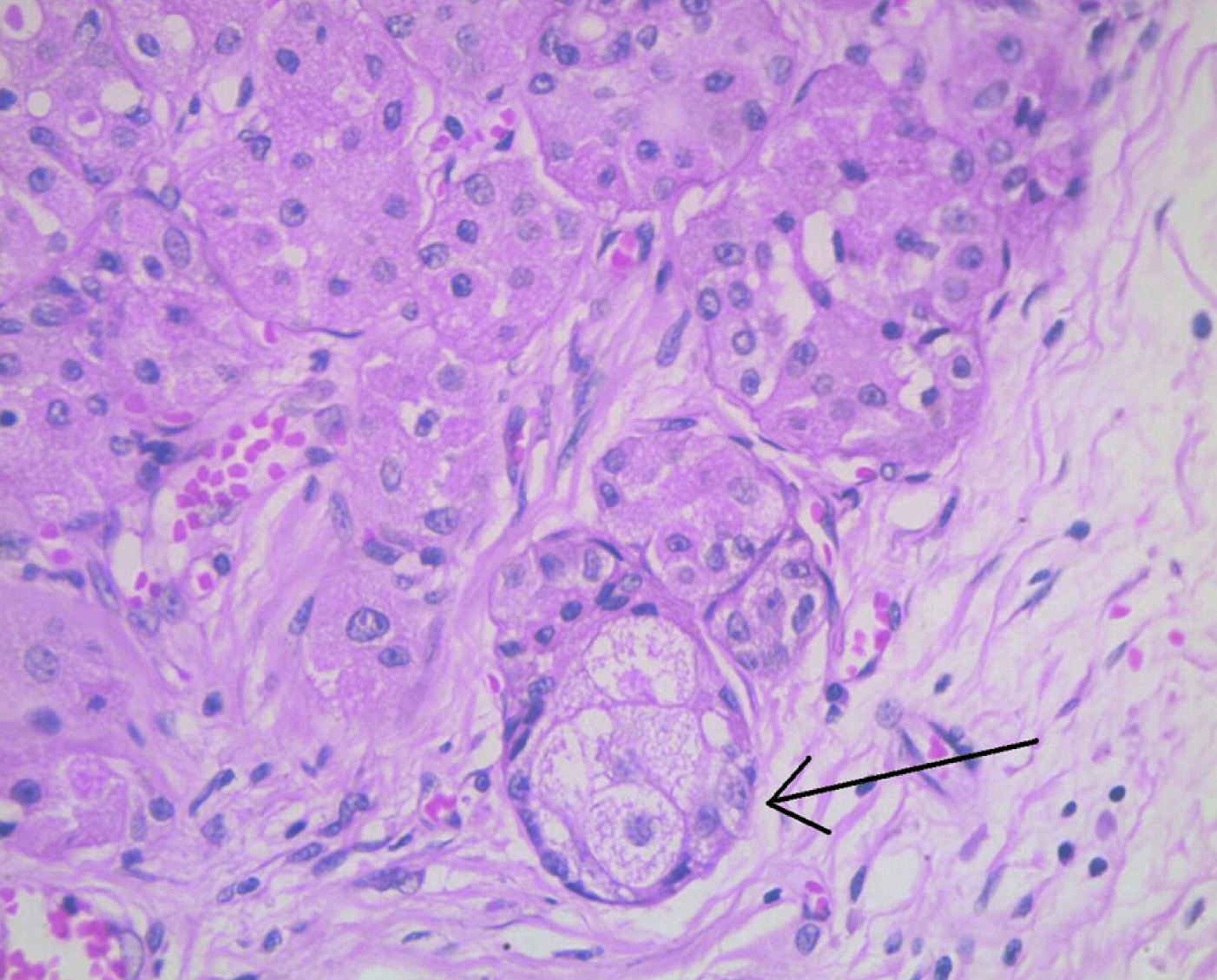
Left salivary gland was enlarged with a large fatty lesion, 55mm x 45mm x 20mm, having a large mural component. Lesion had solid component in it measuring approximately 27 x 17 mm. with a few mottled densities [Table/Fig-1]. There was no significant lymphadenopathy. Surgery was done under general anaesthesia. Patient was positioned on a shoulder roll with head tilted to right side. Painting with betadine lotion was done followed by drapping. The incision was made in the skin crease 5cm below the angle of mandible and deepened through platysma. Both superficial and deep lobes were identified with preservation of mandibular nerve and hypoglossal nerve with ligation of facial artery and facial vein. A 5 × 5 cm large mass arising from the left submandibular gland was excised and submitted for histopathological examination. After securing complete hemostasis, cervical fascia and skin flaps were sutured back in position. Grossly, the tumour was lobulated, encapsulated mass with well-defined brown areas and adjacent greasy-yellow soft areas [Table/Fig-2]. Histopathology examination revealed circumscribed tumour composed of lobules and sheets of oncocytes [Table/Fig-3,4]. Also, present were sheets and lobules of mature adipocytes, some of which are entrapped by the oncocytic nodules [Table/Fig-3,4]. There was patchy periductal chronic inflammation and fibrosis. There was focal sebaceous metaplasia at the edges of oncocytic nodules [Table/Fig-5]. There was no evidence of lymphovascular or perineurial invasion or any extra capsular invasion. Immunohistochemistry was not indicated in this case due to obvious morphological findings, which were consistent with those mentioned in the literature. On a telephonic follow up, no recurrence of symptoms so far. Patient is due for a yearly follow-up during which imaging will be carried in case there is any clinical evidence of recurrence.
CT scan image showing a lobulated fat containing lesion
Gross specimen showing lobulated tumour with grey-brown, firm oncocytic component with adjacent greasy-yellow lipomatous component
H&E stain, low power view.Oncocytic nodule on left side, lipomatous lesion on right side (10X)
H&E stain, 20x magnification showing sheets of oncocytic cells
H&E stain, 40x magnification showing focus of a sebaceous metaplasia
Discussion
Liomatous tumours are commonly seen in subcutaneous soft tissue. Salivary gland lipomatous tumours comprise about 0.5% of all salivary gland tumours [1–4]. Common sites include parotid gland followed by submandibular gland [2–4]. Most of the patients were in their middle age with a male predilection [2–4]. Lipomatous tumours can be subdivided into monophasic and biphasic subtypes. Monophasic tumours are commoner, which are well circumscribed tumours with a lipomatous component only. These tumours have identical features as soft tissue lipomas, curable by simple excision [1–4].
Biphasic/hybrid lipomatous tumours have epithelial and a lipomatous component. Epithelial component can further be classified as "oncocytic" and "non-oncocytic" component. From the published literature, it is understood that these tumours have variable histological features. The difficulty in the subclassification of these tumours may be due to the reasons that a lipomatous component may be present in pleomorphic adenoma or myoepithelioma [5]. In the recent WHO classification of salivary gland tumours, subclassification include a heterogenous group of tumours termed as sialolipoma. The term "sialolipoma" is used when the histological features are reminiscent of a normal salivary gland, justifying its reproducible classification. The amount of fatty tissue present in the reported cases of sialolipoma was in the range of 40%-70%. The presence of well-encapsulated tumour on gross examination differentiates sialolipoma from the fatty infiltration of the salivary gland tissue [5–7]. A minor subset of biphasic tumours with oncocyticlipo epithelial lesions have predominantly epithelial component, which is helpful in categorizing these as "lipoadenoma containing abnormal oncocytic component" or oncocytic lipoadenoma. The amount of oncocytic component may vary from tumour to tumour and within the different areas of a tumour. The oncocytic component in our case was about 50% and was in sheets and lobules, surrounded by and focally infiltrated by a benign lipomatous component. Nagao [7] suggested that there was entrappment of glandular component within the lobules of adipose tissue and the pathogenesis was of non-neoplastic nature. Later on Akrish et al., [8] came up with other hypothesis saying that a dysfunction of a salivary gland leading to modification of function of salivary gland could lead to the tumorigenesis, supporting it with findings such as absence of recurrence, prolonged natural history, histological features of duct ectasia, periductal fibrosis, oncocytic metaplasia, replacement of normal salivary gland tissue with adipose tissue as well as the chronic inflammatory infiltrate. On histology, other differential diagnosis for oncocytic lipoadenoma are pleomorphic adenoma with lipometaplasia and lipomatosis. Pleomorphic adenoma can be excluded by presence of normal salivary gland tissue and other features of pleomorphic aednoma. A distinctly placed oncocytic and lipomatous components on gross examination allows oncocytic lipoadenoma to be separated from lipomatosis, fibrolipoma and other lipomatous tumours. Our case also showed foci of sebaceous metaplasia, periductal chronic inflammation and periductal fibrosis. These findings are consistent with the histological features described in published studies [1,2]. In our case, presence of histological findings like lobules of lipocytes, sebaceous metaplasia, periductal chronic inflammation and periductal fibrosis, overlap with those of sialolipoma which may suggest association between these entities [2]. Immunohistochemical findings in the form of cytokeratin profile P63 and cytogenetic studies carried out so far also suggest that there is significant association between oncocytic lipoadenoma and sialolipoma [9]. Due to rarity of these tumours and their heterogeneous histological and clinical features, a reliable and reproducible classification is difficult, however, increased awareness of these entities has resulted in increased number of reported cases during the last few years. These rare tumours will be better understood and recognized regarding their clinical profile and biological behavior if further evidence is sought after. Larger studies and molecular profiling is required for further understanding of these tumours that will help in establishing a proper classification.Our case adds to the very small tally of oncocytic lipoadenomas.
Conclusion
Oncocytic lipoadenoma, a rare subtype of lipomatous tumours of salivary gland, has been omitted from WHO classification. Our aim is to add this case into the existing small pool of case reports of this rare entity, which may enhance its understanding and help in putting them under a proper “umbrella” from a “waste basket” category.
[1]. Baker SE, Jensen JL, Correll RW, Lipomas of the parotid glandOral Surg Oral Med Oral Pathol 1981 52:167-71. [Google Scholar]
[2]. Abbas A, Stephan I, Bruno M, Michael L, Johannes Z, Arndt H, Lipomatous Salivary Gland Tumour: A series of 31 cases spanning their morphologic spectrum with emphasis on Sialolipom and Oncocytic lipoadenomaAm J of SurgPathol 2013 37(1):128-37. [Google Scholar]
[3]. Barnes L, Eveson JW, Reichart P, Sidransky D, WHO Classification of TumoursPathology and Genetics of Head and Neck Tumours 2005 LyonIARC Press:275 [Google Scholar]
[4]. Walts AE, Perzik SL, Lipomatous lesions of the parotid areaArch Otolaryngol 1976 102:230-32. [Google Scholar]
[5]. Jin YT, Lian JD, Yan JJ, Pleomorphic adenoma with extensive adipose contentHistopathology 1996 28:87-89. [Google Scholar]
[6]. Skálová A, Stárek I, Simpson RH, Spindle cell myoepithelialtumours of the parotid gland with extensive lipomatous metaplasia. A report. of four cases with immunohistochemical and ultrastructural findingsVirchows Arch 2001 439:762-67. [Google Scholar]
[7]. Nagao T, Sugano I, Ishida Y, Sialolipoma: a report of seven cases of a new variant of salivary gland lipomaHistopathol 2001 38:30-36. [Google Scholar]
[8]. Akrish S, Leiser Y, Shamira D, Paled M, Sialolipoma of salivary gland:two new cases, literature review and histogenetichypothesisJ Oral MaxillofacSurg 2011 69:1380-84. [Google Scholar]
[9]. Ilie M, Hofman V, Pedeutour F, Oncocytic lipoadenoma of the parotid gland: Immunohistochemical and cytogenetic analysisPathol Res Pract 2010 206:66-72. [Google Scholar]