Chrysosporium: An Uncommon Fungus in Chronic Rhinosinusitis
Panduranga M. Kamath1, Vishnu Prasad2, Vijendra S. Shenoy3, Aswin Mukundan4, Suchithra Shenoy5
1Professor, Department of Otorhinolaryngology, Head & Neck Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
2Consultant, Department of Otorhinolaryngology, Head & Neck Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
3Associate Professor, Department of Otorhinolaryngology, Head & Neck Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
4Junior Resident, Department of Otorhinolaryngology, Head & Neck Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
5Associate Professor, Department of Microbiology, Kasturba Medical College, Mangalore, Manipal University, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishnu Prasad, Consultant, Department of Otorhinolaryngology – Head & Neck Surgery, Kasturba Medical College, Mangalore, Manipal University, Karnataka – 575001, India.
E-mail: dr.vishnukp@yahoo.com
Chronic rhinosinusitis is one of the commonest health problem encountered in rhinology. Of these allergic fungal rhinosinusitis forms a significant group of patients. Patients commonly present with typical symptoms of sinusitis and the diagnosis is often made after imaging and/or intraoperatively. We report a rare case of allergic fungal sinusitis (AFS) caused by Chrysosporium species in a 70-year-old male with no co-morbidities. The fungus was isolated from allergic mucin collected from the sinuses. Therapy with intravenous Voriconazole was given leading to good relief for the patient, and no recurrences have occurred till date. Infections caused by Chrysosporium species are very rare, and is very rarely been reported to cause sinusitis in humans.
Allergic mucin, Fungal sinusitis, Voriconazole
Case Report
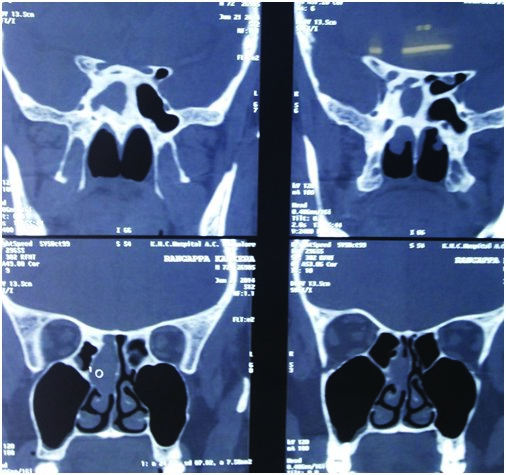
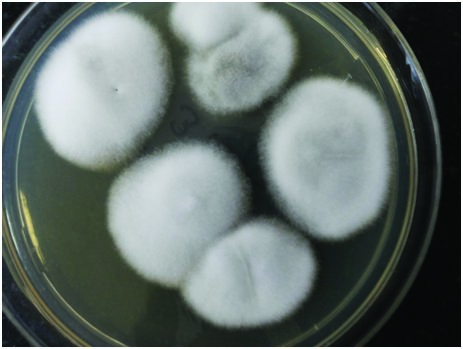
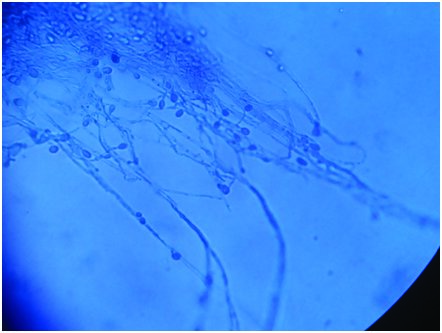
A healthy 70-year-old male patient, who was a farmer by occupation presented to us with complaints of recurrent right sided nasal block, right sided retro-orbital pain and multiple episodes of epistaxis of three months duration. There was no history of tuberculosis, diabetes mellitus or other immunocompromised states. The diagnostic nasal endoscopy did not reveal any gross abnormality except for a deviated nasal septum to right, minimal mucosal discharge on right nasal cavity and polypoidal mucosa over right middle turbinate. His serum IgE was 305 UI/ml. CT scan of the Nose and Paranasal Sinuses showed a soft tissue density obliterating the right sphenoid sinus and right posterior ethmoid air cells with widened sphenoethmoidal recess [Table/Fig-1]. Functional Endoscopic Sinus Surgery was done to clear out the disease from sinuses. Intraoperatively fungal debris and mucin with mucosal hypertrophy was found in the right posterior ethmoid sinus and sphenoid sinus which was sent for microbiological examination. There were no complications intraoperatively or postoperatively and the patient was discharged in the third postoperative day. Microbiological examination confirmed the presence of the fungus on Potassium Hydroxide preparation. The fungus grew on Sabouraud’s dextrose agar after one week of incubation as white cottony growth with reverse light brown. On Lactophenol cotton blue preparation hyaline, septate hyphae with terminal one celled ovoid smooth walled conidia were present [Table/Fig-2,3]. Patient was readmitted and started on intravenous Voriconazole 300 mg twice daily for nine days. Patient was quite comfortable during the period of the treatment and he showed satisfactory symptomatic improvement. Patient is now on constant follow up and has since reported good relief in symptoms and there have been no signs of recurrence till date.
Discussion
Chronic rhinosinusitis is a major cause of morbidity in our current era affecting more than 14% of adults and children [1]. Acute rhinosinusitis is usually unimicrobial whereas chronic form will have multiple microorganisms [1]. Chronically infected sinuses are often inhabitant for fungus which is difficult to completely eradicate hence adding complications or morbidities [2]. Incidence of AFS is 5-10% of all cases of chronic rhinosinusitis which requires surgery [3]. It represents an allergic/hypersensitivity disorder and is the commonest form of fungal rhinosinusitis [4]. Members of the dematiaceous family are commonly implicated like alternaria, curvularia, fusarium, rhizopus, drechslera and excerohilum [5].
AFS is an allergic/hypersensitivity response to extramucosal fungal pathogens in the sinus [6]. It occurs mainly in immunocompetent patients, in contrast to invasive fungal diseases that usually involve an immunocompromised host. In 2003, Kuhn and Swain [7] described five major and six minor criteria for diagnosis of AFS in adults. The former were: (1) type I IgE-mediated hypersensitivity; (2) nasal polyposis; (3) characteristic CT findings; (4) allergic mucin; and (5) positive fungal smear and/ or culture. The later criteria included: (1) asthma; (2) unilateral predominance; (3) radiographic bone erosion on CT; (4) positive fungal culture; (5) Charcot-Leyden crystals; and (6) serum eosinophilia. Our patient had most of the major criteria including a raised serum IgE levels. AFS is commonly found in tropical climates like in India and is commonly seen in third to fifth decades of life. Majority of the patients have history of allergy [8]. In majority of patients CT scan shows unilateral involvement with expansion of involved sinuses sometimes with internal hyper-density of the affected sinuses [9]. But our patient did not present with the typical symptoms of allergic rhinosinusitis and there was no history of atopy or asthma. Also, imaging showed patient had a unilateral sinus involvement with widening of the sphenoethmoidal recess. The key to surgical management is the complete removal of all allergic mucin, polyps and fungal debris to decrease antigenic load and to provide adequate drainage and ventilation to all sinuses [3].
Chrysosporium is rarely seen in fungal debris or allergic mucin isolated from sinuses. Chrysosporium is a poorly known, thermotolerant and keratinophilic species. Such fungi are encountered in the diagnostic laboratory predominantly as contaminants [10]. It was initially discovered by horse hair bait from horse dung collected in Kuwait and is rarely implicated in AFS. Fungi isolated in AFS were thought to be non-cross reactive but recent discovery of an 18-kD protein has led to a proposal of a ‘fungal pan allergen’ [5]. Infection is caused due to exposure to airborne conidia. In our patient we assume that he contracted the fungus from his workplace as he is a farmer by occupation and subsequently led to his symptoms. It has to be emphasized that isolation of this fungus from the paranasal sinuses of this patient with rhinosinusitis is very rare upto the extent that only one case has been reported till date [11]. But that was an invasive disease in an immunocompromised host. In humans, there are only few reports of deep infection caused by species of Chrysosporium were reported [12].
AFS has been an increasingly recognized etiology for the refractory chronic sinusitis in an immunocompetent host, analogous to allergic bronchopulmonaryaspergillosis (ABPA), a related process in the lung. Most patients experience relapse in the disease processes despite continued oral or topical corticosteroid therapy and aggressive endoscopic sinus surgery. Controlled trials have shown benefit in treating ABPA with adjunctive antifungal therapy, longterm antifungals has been in use in a young man with remittent AFS, which helps in breaking the cycle of relapsing disease [13-15] . The infection is thought to be susceptible to Amphotericin – B; however standardized values are not yet available. Susceptibility data from previous studies suggest that the organism is susceptible to Amphotericin-B and moderately resistant to Itraconazole [16]. Recent studies have also noted the effectiveness of systemic Voriconazole in Chrysosporium infection [17]. Chrysosporium is a very rare infection which can cause infection in both noninvasive and invasive form and also considering the willingness for the revision surgeries in elderly patient; he was started on intravenous Voriconazole for nine days which proved to be quite effective.
Non contrast Enhanced Computed Tomography scan of Osteomeatal complex showing widening of spheno-ethmoidal recess and soft tissue density in right sphenoid and posterior ethmoid sinuses
Fungal growth on Sabaraoud’s dextrose agar with antibiotics
Lactophenol cotton blue preparation from the culture
Conclusion
Chrysosporium causing fungal sinusitis in an elderly, immunocompetent patient is very rare. In localized, non-invasive form of fungal sinusitis, regardless of the fungus isolated, debridement proves to be the best modality of treatment although systemic antifungals do play an adjuvant role. Even though our patient had good relief with Voriconazole, further studies on susceptibility tests are necessary for rare fungus like Chrysosporium.
[1]. A Masood, I Moumoulidis, J Panesar, Acute rhinosinusitis in adults: an update on current managementPostgrad Med J 2007 83:402-08. [Google Scholar]
[2]. I Brook, Microbiology and antimicrobial management of sinusitisOtolaryngolClin North Am 2004 37(2):253-66. [Google Scholar]
[3]. KW Ah-See, AS Evans, Sinusitis and its managementBMJ 2007 334(7589):358-61. [Google Scholar]
[4]. K Van Crombruggen , N Zhang, P Gevaert, P Tomassen, C Bachert, Pathogenesis of chronic rhinosinusitis: inflammationJ Allergy ClinImmunol 2011 128:728-32. [Google Scholar]
[5]. MS Schubert, Allergic Fungal SinusitisOtolaryngol Clin N Am 2004 37:301-26. [Google Scholar]
[6]. D Glass, RG Amedee, Allergic Fungal Rhinosinusitis: A ReviewThe Ochsner Journal 2011 11(3):271-75. [Google Scholar]
[7]. FA Kuhn, R Swain, Allergic fungal sinusitis: diagnosis and treatmentCurr Opin Otolaryngol Head Neck Surg 2003 11(1):1-5. [Google Scholar]
[8]. BJ Ferguson, Eosinophilicmucinrhinosinusitis: a distinct clinicopathological entityLaryngoscope 2000 110:799-813. [Google Scholar]
[9]. BT Khattar, C Hathiram, Allergic fungal RhinosinusitisOtorhinolaryngol Clin Int J 2009 1:37-44. [Google Scholar]
[10]. BH Bowman, TJ White, JW Taylor, Human pathogenic fungi and their close nonpathogenic relativesMol Phylogenet Evol 1996 6:89-96. [Google Scholar]
[11]. FE Levy, JT Larson, E George, RH Maisel, Invasive Chrysosporium infection of the nose and paranasal sinuses in an immunocompromised hostOtolaryngol. Head Neck Surg 1991 104:384-88. [Google Scholar]
[12]. A Warwick, P Ferrieri, B Burke, BR Blazar, Presumptive invasive Chrysosporium infection in a bone marrow transplant recipientBone Marrow Transplant 1991 8:319-22. [Google Scholar]
[13]. D Andes, R Proctor, RK Bush, TR Pasic, Report of successful prolonged antifungal therapy for refractory allergic fungal sinusitis Clin Infect Dis 2000 31(1):202-04. [Google Scholar]
[14]. K Seiberling, PJ Wormald, The role of itraconazole in recalcitrant fungal sinusitisAm J Rhinol Allergy 2009 23(3):303-06. [Google Scholar]
[15]. CC Khalil, CC Tharwat, CC Abdou, CC Essa, CC Elsawy, HO Elnakib, The role of antifungal therapy in the prevention of recurrent allergic fungal rhinosinusitis after functional endoscopic sinus surgery: a randomized, controlled studyEar Nose Throat J 2011 90(8):E1-7. [Google Scholar]
[16]. E Roilides, L Sigler, E Bibashi, H Katsifa, N Flaris, C Panteliadis, Disseminated infection due to Chrysosporiumzonatum in a patient with chronic granulomatous disease and review of non-Aspergillus fungal infections in patients with this diseaseJ Clin Microbiol 1999 37(1):18-25. [Google Scholar]
[17]. JP Donnelly, BED Pauw, Voriconazole—a new therapeutic agent with an extended spectrum of antifungal activityClinical Microbiology and Infection 2004 10:107-17. [Google Scholar]