Pulmonary Hemorrhage (PH) in Extremely Low Birth Weight (ELBW) Infants: Successful Treatment with Surfactant
Pradeep Suryawanshi1, Rema Nagpal2, Vaibhav Meshram3, Nandini Malshe4, Vijay Kalrao5
1Head & Professor, Department of Neonatology, BVU Medical College, Katraj-Dhankawadi, Pune, India.
2Assistant Professor, Department of Neonatology, BVU Medical College, Katraj-Dhankawadi, Pune, India.
3Clinical Fellow, Department of Neonatology, BVU Medical College, Katraj-Dhankawadi, Pune, India.
4Associate Professor, Department of Neonatology, BVU Medical College, Katraj-Dhankawadi, Pune, India.
5Professor, Department of Pediatrics, BVU Medical College, Katraj-Dhankawadi, Pune, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradeep Suryawanshi, Head & Professor, Department of Neonatology, BVU Medical College, Katraj-Dhankawadi, Pune-411043, India.
E-mail: drpradeepsuryawanshi@gmail.com
We report a case of an extremely low birth weight (ELBW) infant presenting with pulmonary hemorrhage (PH) in which we have given surfactant after an acute episode of bleeding with severe intractable hypoxemia. Surfactant replacement therapy showed improvement in Mean Airway Pressure (MAP) and oxygenation indices. Our case suggests that surfactant replacement therapy is useful in PH.
Conventional ventilation, Hypoxia, Preterm
Case Report
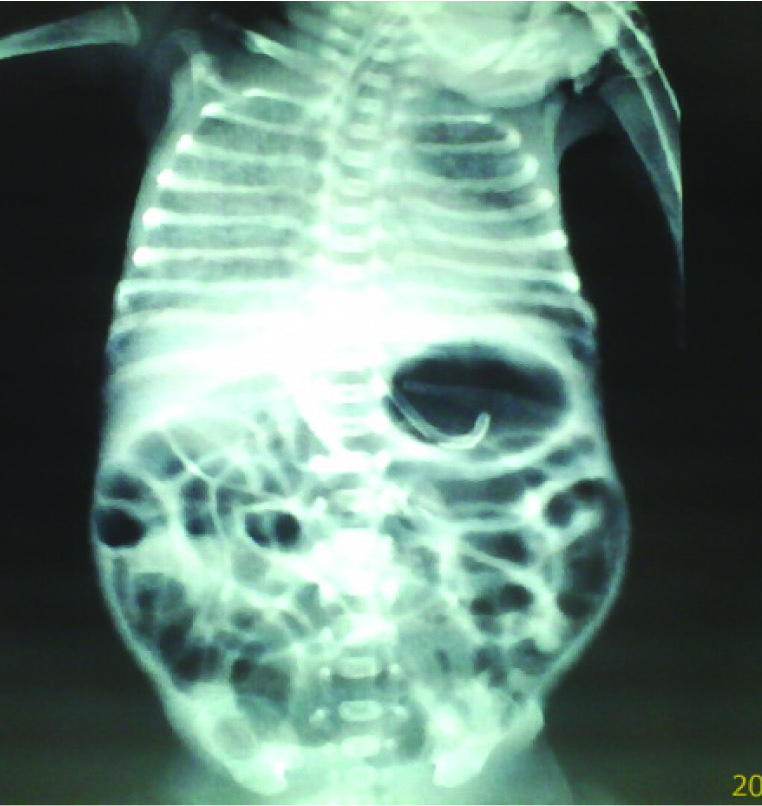
A preterm male neonate 27-week-gestation and birth weight of 680 grams was admitted in neonatal intensive care unit with grade IV respiratory distress syndrome (RDS) was ventilated and given surfactant treatment. RDS, Patent ductus arteriosus, Neonatal jaundice and sepsis complicated the initial course. On day 20th of life, the neonate developed profuse PH. We noticed fresh blood in the endotracheal tube associated with desaturation (SpO2 74%) and a Chest X-Ray compatible with PH [Table/Fig-1]. The infant needed blood transfusion because of anemia (Hb 85 g/L). Coagulation tests were normal. After intubation, a second episode of PH occurred with desaturation (SpO2 60%) and increased oxygen requirement (FiO2 1.0) leading to increase in MAP up to 15 cm H2O on conventional ventilation. Despite high settings on conventional ventilation oxygen saturation remained poor (SO2 50-60%). In view of high FiO2 (1.0) requirements and high MAP (15 cm H2O) decision was taken to give a trial of surfactant therapy. Surfactant (Curosurf, Chiesi farmaceutici S.P.A., Parma, Italy, 200 mg/kg) was given as a bolus. Clinical and radiological improvement [Table/Fig-2] was noted after 24 hr of surfactant therapy. Baby was successfully extubated after 48 hr of surfactant therapy, on day 23rd of life.
Discussion
PH is a life threatening condition occurring to 1-12/1000 live births, with rates increasing to 50/1000 live births in risk groups, such as prematurity, IUGR, and/or sepsis [1]. Smaller gestational age, lower birth weight, lower Apgar scores at one and five min, severe RDS (grades 3 or 4), and use of surfactant in very low birth weight infants at greater risk of PH [2]. Different approaches have been proposed for the management of PH in newborn infants, including high airway pressures during mechanical ventilation high frequency oscillation [3], ECMO [4], administration of recombinant activated Factor VII [5] and surfactant replacement therapy [6].
PH has been effectively managed using surfactant instillation, including in those infants who have previously been treated with surfactant [3-5]. Pandit et al., [7] showed improvement in oxygen indices after six hours of surfactant replacement therapy in 15 neonates with PH.
Amizuka et al., [8] treated 26 out of 27 neonates with PH occurring at 1.5 h after birth with surfactant. Treatment was at 3.0 h after the onset of PH. A good response to exogenous surfactant was seen in 82% of cases.
In majority of case studies [7-9] surfactant was given as a treatment of pulmonary hemorrhage in first week of life. However, our case presented with pulmonary hemorrhage on day 20th of life and responded to surfactant therapy.

Conclusion
Smaller gestational age, lower birth weight, lower Apgar scores at one and five min, severe respiratory distress syndrome (grades 3 or 4), and use of surfactant place very low birth weight infants at greater risk of PH. Surfactant replacement therapy is useful in treatment of massive PH. Further randomized controlled trial would be useful for identification of potential benefit
[1]. CH Ferreira, F Carmona, FE Martinez, Prevalence, risk factors and outcomes associated with pulmonary hemorrhage in newborns J Pediatr (Rio J) 2014 90:316-22. [Google Scholar]
[2]. TM Berger, EN Allred, LJ Van Marter, Pulmonary hemorrhage in very low-birth weight infants: risk factors and management. Chen YY1, Taiwan Premature Infant Development Collaborative Study GroupPediatr Int 2012 54(6):743-47. [Google Scholar]
[3]. MD Pappas, AP Sarnaik, KL Meert, Idiopathic pulmonary hemorrhage in infancy. Clinical features and management with high frequency ventilationChest 1996 110:553-55. [Google Scholar]
[4]. NS Kolovos, DJ Schuerer, FW Moler, Extracorporal life support for pulmonary hemorrhage in children: a case seriesCrit Care Med 2002 30:577-80. [Google Scholar]
[5]. R Grizeli, J Vukovic, B Filipovic-Grcic, Successful use of recombinant activated FVII and aminocaproic acid in four neonates with life-threatening hemorrhageBlood Coagul Fibrinolysis 2006 17:413-15. [Google Scholar]
[6]. TM Neumayr, AM Watson, ME Wylam, Y Ouellette, Surfactant treatment of an infant with acute idiopathic pulmonary hemorrhagePediatr Crit Care Med 2008 9:e4-6. [Google Scholar]
[7]. PB Pandit, MS Dunn, EA Colucci, Surfactant therapy in neonates with respiratory deterioration due to pulmonary hemorrhagePediatrics 1995 95:32-36. [Google Scholar]
[8]. T Amizuka, H Shimizu, Y Niida, Y Ogawa, Surfactant therapy in neonates with respiratory failure due to haemorrhagic pulmonary oedemaEuropean Journal of Pediatrics 2003 162:697-702. [Google Scholar]
[9]. Bozdag Senol, Dilli Dilek, Gökmen Tülin, Dilmen Ugur, Comparison of Two Natural Surfactants for Pulmonary Hemorrhage in Very Low-Birth-Weight Infants: A Randomized Controlled TrialAmer J PerinatolDOI: 10.1055/s-0034-1389090. 2014 Sep 21 (Epub ahead of Print) [Google Scholar]