Background: Image intensifiers have become popular due to the concept of minimally invasive surgeries leading to decreasing invasiveness, decreased operative time, and less morbidity. The drawback, however, is an increased risk of radiation exposure to surgeon, patient and theatre staff. These exposures have been of concern due to their potential ability to produce biological effects. The present study was embarked upon to analyse the amount of radiation received by orthopedic surgeons in India using standard precautionary measures and also to bring awareness about the use of image intensifier safety in everyday practice.
Materials and Methods: Twelve right-handed male orthopedic surgeons (4 senior consultants, 5 junior consultants and 3 residents) were included in a three month prospective study for radiation exposure measurement with adequate protection measures in all procedures requiring C Arm fluoroscopy. Each surgeon was provided with 5 Thermo Luminescent Dosimeter (TLD) badges which were tagged at the level of neck, chest, gonads and both wrists. Operative time and exposure time of each procedure was recorded. Exposure dose of each badge at the end of the study was obtained and the results were analysed.
Results: Mean radiation exposure to all the parts were well within permissible limits. There was a significantly positive correlation between the exposure time and the exposure dose for the left wrist (r=0.735, p<0.01) and right wrist (r=0.58, p<0.05). The dominant hand had the maximum exposure overall.
Conclusion: Orthopaedic surgeons are not classified radiation workers. The mean exposure doses to all parts of the body were well within permissible limits. Nothing conclusive, however, can be said about the stochastic effects (chance effects like cancers). Any amount of radiation taken is bound to pose an additional occupational hazard. It is thus desirable that radiation safety precautions should be taken and exposures regularly monitored with at least one dosimeter for monitoring the whole-body dose.
Introduction
The use of fluoroscopy has increased tremendously in field of orthopedics. The image intensifiers have enabled orthopedic surgeons to become technically more proficient and decrease the morbidity of the patient by minimizing area of operative field and decreasing operative time [1].
Fluoroscopy has been used and abused. Some overuse it forgetting the principles of radiation protection while others underuse it due to unfounded fears. In general, orthopedic surgeons lack awareness about the radiation exposure they are getting and its effects on health and are callous with protection [2]. Surgeons and assistants are at maximum risk among all OT personnel due to proximity to exposure area. Some studies concluded that whole body dose received is well within recommended levels but have emphasized caution due to long term effects of even low dose radiation [3]. It is pertinent that any amount of exposure to ionizing radiation leading to secondary occupational risk should be avoided or maximal caution exercised to minimize the exposure.
There have been few studies evaluating the dose of radiation received by orthopaedic surgeons worldwide [4-8] and none from the Indian subcontinent. The present study was embarked upon to analyse the amount of radiation received by orthopedic surgeons in India using standard precautionary measures and also to bring awareness about the use of image intensifier safety in everyday practice.
Materials and Methods
A three month prospective study (Level II) was conducted at our institute from January 2002 to March 2002 with prior ethical committee approval. Twelve right-handed male orthopedic surgeons (4 senior consultants, 5 junior consultants and 3 residents) were included for the study.
All procedures requiring C Arm fluoroscopy were included in the study while those done only under radiographic control were excluded. The portable C-Arm fluoroscope with image intensifier used for the procedures was Stenoscope Plus 9000 (GE).
Each surgeon was provided with 5 Thermo-luminescent Dosimeter (TLD) badges [Table/Fig-1] obtained from Department of Radiological Physics, Bhaba Atomic Research Centre (BARC), Mumbai, India after approval of their personal data from the agency. The 1st badge was worn anteriorly over the neck under the thyroid guard and measured radiation exposure to the neck and thyroid region. The 2nd badge was placed at the chest level under the lead apron of 0.5mm lead equivalent thickness and measured exposure to chest, body organs and approximately 80% of active marrow [4]. The 3rd badge was worn over the gonads and measured the gonadal dose. The 4th and 5th badges were worn over the dorsum of left and right wrist in between two gloves for measuring the exposure to hands [Table/Fig-2]. After the surgical procedure was over, the TLD badges were stored in small boxes (with formalin tablets for the wrist) in lockers away from the operating room. Control TLD badge was stored in a similar box and kept in the same locker to estimate the environmental radiation.
A record was kept for duration of surgery and fluoroscopy exposure time. TLD badges were sent to BARC for measurement of radiation exposure.
The results were analysed using the student t-test and correlation coefficients.
Results
Average age of the subjects was 36.83 y. There were 147 procedures where C arm was used. Senior consultants on an average operated in 9 cases per subject where C arm was used, junior consultants operated or assisted in 12.8 cases per subject and residents assisted in 15.67 cases per subject. Most common procedure was interlocking nailing femur, which also had the maximum mean operative time (02:32:33 h/case) as well as maximum mean exposure time (0:04:09). There was a significant positive correlation between the mean operative time and mean exposure time for all procedures (r-value = 0.803, p-value<0.05). Closed reduction and interlock nailing had significantly higher exposure times than open procedures and percutaneous procedures [Table/Fig-3].
The mean exposure doses (in mSV) are given in [Table/Fig-4] which when extrapolated is well within permissible limits of International Council for Radiation Protection (ICRP) [9]. Right wrist (dominant hand) had the maximum mean exposure dose followed by left wrist, neck, chest and gonads.
There was a significantly positive correlation between the exposure time and the exposure dose for the left wrist (r=0.735, p<0.01) and right wrist (r=0.58, p<0.05) while it was not significant for the Protectionneck, chest and gonads. There was no significant difference in the exposures to the dominant and nondominant hand of the surgeons and assistants [Table/Fig-5].
Discussion
Orthopaedic surgeons and assistants are at the maximum radiation risk among all OT personnel due to proximity to exposure area [10]. This study was conducted in an attempt to analyse the radiation doses received by orthopaedic surgeons in an Indian setup as no such study has been done previously. An attempt is also being made to promote radiation protection awareness and the safe use of radiation in the operation theatre.
There was a significantly positive correlation between operative time and exposure time. In general, closed reduction and interlocking nailing procedures were associated with a higher exposure time in comparison to open procedures and percutaneous procedures/ closed reductions and cast. This was similarly highlighted by other authors [6,11]. This is not surprising considering that in closed reduction and interlock nailing of long bone fractures the soft tissue mass is more and poses greater difficulty for reduction. Added exposure time is also required for the locking procedure as well [12].
The importance of ionizing radiation stems from its ability to produce biologic damage. The effects of radiation can be divided into dose-dependent (non stochastic) or dose-independent (stochastic) [2]. Our study indicates that the greatest exposure to the surgeon is in the areas of the extremities and the head and neck as was also reported by others [4,5]. In terms of radio biologic effects, it would pertain to development of cataracts, alteration of thyroid function and induction of skin cancers. The amount of radiation received at level of chest and gonads was found to be negligible. The protection offered at the level of the chest documents the effectiveness of the standard lead apron (5mm thick). It provides good shielding to approximately 82% of active bone marrow [4]. The gonadal dose received was also very less thereby allaying the fears of potential adverse effects to progeny. It was estimated by Theocharopoulos N et al., that the genetic risk for orthopaedic surgeon after 10 y of occupational exposure to be 16,000 times lower than the natural frequency of heritable disease [8].
Right (dominant) wrist received the maximum exposure out of all the body parts where badges were attached. This may be due to increased exposure to the dominant hand of the surgeon which is closer to the image intensifier during a procedure and thus is in more proximity to the radiation. There was no significant difference in the exposures to the dominant and nondominant hand of the surgeons and assistants as was the case in the study by Sanders R et al., [6].
There was a significantly positive correlation between exposure time and exposure doses for the left wrist and right wrist. Sanders R et al., too found an increase in the exposure dose of the extremities with exposure time [6]. In his series, Miller [5] found more exposure to the head and neck area, possibly because the subjects received more scatter radiation, or the dosimeter to measure the neck dose was outside the thyroid shield (not mentioned).
The exposure to the surgeons and assistants in our series was well within ICRP limits as was the case with other series [1,3,5,13]. This will only reduce the non stochastic effects. On the other hand nothing conclusive can be said about the stochastic or chance effects like cancers. Many authors have suggested a significantly increased risk of cancer incidence among orthopedic surgeons [4,7,14].
The amount of radiation received cannot be made nil but can be minimized by using the ALARA (As low as reasonably achievable) principle [15]. The amount of radiation exposure depends on the following variables which can be modified to minimize radiation exposure.
a. Personal Protection
a. Shielding – All personnel should wear protective gear [1,4]. Lead aprons help in reducing the exposure by a factor of 4 in lateral view and a factor of 16 in postero-anterior view. Thyroid guards decrease the exposure 2.5 times the normal. Eye protection is essential and is the first determinant of workload in all procedures. Lead apron should have at least 0.5mm equivalent thickness of lead and the goggles should be at least 0.15 mm lead equivalent thick [7].
b. Distance – The intensity of radiation at a point is inversely proportional to the square of distance.
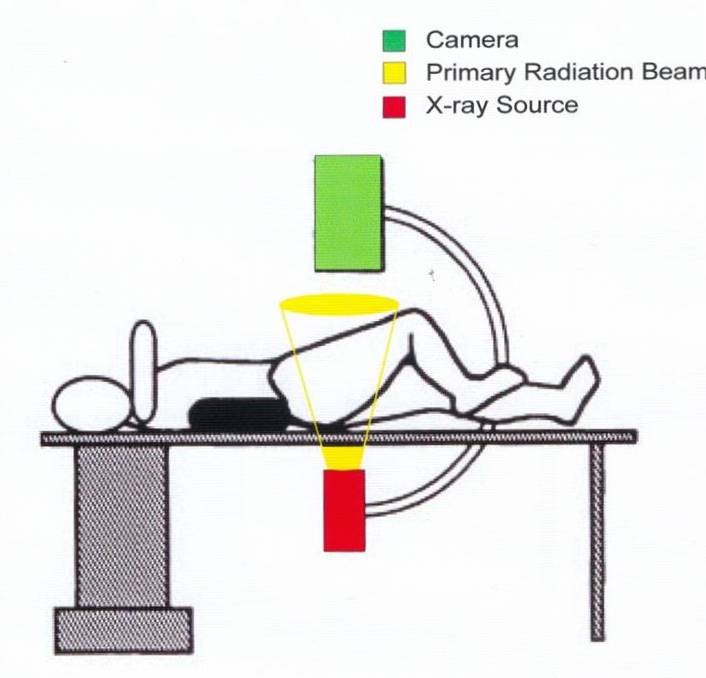
i. Gachiano et al., [16] had shown that average amount of radiation received at 18 inches from primary beam was only 0.1% of that measured directly over femoral head [Table/Fig-6]. The surgeon and his team must maintain a minimum distance of 18 inches from this zone of primary beam to avoid ill effects of direct beam radiation.
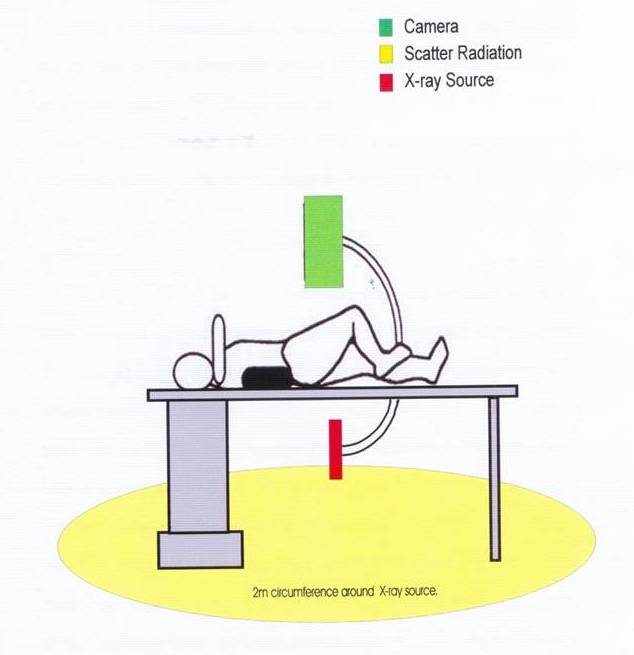
ii. Alonso et al., [17] concluded that the scatter radiation outside 2 meter zone of a C Arm unit is less than 1 mSv [Table/Fig-7]. Within 2 metre of the C Arm unit, the lead protection is a must.
b. Personnel related factors
a. Technical proficiency – Surgeons should be familiar with the procedure, the technique and the instrumentation. Effort should be to supplement image to the clinical knowledge and not vice versa [2]. Some studies have reported that more the experience lesser is the exposure [13,18].
b. Adequately trained operator – will avoid unnecessary exposures.
c. Personnel monitor – Routinely radiation dose meters should be worn by all persons working in or near radiation fields.
d. Staff training – Many of the surgeons and staff are callous towards radiation protection. It has been a personal experience that many persons do not wear thyroid shields. Theocharopoulos et al., [7] concluded that the use of thyroid protection leads to a further 2.5- fold decrease of radiation dose than without thyroid protection. All staff should undergo a regular orientation programme towards radiation protection.
c. Procedure related factors
a. Duration of Exposure – The lesser the exposure time, the lesser the exposure dose and the radiation side effects.
i. Well-planned procedure – The procedure should be well planned with job descriptions clearly marked out prior to surgery so as to minimize the time of exposure.
ii. Intermittent Fluroscopy – 3 sec burst with ‘long off’ interval is preferable. Continuous fluoroscopy should be avoided [6,11].
iii. Pulse Mode – decreases radiation dose by 70% [2].
iv. Image Capture and Memory Storage – allows study of the image by the surgeon without re-exposure to the patient.
b. Avoid direct handling of x-ray tube while in operation and placement of the hand directly in the radiation beam.
c. Position of the C Arm - The intensity of scatter radiation is the maximum in backward direction in orthopaedic procedures. The amount of scatter radiation to the surgeon is maximum in horizontal fluoroscopy and that is why it was proposed that the beam should be directed from medial to lateral direction [16,19]. This is not what the norm is due to the construction of the C Arm. We suggest a change in design of the C Arm interchanging the positions of the X-ray tube and the camera unit. In the postero-anterior imaging, the beam should be directed from posterior to anterior [16].
d. Collimation – reduces the beam area and enhances contrast, thereby decreasing the radiation dose to the surgeon and other staff [1].
e. Exposure Time Alarm – would warn the surgeon and the operator of the amount of radiation exposure received.
d. Equipment related factors
a. Quality of machine – the whole assembly of the unit should meet CRP/AERB/BARC recommendations [2].
b. Mini Carm Units may produce lesser radiation hazard than normal C Arm Units [1].
c. Maintenance of equipment and protective shields -
i. A decrease in efficiency of the C Arm unit is compensated by increased exposure to get similar brightness and contrast of imaging. Amount of radiation delivered varies by more than a 100% in more than 30% of the machines at one year interval. It is therefore desirable to have a half yearly quality assurance with regards to the output of radiation and system resolution of all units.
ii. Protective shields should be properly stored (not folded as it breaks the lead in it). They should also be routinely checked and faulty pieces either repaired or discarded.
iii. TLD badges used for monitoring may be stored in Lead Boxes [20].
TLD Badges used were obtained from Bhaba Atomic Research Centre

Positioning of the TLD Badges

Difference between exposure times of closed versus open versus percutaneous procedures
| Mean exposure time per case (hh:mm:ss) | t-value | p-value |
|---|
| Closed reduction and nailing procedures | 0:03:31 | Closed vs open – 2.27 | p<0.05 (S) |
| Open procedures | 0:02:29 | Closed vs percut – 3.85 | p<0.005 (S) |
| Percutaneous procedures | 0:01:47 | Open vs percut – 1.5 | p<0.1 (S) |
Cumulative mean exposure dose to various body parts of all the surgeons
| Neck | Chest | Gonads | Right wrist | Left wrist |
|---|
| Mean exposure per subject (mSv) | 0.328 | 0.17 | 0.15 | 0.73 | 0.58 |
| Extrapolated mean annual exposure per subject (mSv) | 1.312 | 0.68 | 0.60 | 2.92 | 2.32 |
| ICRP limits (mSv) | 150 | 20 | 20 | 500 | 500 |
mSv = milli Sieverts, ICRP = International Council of Radiation Protection
Comparison of right and left wrist dosage for senior consultants versus junior consultants versus residents
| Mean right wrist Exposure (mSv) | Mean left wrist Exposure (mSv) | Mean difference of exposure of right vs left wrist (mSv) | t-value | p-value |
|---|
| Senior Consultants | 0.637 | 0.37 | 0.267 | 1.703 | p>0.1 (NS) |
| Junior Consultants | 1 | 0.838 | 0.162 | 0.849 | p>0.1 (NS) |
| Residents | 0.401 | 0.435 | -0.143 | -1.639 | p>0.1 (NS) |
mSv = milli Sieverts, ICRP = International Council of Radiation Protection
Zone of Primary Beam radiation: adapted from Gachiano et al., [16] who had shown that average amount of radiation received at 18 inches from primary beam was only 0.1% of that measured directly over femoral head
Zone of Scatter radiation is at the back of the X-ray tube: Alonso et al., [17] concluded that the scatter radiation outside 2 meter zone of a C Arm unit is less than 1 mSv
Conclusion
To summarize, the total amount of radiation exposure during fluoroscopy does not exceed the recommended levels. It implies decreased chances of dose dependent effects, but stochastic (chance) effects like cancers can still occur. Orthopaedic surgeons are not classified radiation workers. Radiation exposure is thus an additional secondary occupational hazard in addition to the hazards of other surgical fields. It should hence be a concern for orthopedic surgeons. Radiation safety precautions should be taken and exposures regularly monitored with at least one dosimeter for monitoring the whole-body dose. Radiation safety programs should be routinely conducted.
mSv = milli Sieverts, ICRP = International Council of Radiation Protection
mSv = milli Sieverts, ICRP = International Council of Radiation Protection
[1]. BL Badman, L Rill, B Butkovich, M Arreola, RAV Griend, Radiation Exposure with Use of the Mini-C-Arm For Routine Orthopaedic Imaging ProceduresJ Bone Joint Surg Am 2005 87(1):13-17. [Google Scholar]
[2]. JK Jain, RK Sen, SC Bansal, ON Nagi, Image intensifier and the orthopedic surgeonInd J Orthop 2001 35(2):13-9. [Google Scholar]
[3]. G Singer, Occupational radiation exposure to the surgeonJ Am Acad Orthop Surg 2005 13(1):69-76. [Google Scholar]
[4]. TP Barry, Radiation exposure to an orthopedic surgeonClin Orthop 1984 182:160-64. [Google Scholar]
[5]. ME Miller, ML Davis, CR MacClean, JG Davis, BL Smith, JR Humphries, Radiation exposure and associated risks of operating room personnel during use of fluoroscopic guidance for selected orthopedic surgical proceduresJ Bone Joint Surg 1983 65:1-4. [Google Scholar]
[6]. R Sanders, KJ Koval, T DiPasquale, G Schmelling, S Stenzler, E Ross, Exposure of the orthopaedic surgeon to radiationJ Bone Joint Surg Am. 1993 75(3):326-30. [Google Scholar]
[7]. N Theocharopoulos, K Perisinakis, J Damilakis, G Papadokostakis, A Hadjipavlou, N Gourtsoyiannis, Occupational exposure from common fluoroscopic projections used in orthopaedic surgeryJ Bone Joint Surg Am 2003 85:1698-703. [Google Scholar]
[8]. N Theocharopoulos, J Damilakis, K Perisinakis, K Papadokostakis, A Hadjipavlou, N Gourtsoyiannis, Image-guided reconstruction of femoral fractures: is the staff safe?Clin Orthop Relat Res. 2005 (430):182-88. [Google Scholar]
[9]. J Valentinm, The 2007 Recommendations of the International Commission on Radiological ProtectionICRP publication 103. Ann ICRP 2007 37(2-4):1-332. [Google Scholar]
[10]. D Herscovici, RW Sanders, The effects, risks and guidelines for radiation use in orthopedic surgery Clin Orthop 2000 375:126-32. [Google Scholar]
[11]. DG Jones, J Stoddart, Radiation use in the orthopaedic theatre: a prospective auditAust N Z J Surg 1998 68(11):782-84. [Google Scholar]
[12]. PE Levin, RW Schoen, BD Browner, Radiation exposure to the surgeon during closed interlocking intramedullary nailingJ Bone Joint Surg Am 1987 69:761-66. [Google Scholar]
[13]. R Botchu, K Ravikumar, Radiation exposure from fluoroscopy during fixation of hip fracture and fracture of ankle: Effect of surgical experienceIndian J Orthop 2008 42(4):471-73. [Google Scholar]
[14]. L Brateman, Radiation safety considerations for diagnostic radiology personnelRadiographics 1999 19(4):1037-55. [Google Scholar]
[15]. Mastrangelo Giuseppe, Fedeli Ugo, Fadda Emanuela, Giovanazzi Angelo, Scoizzato Luca, Saia Bruno, Occupational Medicine 2005 55:498-500. [Google Scholar]
[16]. AA Giachino, M Cheng, Irradiation of the surgeon during pinning of femoral fracturesJ Bone Joint Surg Br 1980 62-B(2):227-29. [Google Scholar]
[17]. JA Alonso, DL Shaw, A Maxwell, GP McGill, GC Hart, Scattered radiation during fixation of hip fractures. Is distance alone enough protection? J Bone Joint Surg Br 2001 83(6):815-18. [Google Scholar]
[18]. MJ Oddy, CH Aldam, Ionising radiation exposure to orthopaedic trainees: the effect of sub-specialty trainingAnn R Coll Surg Engl 2006 88(3):297-301. [Google Scholar]
[19]. JD Lester, S Hsu, CS Ahmad, Occupational Hazards Facing Orthopedic SurgeonsAm J Orthop 2012 41(3):132-39. [Google Scholar]
[20]. EP Lácio, AA Ribeiro, BM Gavassi, GG Di Stasi, JA Galbiatti, AD Junior, Exposure of the surgical team to ionizing radiation during orthopedic surgical proceduresRev Bras Ortop 2014 49:227-32. [Google Scholar]