Solitary Fibrous Tumour of Lacrimal Gland: A Rare Entity
Vikram Narang1, Nagi Anitaraj Rajendra Singh2, Gurkirat Singh Bajwa3, Neena Sood4
1 Assistant Professor, Department of Pathology, Dayanand Medical College & Hospital, Ludhiana, India.
2 Resident, Department of Pathology, Dayanand Medical College & Hospital, Ludhuana, India.
3 Professor & Head, Department of Opthalmology, Dayanand Medical College & Hospital, Ludhuana, India.
4 Professor & Head, Department of Pathology, Dayanand Medical College & Hospital, Ludhuana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Vikram Narang, Assistant Professor, Department of Pathology, DMCH, Ludhiana, India.
E-mail: drvikramnarang@yahoo.com
Solitary fibrous tumour (SFT) is a rare spindle cell tumour of mesenchymal origin most commonly encountered in pleura. It can affect the orbital region but SFT of lacrimal gland is rare. We hereby report of a SFT of lacrimal gland in a 50-year-old male presenting with slow growing swelling in left superolateral orbital region. The preliminary fine needle aspiration cytology (FNAC) could not reveal any definite diagnosis. Excision biopsy and immunohistochemistry (IHC) confirmed the diagnosis. Therefore, clinician and pathologist should be aware of this entity and biopsy along with IHC is required to rule out other entities which can mimic it clinically and histopathologically.
Immunohistochemistry, Mesenchymal lesion, Spindle cell tumour
Case Report
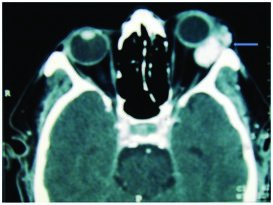
A 52-year-old male presented to the ophthalmology outpatient department with complaints of swelling in the left supero-lateral aspect of the orbit (lacrimal gland region) for past two years. Patient gave history of gradual increase in size of the lesion. On examination, the swelling was apparently soft and non tender. He ruled out any history of trauma at this site. No associated ocular complaints were present. Routine investigations like Complete blood counts, Liver function tests, Renal function tests, Viral markers (HIV, HbsAg and HCV) were unremarkable. Magnetic resonance imaging (MRI) and FNAC were advised with clinical possibility of Lipoma. MRI revealed an extra corporal mass on supero lateral aspect of left orbit possibly lacrimal in origin [Table/Fig-1]. FNAC smears were scantily cellular and exhibited spindle shaped cells with bland chromatin and inconspicous nucleoli against a haemorrhagic background. Scant cellularity hampered the diagnosis and only a suggestion of neoplastic nature of the lesion was offered. Wide local excision of the lesion was planned and tissue was sent for histopathology.
MRI showing an extra corporal mass on supero lateral aspect of left orbit
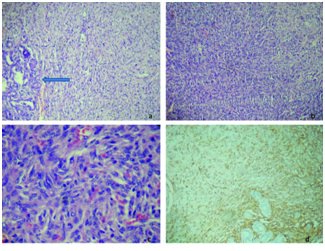
Histopathological examination revealed partly encapsulated cellular tumour arising from the lacrimal gland. The tumour cells were arranged in patternless sheets and fascicles with focal storiform pattern. The tumour cells had spindle shaped nuclei with moderate amount of ill defined eosinophilic cytoplasm and an occasional mitotic figure. Histomorphology was suggestive of benign spindle cell tumour. IHC was done to rule out the possibility of schwannoma/hemangiopericytoma. On IHC the tumour cells were positive for CD34, Vimentin and negative for SMA and S100 on IHC [Table/Fig-2a–d]. The MIB1 labelling index was less than 1%. Hence, the final diagnosis of SFT of lacrimal gland was made. The patient is now on follow up and shows no evidence of local recurrence.
(2a)Microphotograph showing junction of lacrimal gland and tumour (arrow) (H&E,100X)
(2b)- Microphotograph exhibiting patternless sheets of tumour cells (H&E,100X)
(2c)-Microphotograph of high power view of spindle shaped tumour cells (H&E, 400X)(2d)- Microphotograph showing tumour cells to be positive for CD34 (200X)
Discussion
SFT is a rare tumour of adults that originally was believed to be derived from mesothelium. However, the subsequent identification of this tumour in sites not usually associated with serosal surfaces, including the thyroid and parotid glands, nasal cavity, and paranasal sinuses, supports a mesenchymal origin for this neoplasm. These tumours arise in the fifth to seventh decades of life, with no apparent sex predilection [1,2]. Dorfman et al., also reported three cases of orbital region SFTs in 44-year-old male, 65-year-old female and 69-year-old female [3]. The present case is also a 50-year-old male.
Because SFT may not be well known to many ophthalmologists and because of the tumour's variable histopathologic appearance, SFT may be easily misdiagnosed [4]. Orbit is an unusual site for SFT to occur and generally pursues a slow, indolent, and nonaggressive course, reaches a size up to 4.5 cm [5]. The present case was also a slow growing tumour with duration of two years and size of 3.5 cms.
Histopathologic analysis may be of prognostic as well as diagnostic importance as SFT associated with hypercellularity, cellular pleomorphism, and an elevated mitotic count (2:4 per 10 high-power fields) has an aggressive clinical behavior such as local recurrence, and distant metastases [5]. The biopsy may show large areas of the tumour containing storiform formations, sarcoma-like areas, fascicular formations, neural type palisades, and hemangiopericytoma-like patterns [6]. Differential diagnosis based on histopathological features includes meningioma, fibrous histiocytoma, schwannoma and hemangiopericytoma. Of these tumours, a differential diagnosis to hemangiopericytoma with SFT is mandatory because hemangiopericytoma has a aggressive clinical course with high recurrence and higher rate of distant metastasis as compared to the general benign nature of SFT. The hemangiopericytoma is typically composed of small, oval to slightly spindle shaped cells and “staghorn” vascular pattern.
For definite diagnosis pathologist rely on immunohistochemical stains. Strong and consistent CD34 immunoreactivity in SFT can be the important clue. Immunohistochemical analysis of hemangiopericytoma reveals strong positivity to vimentin, factor XIIIa and Leu-7, and weak positivity to desmin and cytokeratin and weak positivity to CD34.The present case also showed patternless sheets of spindle cells exhibiting strong positivity with CD34 [7–9].
Although histologic characteristics and frequent CD34 expression allow for an accurate diagnosis in the majority of SFT cases, a wide histologic spectrum and an occasional unexpected immunophenotype may pose diagnostic challenges. Molecular analyses and recent studies have suggested that almost all SFTs harbor an NAB2-STAT6 fusion gene, which is considered specific to this tumour type [10].
The prognosis in SFT, depends upon complete resection rather than histologic findings because the clinical behavior of SFT varies disregards of the histologic prognostic factors [8,9].
Conclusion
SFT is a rare tumour in lacrimal gland region. The histopathological examination along with IHC is essential for accurate diagnosis. The clinician and pathologist must be aware of this entity to understand the prognostic implications of tumour and to differentiate it from other spindle cell tumour which can mimic this rare lesion.
[1]. Scott IU, Tanenbaum M, Rubin D, Lares E, Solitary Fibrous Tumour of the Lacrimal Gland FossaOphthalmology 1996 103:1613-18. [Google Scholar]
[2]. Ali SZ, Hoon V, Hoda S, Heelan R, Zakowski MF, Solitary fibroustumour. A cytologic-histologic study with clinical, radiologic, and immunohistochemical correlationsCancer 1997 81:116-21. [Google Scholar]
[3]. Dorfman DM, To K, Dickersin GR, Solitary fibrous tumour of the orbitAm J Surg Pathol 1994 18:281-7. [Google Scholar]
[4]. Galie M, Tieghi R, Cavazzini L, Clauser L, Solitary fibrous tumour of the orbit : a case reportInt J Oral MaxillofacSurg 2005 34:331-33. [Google Scholar]
[5]. Giuffre I, Faiola A, Bonanno E, Liccardo G, Solitary fibrous tumour of the orbit. Case report and review of the literatureSurgNeurol 2001 56:242-46. [Google Scholar]
[6]. O’Donovan DA, Bilbao JM, Fazl M, Antonyshyn OM, Solitary fibrous tumour of the orbitJ Craniofac Surg 2001 13:641-44. [Google Scholar]
[7]. Perry A, Scheithauer BW, Nascimento AG, The immunophenotypic spectrum of meningeal hemangiopericytoma: a comparison with fibrous meningioma and solitary fibrous tumour of meningesAm J Surg Pathol 1997 21:1354-60. [Google Scholar]
[8]. Ha JK, Park BJ, Kim YH, Lim YJ, Orbital Solitary Fibrous Tumour : A Case Report and Diagnostic CluesJ Korean Neurosurg Soc 2009 46:77-80. [Google Scholar]
[9]. Westra WH, Gerald WL, Rosai J, Solitary fibrous tumour. Consistent CD34 immunoreactivity and occurrence in the orbitAm J Surg Pathol 1994 18:992-98. [Google Scholar]
[10]. Yoshida A, Tsuta K, Ohno M, Yoshida M, Narita Y, Kawai A, STAT6 immunohistochemistry is helpful in the diagnosis of solitary fibrous tumoursAm J Surg Pathol 2014 38(4):552-59. [Google Scholar]