Lymph nodes are an important part of immune system. Lymph nodes play a crucial role in tumour progression. Metastases are tumour implants discontinuous with the primary tumour. The characterization of a neoplasm as primary or metastatic has always troubled surgical pathologists. Histological assessment of such lymph node biopsies help to arrive at an appropriate diagnosis, often with the help of advanced techniques like IHC.
Hence, the present study is an attempt to evaluate metastatic lesions in lymph node biopsies with clinico-pathological correlation and special emphasis on IHC in metastatic breast carcinoma.
Materials and Methods
The present study was conducted in the Department of Pathology, M. R. Medical College Gulbarga. It was a 10 year study including 8 year retrospective study and 2 year prospective study (From July 2004- June 2014). A total number of 228 metastatic lymph node biopsies were studied. Cases of lymphadenitis and primary malignancies of lymph node were excluded. All retrospective cases were collected from the departmental records. All cases included specimens sent for histopathology as a part of routine protocol for treatment, pathologic assessment and planning further management. The consent for the same was taken before surgery.
For each case the following parameters were noted: age, sex, size of lymph node, number of lymph nodes received, site of lymph node, site of primary and histological type of malignancy.
All specimens were fixed in 10% formalin solution and paraffin blocks had been prepared which were cut at 4-5 microns thickness. They were subsequently stained with hematoxylin and eosin and evaluated histopathologically. Special techniques like IHC were done only for metastasis of breast carcinoma.
Results
Age of the patients ranged from 16 y to 85 y with a median age of 47.02 y. The youngest patient was 16 y (papillary carcinoma of thyroid) and the oldest was 85 y (IDC). Male to female ratio was 1:2.17 [Table/Fig-1]. Most common site of lymph node with metastasis was axillary that is 77 cases (33.77%) followed by cervical that is 52 cases (22.80%) and pelvic that is 22 cases (9.64%). Female predominance was noted in all sites of lymph node except cervical and iliac nodes.
| Male | % | Female | % | Total | % |
|---|
| <20 years | 00 | 0% | 09 | 3.94% | 09 | 3.94% |
| 21-40 years | 18 | 7.89% | 53 | 23.24% | 71 | 34.14% |
| 41-60 years | 41 | 17.98% | 73 | 32.01% | 114 | 50% |
| >60 years | 13 | 5.70% | 21 | 9.21% | 34 | 14.91% |
| Total | 72 | 31.57% | 156 | 68.42% | 228 | 100% |
Grossly, size of the metastatic lymph nodes varied from 0.5 cm to 4 cm. Out of 228 cases, 42 cases were of single lymph node and the remaining 186 cases were with multiple metastatic lymph nodes. Maximum lymph nodes received in a single case were 9 and all of them showed metastasis. Cut section of the lymph nodes biopsies showed grey white colour in 198 cases.
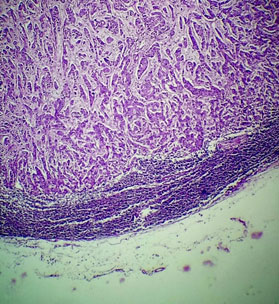
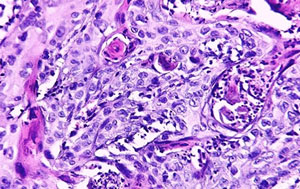
Most of the cases (77 cases; 33.8%) were metastasis of breast carcinoma, out of which 68 were from infiltrating ductal carcinoma (IDC) [Table/Fig-2] and 9 from medullary carcinoma. Next most common histological subtype was squamous cell carcinoma from head & neck, cervix and male genital system [Table/Fig-3]. Among squamous cell carcinoma metastasis of head and neck origin, 44 were non-keratinizing and 3 keratinizing. Those originating from cervix included 18 cases of non-keratinizing squamous cell carcinoma and 1 keratinizing.
Axillary lymph node section showing metastatic deposits of Infiltrating ductal carcinoma of breast [H&E 100x]
Metastatic keratinizing squamous cell carcinoma in cervical lymph node [H&E 400x]
Almost all cases of metastasis from breast malignancies were seen in females except for a single case of IDC in a male. Squamous cell carcinoma metastasis was more common in males mainly attributed to by primaries in head and neck, and male genital tract. Adenocarcinoma metastasis was also more common in males with gastrointestinal tract (GIT) as primary [Table/Fig-4]. Male to female ratio among SCC and adenocarcinoma metastasis cases were statistically significant (p<0.01). Thyroid carcinoma and lung carcinoma metastasis showed predominance among females. However malignant melanoma metastases were equally distributed among males and females [Table/Fig-5].
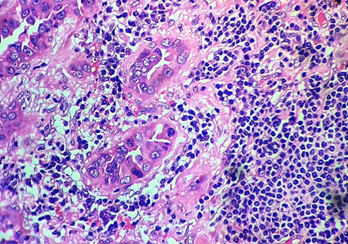
Metastasis of adenocarcinoma [H&E 400x]
Site of primary and histological subtype of metastasis
| Primary | Histological type | Males | Females | No | % |
|---|
| Breast | Infiltrating duct cell carcinoma | 1 | 67 | 77 33.77% |
| Medullary Ca of Breast | - | 9 |
| Head & Neck | Cheek | Squamous cell carcinoma | 6 | 5 | 11 | 4.82% |
| Tongue | Squamous cell carcinoma | 13 | 6 | 19 | 8.33% |
| Larynx | Squamous cell carcinoma | 3 | 3 | 6 | 2.63% |
| Skin | Squamous cell carcinoma | 3 | 1 | 4 | 1.75% |
| Pharynx | Squamous cell carcinoma | 3 | 2 | 5 | 2.19% |
| Shoulder | Malignant Melanoma | 2 | - | 2 | 0.87% |
| Neck | Malignant Melanoma | 2 | - | 2 | 0.87% |
| Thyroid | Follicular Ca of Thyroid | - | 6 | 16 | 7.01% |
| Papillary Ca of Thyroid | 4 | 6 |
| Gastrointestinal tract | Stomach | Adeno Ca | 8 | 1 | 9 | 3.94% |
| Colon | Adeno Ca | 14 | 4 | 18 | 7.89% |
| Anorectal | Malignant Melanoma | - | 5 | 7 | 3.07% |
| Adeno Ca | 1 | 1 |
| Foot | Malignant Melanoma | 3 | 2 | 5 | 2.19% |
| Male Genital Tract | Penis | Squamous cell carcinoma | 6 | - | 6 | 2.63% |
| Female genital tract | Ovary | Adeno Ca | - | 13 | 32 | 14.03% |
| Cervix | Squamous cell carcinoma | - | 19 |
| Lung | Non-small cell Ca of Lung | 1 | 2 | 9 | 3.94% |
| Small cell ca of Lung | 2 | 4 |
| TOTAL | 72 | 156 | 228 | 100% |
Majority of cases showed metastasis to axillary lymph node from mainly IDC that is 68 cases followed by 9 cases of medullary carcinoma of breast. Cervical lymph node metastasis was mainly of squamous cell carcinoma in 28 cases followed by thyroid carcinoma in 16 cases. Pelvic and pyloric lymph node metastasis had an equal distribution of squamous cell carcinoma and adenocarcinoma metastasis. Most of the malignant melanoma metastases were to cervical, inguinal and mesenteric lymph nodes (4 cases each) followed by iliac (2 cases). The group of lymph nodes that were least involved by metastasis were obturator and paraaortic (5 each) [Table/Fig-6].
Site of metastasis with histological subtype of primary
| | IDC | SCC | Adeno Ca | Thyroid Ca | Medullary Ca of breast | Malignant Melanoma | Lung Ca | Total | Percentage |
|---|
| 1) | Axillary | 68 | | | | 09 | | | 77 | 33.8% |
| 2) | Cervical | | 28 | | 16 | | 04 | 04 | 52 | 22.8% |
| 3) | Pelvic | | 11 | 11 | | | | | 22 | 9.7% |
| 4) | Inguinal | | 09 | 08 | | | 04 | | 21 | 9.2% |
| 5) | Mesenteric | | 06 | 02 | | | 04 | | 12 | 5.2% |
| 6) | Supraclavicular | | 06 | | | | | 05 | 11 | 4.8% |
| 7) | Iliac | | 05 | 06 | | | 02 | | 13 | 5.7% |
| 8) | Obturator | | 01 | 04 | | | | | 05 | 2.3% |
| 9) | Pyloric | | 05 | 05 | | | | | 10 | 4.4% |
| 10) | Para aortic | | 01 | 04 | | | | | 05 | 2.1% |
| Total | 68 | 72 | 40 | 16 | 09 | 14 | 09 | 228 | 100% |
For 60 cases of breast carcinoma metastasis, IHC was done. Out of which, 27 (45.00%) were ER positive, 25 (41.67%) were PR positive and 23 (38.33%) were HER2/neu positive [Table/Fig-7]. These results correlated with the expression in primary breast carcinoma. Among these 60 cases, 56 were IDC and 4 were medullary carcinoma metastasis. Majority of IDC cases were ER negative (51.79%), PR negative (55.36%) and HER2/neu negative (58.93%). All the 4 cases of Medullary carcinoma metastasis were ER/PR negative and HER2/neu negative [Table/Fig-8,9,10,11].
Distribution of breast carcinoma metastasis according to expression of er, pr and her2/neu.
| Marker | No. of cases (n=60) | Percentage |
|---|
| ER |
| Positive | 27 | 45.00% |
| Negative | 33 | 55.00% |
| PR |
| Positive | 25 | 41.67% |
| Negative | 35 | 58.33% |
| HER2/neu |
| Positive | 23 | 38.33% |
| Negative | 37 | 61.67% |
Distribution of breast carcinoma metastasis according to immunohistochemical expression of histological subtypes of the primary.
| IDC (n=56) | Medullary (n=4) |
|---|
| ER Positive | 27 (48.21%) | 0 (0.00%) |
| ER Negative | 29 (51.79%) | 4 (100.00%) |
| PR Positive | 25 (44.64%) | 0 (0.00%) |
| PR Negative | 31 (55.36%) | 4 (100.00%) |
| HER2/neu Positive | 23 (41.07%) | 0 (0.00%) |
| HER2/neu Negative | 33 (58.93%) | 4 (100.00%) |
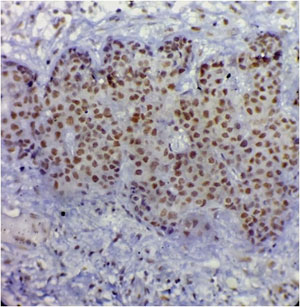
ER nuclear positivity in metastasis of breast carcinoma
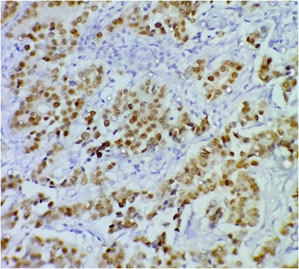
PR nuclear positivity in metastasis of breast carcinoma
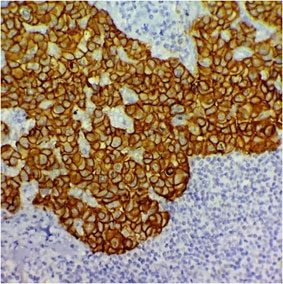
Her2/neu membrane positivity within the metastatic breast carcinoma lesion
Discussion
Lymph nodes play essential role in the control of tumour progression. Lymph node may act as efficient barriers and destroy the invading tumour cells or stop dissemination. Within the lymph nodes, the metastatic tumour cells first appear in the marginal sinus, from which they penetrate the medullary sinuses, the medulla, and the cortex eventually resulting in total parenchymal replacement. Lymph node metastasis presents the best opportunity for primary tumour diagnosis through biopsy and histologic evaluation [1].
In the present study, a total number of 228 cases were studied over a period of 10 years (2004 to 2014). Taking age into consideration the relative incidence of metastatic lesions of the lymph node was gradually increasing through age, peaking during 4th to 6th decade. The maximum number of cases was from the age group of 41-60 years with a mean age of 47.02, which correlates with the study of V. Popat et al., [2], Naeimi et al., [3], Sinha et al., [4] and Laxman [5]. Present study showed female predominance because majority of patients were of breast carcinoma in females, while other studies showed male predominance.
The anatomic location of a lymph node with metastasis provides an important indication of the primary site of its origin. The dominant site of metastasis was in the axillary lymph node in our study which correlated with study by Laxman [5] [Table/Fig-12]. The most common primary site of malignancy was breast (33.77%), which is comparable to the study done by Shamshad et al., [6] (22.21%) and Laxman [5] (54.39%). The preponderance of involvement of various sites of metastasis differed in both sexes. Most common site of metastasis in male was cervical lymph node while it was axillary lymph node in females. Most common site of primary in males was head and neck while in females it was breast.
Comparison with other studies
| Author / Year | | Total cases |
|---|
| Axillary | Cervical | Inguinal |
|---|
| Sinha et al., (2003) | 5.43% | 17.39% | 5.43% | 92 |
| Laxman (2008) | 47.8% | 15.2% | - | 114 |
| Shamshad et al., (2011) | 27.11% | 56.51% | - | 171 |
| Present Study (2014) | 33.77% | 22.81% | 9.2% | 228 |
Based on histopathology, a total number of 77 metastatic breast carcinomas were noted. 68 of the lymph node deposits showed IDC and 9 showed medullary carcinoma of breast. Apart from that, 72 cases were from squamous cell carcinoma followed by adenocarcinoma 40 cases and malignant melanoma 14 cases.
Squamous cell carcinoma mainly metastasized to cervical lymph nodes followed by pelvic (11 cases) and inguinal (9 cases). Laxman [5] found squamous cell carcinoma in 23.68% of cervical lymph nodes with metastasis, while Gautam et al., [7] found in 8.5%. In the present study 12.28% of lymph node metastasis was of squamous cell carcinoma within cervical lymph node. Most common primary site was oral cavity in the cheek which correlates with Gautam et al., [7] and Sabeti et al., [8] while in Shamshad et al., [6] study oropharynx was the most common primary site.
Adenocarcinoma mainly metastasized to pelvic lymph nodes and histologically revealed signet ring pattern of gastric carcinoma and glandular pattern with large mucus secreting cells of rectosigmoid carcinoma. The most common primary site was colon which correlates with the study by Gautam et al., [7]. Incidence of metastasis from GIT, lung and female genital tract in our study correlated with the study by Shamshad et al., [6] and Laxman [5]. Metastases from thyroid cancer were seen in 7.01% cases in which also correlates with study of Naeimi et al., [3] and Laxman et al., [5]. Most of the cases were seen predominantly in females with mean age of 48 which correlated with the study of Nobuyuki et al., [9].
Surgical treatment of breast carcinoma most commonly practised is modified radical mastectomy with axillary lymph node dissection. In this study, out of 185 mastectomy specimen, 41.67% cases were associated with axillary lymph node metastasis. This correlated with other Indian and international studies [10–15]. In view of rising incidence of breast cancer in India, a thorough assessment of mastectomy and axillary lymph node biopsies is essential. Routine histopathology is insufficient to predict prognosis and response to therapy in breast carcinoma. Thereby, specialised techniques like IHC play an important role in making therapeutic decisions.
IHC was done in 60 cases of metastatic breast carcinoma in this study. ER, PR and HER2/neu expression was negative in majority of cases which correlated with other Indian studies by Kuraparthy et al., [16] and Verma et al., [10]. International studies were showing hormone receptor positivity and HER2/neu negativity [11–13]. Immunohistochemical expression of lymph node metastasis from IDC cases were mainly ER, PR and HER2/neu negative. The four cases of metastasis from medullary carcinoma were also negative for the triple markers. Similar observation was made by Nadji et al., [17].
Conclusion
The present study helps in understanding the patterns of distribution of metastasis in North Karnataka region, among different groups of lymph node with the primary site of malignancy and histological type. Precise detection of metastasis and histological subtype of the primary, aids in staging and making treatment decisions. Use of ancilliary techniques like immunohistochemistry helps in a more comprehensive study of metastatic lesions especially in metastatic breast carcinoma, where it plays a role in accurate assessment of prognosis and therapeutic response.