T-Cell Lymphoma of the Oral Cavity: Case Report
Kanika Rana1, Vineet Narula2, Eishaan K Bhargava3, Ravi Shankar4, Nidhi Mahajan5
1Senior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College, India.
2Senior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College, India.
3Junior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College, India.
4Junior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College, India.
5Assistant Professor, Department of Pathology, Maulana Azad Medical College, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kanika Rana, Senior Resident, Department of ENT, BL Taneja Block, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi-110002, India.
E-mail: dr.rana.kanika@gmail.com
Lymphomas are heterogenous malignancies of the lymphatic system characterized by lymphoid cell proliferation. They can broadly be divided into Hodgkin’s lymphoma (HL) and non- Hodgkin’s lymphoma (NHL). NHL can originate from B, T, or natural killer (NK) lymphocytes. Extra-nodal presentation of T-cell NHL is extremely rare, and is often seen in immunocompromised individuals. Here, we report a rare case of T-cell lymphoma of the oral cavity in an immune-competent patient. The patient was diagnosed to have T-cell NHL on the basis of biopsy and immunohistochemistry, and was referred to oncology department for chemotherapy for definite treatment.
Gingiva, Non- Hodgkin’s lymphoma
Case Report
A 55-year-old male patient presented to ENT out-patient department with the complaints of a growth on gums of right side of the lower jaw since three months. The growth had rapidly increased in size, and was associated with pain. There was no history of bleeding from the growth, nor did the patient complain of fever, night sweats or weight loss. The patient was a chronic tobacco chewer, however, there was no history of smoking or of alcohol addiction. On oral examination, there was an irregular proliferative mass involving the right lower gingivo-buccal sulcus, extending from the canine tooth till the third molar, and extending on to the retromolar trigone. The growth also involved the lingual surface of mandible and the adjacent floor of the mouth [Table/Fig-1]. The mass was tender and firm in consistency, and did not bleed on palpation. On examining the neck, there was no palpable lymphadenopathy.
The patient underwent a contrast enhanced computed tomography (CECT) scan of oral cavity and neck which revealed a heterogeneously enhancing soft tissue density lesion involving the right buccal mucosa and inferior gingivo-buccal sulcus on right side with involvement of the retromolartrigone. The lesion measured 3.8 x 3.6 x 2.3 cm and was seen to cause destruction of the alveolar process and the body of the underlying mandible. The lesion was found to be abutting the floor of the mouth.
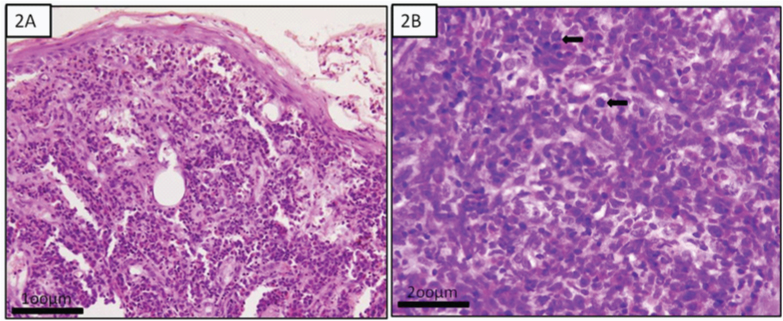
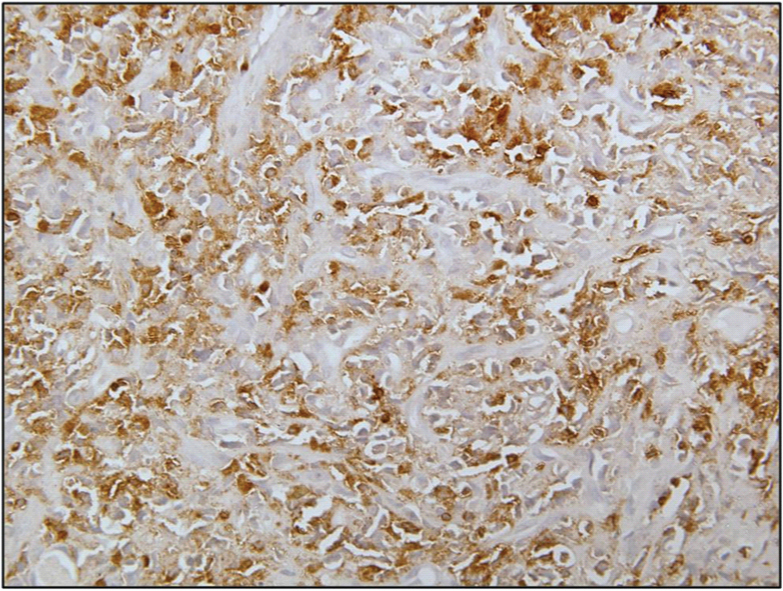
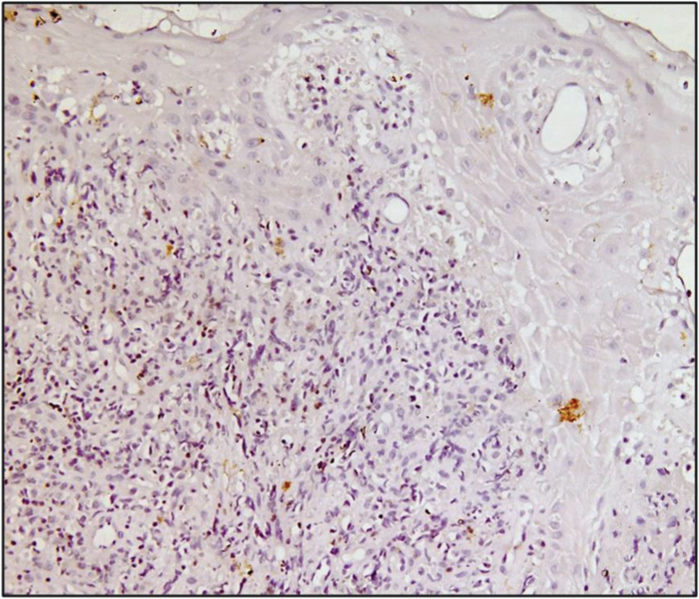
The patient was taken up for an incisional biopsy of the growth under local anaesthesia. Histopathological examination revealed sheets of round cells, large in size with scanty cytoplasm, opened up nuclear chromatin and inconspicuous to single prominent nucleoli. The nuclear membrane was irregular with frequent typical and atypical mitotic figures, with accompanying numerous mature eosinophils and few lymphocytes [Table/Fig-2a&b ]. On immunohistochemistry, the tumour cells were positive for leukocyte common antigen (LCA) and T-cell lineage (CD45RO), and negative for CD1a, B-cell, EMA, cytokeratin, anti-MPO, CD68 and CD20 [Table/Fig-3,4]. Thus a diagnosis of T-cell NHL of oral cavity was established. In order to stage the disease and rule out any systemic manifestations, patient underwent CECT chest and abdomen, and a bone marrow biopsy. Both radiological and haematological investigations were found to be normal indicating no systemic infiltration of NHL cells. The patient was then referred to the oncologists where he was planned for six cycles of chemotherapy (CHOP regimen) with cyclophosphamide, hydrodaunorubicin, vincristine and prednisolone. Unfortunately, the patient received only 3 cycles of chemotherapy and died due to sepsis.
Discussion
Lymphomas are heterogenous malignancies characterized by proliferation of lymphoid cells or their precursors. They can be classified as HL or non-Hodgkin’s lymphoma (NHL) [1]. NHL can further be sub-classified into B-cell, T-cell, or NK/T cell types. NHL presents more commonly than HL, representing about 86% of all lymphomas, and B-cell lymphomas are seen more frequently than T-cell lymphomas [2].
HL rarely shows extra-nodal disease (1% cases), whereas NHL presents as extra-nodal disease in approximately 23-30% of cases [3]. Extranodal NHL is commonly seen to involve gastrointestinal tract, waldeyer’s ring, skin, bones, and others. Oral cavity involvement is seen in only 2% of cases [4]. Due to rare presentation of extra-nodal T-cell NHL in oral cavity, clinicians often find difficulties in proper management of such patients. Various oral sub-sites involving T-cell NHL as mentioned in literature include labial commissure, gingiva, palate, maxilla, buccal mucosa, floor of the mouth, gingivo-buccal sulcus, tongue and uvula [2,4,5] .
These tumours show a wide spectrum of behavior ranging from relatively indolent to highly aggressive and potentially fatal course [6]. It has slowly grown from a rare cancer to the fifth most common cancer in the world over a period of 30 years [7]. Our patient expired after three cycles of chemotherapy due to the potentially fatal nature of the disease. On reviewing the literature, mixed treatment outcomes in oral T-cell NHL were seen, and it was observed to be unrelated to the site of the tumour. Similar fatal outcomes were seen in patients having manifestations of T-cell lymphoma as uvular mass, labial swelling, mouth ulcers, buccal mucosa and upper gingiva, within three months of commencement of chemotherapy [5,8]. Complete remission with chemotherapy or radiotherapy, though less commonly seen, has been reported in patients with involvement of labial commissure and oral mucosa by Villa et al., and May et al., [2,9].
NHL has commonly been associated with HIV, and is considered the second most common HIV-associated malignancy after Kaposi’s sarcoma. The risk of NHL is 60 times greater in patients with HIV disease than in otherwise healthy persons [10]. T-cell lymphoma has occasionally been reported with systemic conditions like celiac sprue, crohn’s disease and several autoimmune diseases [11,12]. However, the patient in our case report was not found to be suffering from HIV- AIDS, any other systemic illnessor immune compromising condition. Immunohistochemistry plays an important role in the diagnosis and classification of hemato-lymphoid neoplasms. The peripheral T-cell lymphomas are about 90% positive for CD3 and CD45RO while B-cell markers include CD19, CD20, CD30 and CD 79. New cell and lineage markers are constantly being discovered and added to the existing list of antibodies [4,7].
A similar case was reported by Bagirath PV et al., describing a 68-year-old, male patient of oral T-cell NHL, involving buccal mucosa and lower gingiva, in a known case of HIV seropositive patient [7]. The diagnosis was made on the basis of biopsy and immunohistochemistry positivity with CD45 and CD3. The patient was referred for chemotherapy, and was lost to follow up. Another case was reported in 76-year-old Japanese women with gingival swelling in both the maxilla and mandible by Matsumoto et al., [13]. The biopsy and positive immunochemistry with CD45RB, CD45RO and CD30 helped in diagnosing the case as an oral anaplastic large cell lymphoma (ALCL), a subtype of T-cell lymphoma.
Treatment options for NHL include chemotherapy, radiotherapy, or both in combination. The CHOP regimen is most widely used for NHL and includes cyclophosphamide, hydrodaunorubicin, vincristine and prednisolone. The R-CHOP regimen includes rituximab (anti-CD20) which improves the cure rate. Radiotherapy alone is considered effective in early stage of presentation. Most studies recommend combination treatment for higher stage disease [14]. Newer agents like Alemtuzumab and Denileukindiftitox have also emerged and are under investigation.
Clinical photograph showing a proliferative growth present in the right gingivobuccal sulcus, extending from the canine tooth till the third molar. The growth is extending onto the adjacent buccal mucosa, retromolartrigone, and lingual surface of the mandible, and abutting the floor of mouth

2a) Histopathology shows sheets of atypical lymphoid cells reaching till the overlying epidermis. (H&E 100X). 2b) shows large atypical cells with vesicular nucleus with prominent cleaving, opened up nuclear chromatin and prominent nucleolus in a mixed inflammatory background of eosinophils, lymphocytes and plasma cells. High mitoses is seen. (H&E 200X) (Arrows show areas of mitoses).
Immunohistochemistry showing intense cytoplasmic expression of CD45RO (T-cell marker) by atypical lymphoid cells. (200X)
Immunohistochemistry showing tumor cells negative for CD20 (B-cell marker). (100X)
Conclusion
T-cell lymphomas present rarely in oral cavity and should be considered as a possible differential diagnosis of any growth in the oral cavity. They can have variable presentations and can easily be confused with other malignancy like squamous cell carcinoma or with pyogenic granuloma. Histopathology and immunohistochemistry play the most important role in the diagnosis of these disorders. Since T-cell lymphomas are associated with an aggressive course, early diagnosis and prompt treatment with chemotherapy and radiotherapy is the key for success in treatment of these disorders.
[1]. NL Harris, World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting, Airlie House, Virginia, November 1997Ann Oncol 1999 10(12):1419-32. [Google Scholar]
[2]. A Villa, U Mariani, F Villa, T-cell lymphoma of the oral cavity: a case reportAust Dent J 2010 55(2):203-203. [Google Scholar]
[3]. E Hanna, J Wanamaker, D Adelstein, R Tubbs, P Lavertu, Extranodal lymphomas of the head and neck: a 20 year experienceArch Otolaryngol Head Neck Surg 1997 123:1318-23. [Google Scholar]
[4]. GH Shah, SK Panwar, PP Chaturvedi, SN Kane, Isolated primary extranodal lymphoma of the oral cavity: a series of 15 cases and review of literature from a tertiary care cancer centre in IndiaIndian J Med Paediatr Oncol 2011 32(2):76-81. [Google Scholar]
[5]. WS Lai, CH Wang, CP Shih, T-cell lymphoma manifesting as a uvular massRheumatology (Oxford) 2013 52(4):608 [Google Scholar]
[6]. S Parihar, RK Garg, P Narain, Primary extra-nodal non-Hodgkin’s lymphoma of gingiva: a diagnostic dilemmaJ Oral Maxillofac Pathol 2013 17(2):320 [Google Scholar]
[7]. PV Bagirath, JV Kumar, UD Arvind, G Shailaja, Aggressive extranodal peripheral T-cell non- Hodgkin’s lymphoma: a rare case report and reviewJ Oral Maxillofac Pathol 2014 18(1):80-83. [Google Scholar]
[8]. HA Pontes, Extranodal Nasal NK/T-cell Lymphoma: a rare oral presentation and FASN, CD-44 and GLUT-1 expressionBraz Dent J 2013 24(3):244-48. [Google Scholar]
[9]. SA May, Oral-cutaneous CD4-positive T-cell lymphoma: a study of two patientsAm J Dermatopathol 2007 29(1):62-67. [Google Scholar]
[10]. KF Basavaraj, K Ramalingam, A Sarkar, S Muddaiah, Primary non-Hodgkin’s lymphoma of gingiva in a 28-year old HIV-positive patientJ Nat Sci Biol Med 2012 3(2):189-91. [Google Scholar]
[11]. CH Shiboski, D Greenspan, CL Dodd, TE Daniels, Oral T-cell lymphoma associated with celiac sprue. A case report Oral Surg Oral Med Oral Pathol 1993 76(1):54-58. [Google Scholar]
[12]. C Scully, JW Eveson, H Witherow, AH Young, RS Tans, ED Gilby, Oral presentation of lymphoma: case report of T-cell lymphoma masquerading as oral Crohn’s disease, and review of the literatureEur J Cancer B Oral Oncol 1993 29(3):225-29. [Google Scholar]
[13]. N Matsumoto, Anaplastic large cell lymphoma in gingiva: case report and literature reviewOral Surg Oral Med Oral Pathol Oral Radiol Endod 2008 106(4):29-34. [Google Scholar]
[14]. RI Van der Waal, PC Huigens, VP Van der, I Van der Waal, Characteristics of 40 primary extranodal non-Hodgkin’s lymphomas of the oral cavity in perspective of the new WHO classification and the International Prognostic IndexInt J Oral Maxillofac Surg 2005 34(4):391-95. [Google Scholar]