Vanishing Roots: First Case Report of Idiopathic Multiple Cervico–Apical External Root Resorption
Priyadarshini Choudhury1, Rajat G. Panigrahi2, Maragathavalli3, Antarmayee Panigrahi4, Padma Charan Patra5
1 Associate Professor, Department of Oral Medicine & Radiology, Kalinga Institute of Dental Sciences, Kiit University, Odisha, India.
2 Associate Professor, Department of Oral Medicine & Radiology, Institute of Dental Sciences, Soa University, Odisha, India.
3 Professor & Hod, Department of Oral Medicine & Radiology, Saveetha Dental College, Saveetha University, Chennai, India.
4 Assistant Professor, Department of Pediatric & Preventive Dentistry, Institute of Dental Sciences, Soa University, Odisha, India.
5 Assistant Professor, Department of Ear, Nose and Throat, Great Eastern Medical School, Srikakulam, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajat G. Panigrahi, N – 5 / 24, IRC Village Bhubaneswar, Odisha-751015, India. E-mail : emaidrrajat@gmail.com
Idiopathic root resorption is a very rare phenomenon. Resorption in tooth is brought about by odontoclastic activity. Special mechanisms in the periodontal ligament exist to prevent mineralization of the periodontal ligament and these periodontal ligament cells produce factors that inhibit mineralized tissue resorption and are capable of regulating bone and cementum formation. When this mechanism is disturbed it manifests in resorption of root structure. This case report is of a 28-year-old male with a very rare phenomenon where external resorption of both cervical and apical portion of root of multiple teeth was observed and it is documented for the first time.
Multiple external root resorption, Periodontal ligament, Permanent teeth
Case Report
A 28-year-old male patient reported to the Department of Oral Medicine and Radiology, Saveetha University (Chennai, India) with a chief complaint of mobility of teeth in upper and lower jaw and gingival enlargement for past two months. He gave history of loss of front teeth in both jaws and gradual enlargement of gingival since then. [Table/Fig-1] showing the partially edentulous maxilla and mandible along with the gingival enlargement. [Table/Fig-2] showing the extent of mobility of 12.
Showing the partially edentulous maxilla and mandible along with the gingival enlargement

Showing the extent of mobility of 12

There was no history of trauma and his past medical and family histories were unremarkable. No history of any medicine, to relate the gingival enlargement or any other factor, could be ascertained. Haematological and biochemical screening like Differential Count, Erythrocyte Sedimentation Rate, Hb%, Serum Calcium, Serum Potassium, Alkaline Phosphatase, T3, T4, TSH were within the normal range. Intraoral examination revealed poor oral hygiene and grade III mobility of 11, 12, 41 and 42. Gingival enlargement was not beyond the middle third of the crown with no secondary changes, so the gingival changes could not be held responsible for malocclusion or any occlusal stress causing resorption of the teeth, as seen in the region of 21, 22, 31 and 32. The patient had class II molar occlusion with increased overjet and overbite. The crowns of maxillary and mandibular teeth did not exhibit any morphological alteration. The involved teeth responded within normal limits to both electrical and heat pulp tester.
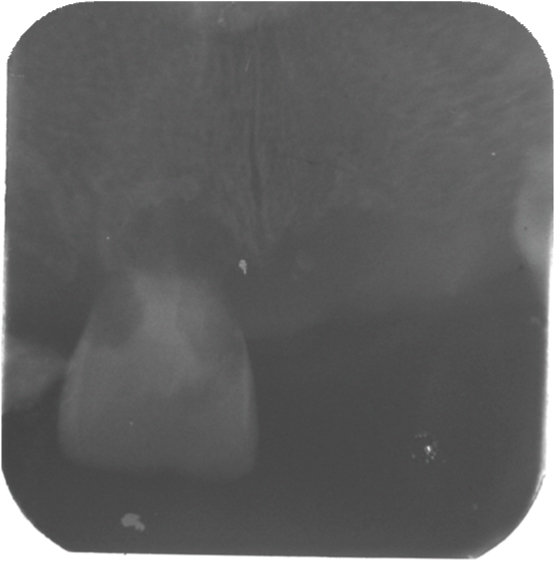
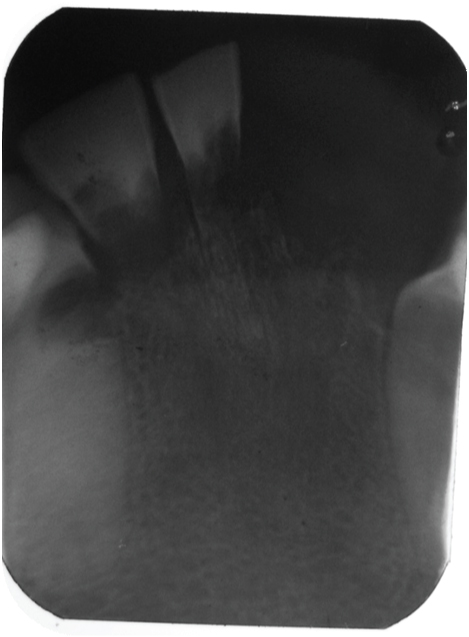
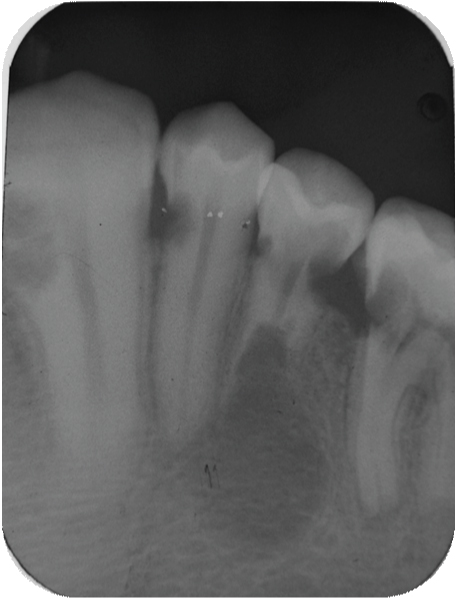
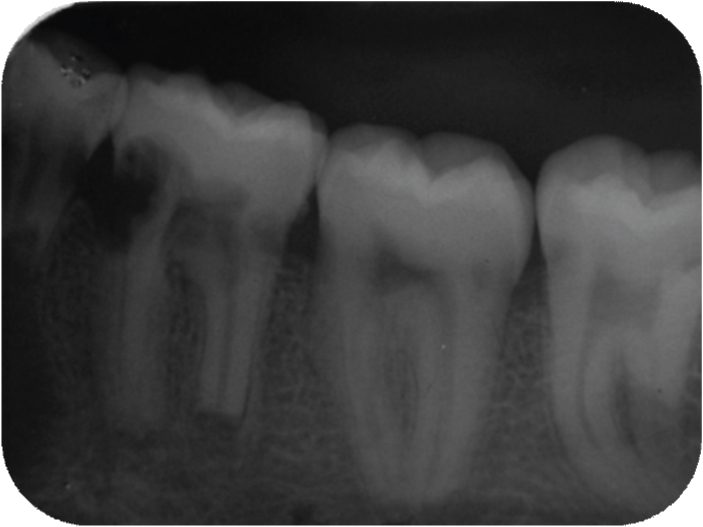
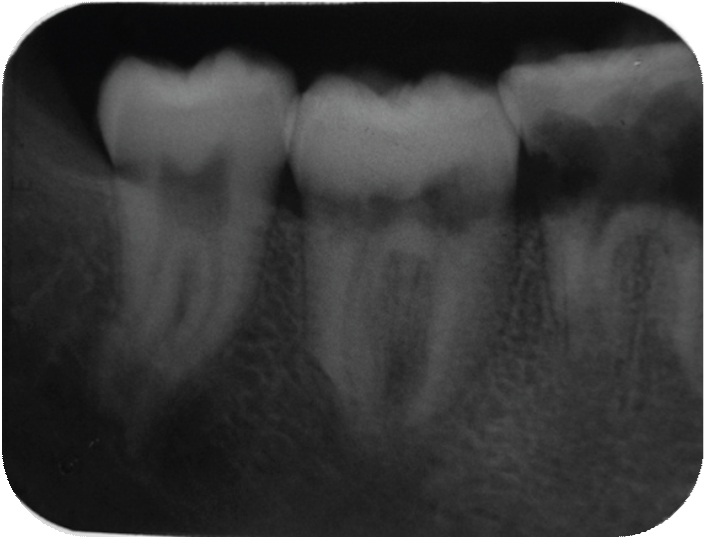
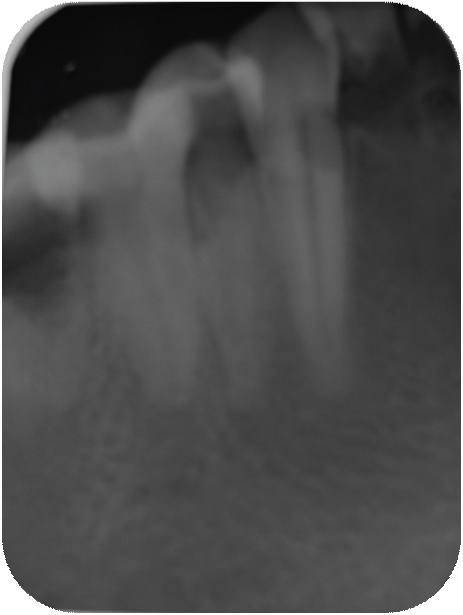
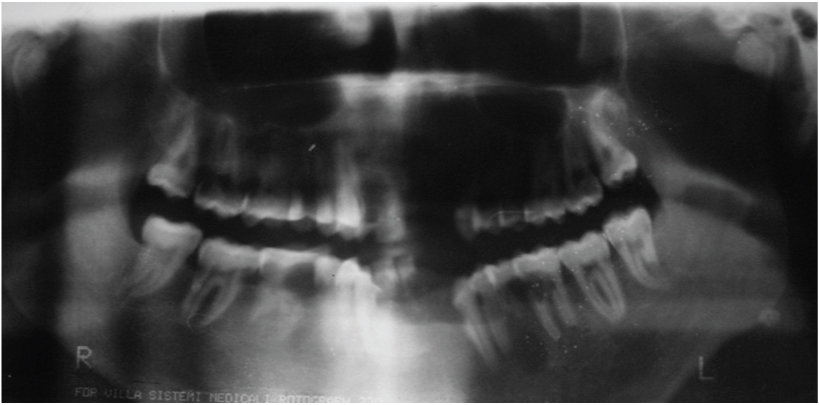
[Table/Fig-3] showing the normal morphology of crowns of the maxillary teeth. [Table/Fig-4] showing the normal morphology of crowns of the mandibular teeth. Full mouth intraoral periapical radiograph revealed complete root resorption in relation to 11, 12, 41 and 42; cervical resorption in 15, 33, 34 and 43, 44; apical resorption in 16, 24, 25 and 26. Resorption in both apical and cervical region was noticed in relation to 35, 36 and 46. Panoramic radiographs showed multiple ill defined radiolucent areas in apical third and cervical region of all teeth in varying degree. Lateral view of skull showed no evidence of any skull changes. In [Table/Fig-5] intraoral periapical radiograph showing complete root resorption in relation to 11 and 12. In [Table/Fig-6] intraoral periapical radiograph showing complete root resorption in relation to 41 and 42. In [Table/Fig-7] intraoral periapical radiograph showing cervical resorbtion in relation to 15 and apical root resorption of mesial and distal roots in relation to 16. Loss of PDL space in 17 can be appreciated.
Showing the normal morphology of crowns of the maxillary teeth

Showing the normal morphology of crowns of the mandibular teeth

Intraoral periapical radiograph showing complete root resorption in relation to 11 and 12
Intraoral periapical radiograph showing complete root resorption in relation to 41 and 42
Intraoral periapical radiograph showing cervical resorbtion in relation to 15 and apical root resorption of mesial and distal roots in relation to 16. Loss of PDL space in 17 can be appreciated

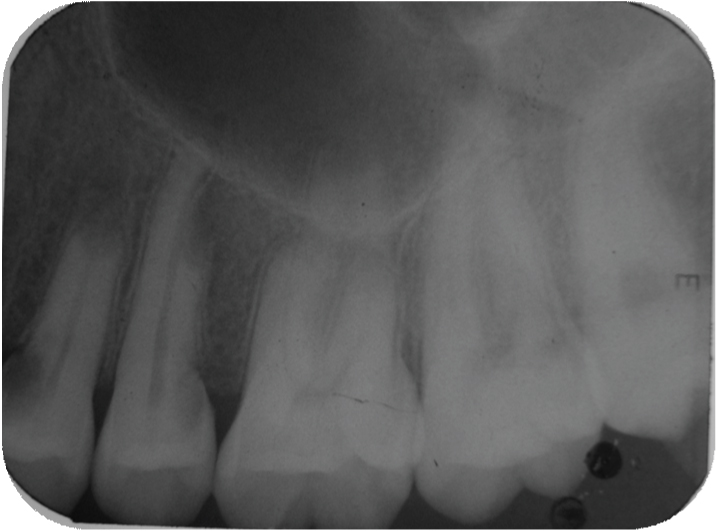
In [Table/Fig-8] intraoral periapical radiograph showing cervical resorption in relation to 33, 34, resorption in both cervical and apical region in relation to 35, 36. In [Table/Fig-9] intraoral periapical radiograph showing cervical and apical resorption in relation to 24, 25 and apical resorption in relation to 26. In [Table/Fig-10] intraoral periapical radiograph showing cervical and apical resorption in relation to 35, 36 and apical resorption in relation to 37. In [Table/Fig-11] intraoral periapical radiograph showing cervical and apical resorption in relation to 46, 47 and 48. In [Table/Fig-12] intraoral periapical radiograph showing cervical resorption in relation to 43, 44 and 45. [Table/Fig-13] Orthopantomograph. In [Table/Fig-14] lateral view of skull showing no osteogenic changes. In [Table/Fig-15] histological examination of extracted mobile teeth showing striae of Retzius, dentinal tubules and interglobular dentin with an area resembling dead tract. Correlating the history, clinical findings supported by radiographic appearance, diagnosis of Multiple Idiopathic external root resorption was made.
Intraoral periapical radiograph showing cervical resorption in relation to 33, 34, resorption in both cervical and apical region in relation to 35,36
Intraoral periapical radiograph showing cervical and apical resorption in relation to 24, 25 and apical resorption in relation to 26
Intraoral periapical radiograph showing cervical and apical resorption in relation to 35, 36 and apical resorption in relation to 37
Intraoral periapical radiograph showing cervical and apical resorption in relation to 46, 47 and 48
Intraoral periapical radiograph showing cervical resorption in relation to 43, 44 and 45
Lateral view of skull showing no osteogenic changes

Histological examination of extracted mobile teeth showing striae of Retzius, dentinal tubules and interglobular dentin with an area resembling dead tract

[Table/Fig-16] showing the resorption of the roots of the extracted teeth in relation to 12, 41 and 42. The teeth having mobility were extracted. The teeth 12, 41 and 42 were sent for histopathological examination (ground sectioning) which revealed: crown morphology comprising of enamel and dentin. The enamel shows striae of retzius, dentin showed dentinal tubules, interglobular dentin with an area resembling dead tract (longitudinal section). [Table/Fig-17] showing the ground section of the extracted tooth specimen. Followed by removable partial denture and teeth with resorped root was endodontically treated. Patient was advised to maintain proper oral hygiene and referred to the department of periodontology for further treatment of gingival enlargement and periodic follow up was suggested.
Showing the resorption of the roots of the extracted teeth in relation to 12, 41 and 42

Showing the ground section of the extracted tooth specimen
Discussion
Multiple idiopathic root resorption is a very uncommon condition which may manifest in the cervical or apical region [1]. It has been postulated that external root resorption has been attributed to 2 types of factors.
a) Local factors: Orthodontic therapy, trauma, periapical or periodontal inflammation, tumours, cysts, occlusal stress, impacted and supernumerary teeth, transplantation and reimplantation are among the local causes that could lead to pathological root resorption [2,3].
b) Systemic factors: Hyperparathyroidism, hypoparathyroidism, hypophosphatemia, hyperphosphatemia, Gaucher’s disease, Paget’s disease of the bone, Goltz syndrome, Papillon - Lefevre syndrome, anachoresis, Turner syndrome as well as dietary habits have been reported as related endocrine disturbances and systemic causes [4–6].
Four types of idiopathic external root resorption have been described in various literature:
Localized Idiopathic Cervical Resorption (LICR);
Multiple Idiopathic Cervical Resorption (MICR);
Localized Idiopathic Apical Resorption (LIAR);
Multiple Idiopathic Apical Resorption (MIAR) [7].
This case report describes a new type of tooth resorption (Suggested new terminology)
Multiple Idiopathic Cervico-Apical Resorption (MICAR).
Localised and multiple idiopathic cervical root resorption exhibit cavity like irregular radiolucency that is present near to the cemento-enamel junction (CEJ), which starts in the region of periodontal ligament (PDL) and extends to involve the root canal system of the effected tooth [8,9]. The local and multiple root resorption are brought about by Periapical Replacement Resorption (PARR) which is shortening of the apical portion of the root with normal bone exhibiting the normal trabeculae pattern in radiograph [10].
The common complaint of the patient with idiopathic root resorption is mobility of the involved tooth. Therefore this condition can be confirmed only by radiograph. Patient had class II malocclusion with increased overjet and overbite but compensatory thickening of cementum layer increased periodontal space could not be appreciated ruling out occlusal stress to be the aetilogical factor. ([Table/Fig-7] shows cervical resorption in relation to 15 and apical root resorption of mesial and distal roots in relation to 16, there is loss of PDL space in 17). All teeth had vital pulps and there was no periodontal or periapical inflammation. By definition, idiopathic external root resorption is a diagnosis of exclusion. Hence, in the absence of any plausible causative factor we considered this case as multiple idiopathic apical root resorption.
Conclusion
Multiple idiopathic apical root resorption involve a wide age range with unknown aetiology. Further investigations are needed to disclose its molecular mechanism and treatment. Henceforth a new type of idiopathic root resorption should be described: Multiple Idiopathic Cervico-Apical Resorption (MICAR).
[1]. Cholia SS, Wilson PH, MakdissiJ. Dentomaxillofac Radiol 2005 34(4):240-46. [Google Scholar]
[2]. Ne RF, Witherspoon DE, Gutmann JL, Tooth resorptionQuintessence Int 1999 30:9-25. [Google Scholar]
[3]. Aren Schätzle M, Tanner SD, Bosshardt DD, Progressive, generalized, apical idiopathic root resorption and hypercementosisJ Periodontol 2005 76(11):2002-11. [Google Scholar]
[4]. Newman WG, Possible etiologic factors in external root resorptionAm J Orthod 1975 67:522-39. [Google Scholar]
[5]. Belanger GK, Coke JM, Idiopathic external root resorption of the entire permanent dentition: report of a caseJ Dent Child 1985 52:359-63. [Google Scholar]
[6]. Rudiger S, Berglundh T, Root resorption and signs of repair in Papillon-Lefe`vre syndrome: a case studyActa Odontol Scand 1999 57:221-24. [Google Scholar]
[7]. Kanas RJ, Kanas SJ, Dental root resorption: A review of the literature and proposed new classification systemCompend Cont Educ Dent 2011 (32):3 [Google Scholar]
[8]. Regezi JA, Sciubba J, Jordan R, Abnormalities of the TeethIn: Oral Pathology: Clinical-Pathologic Correlations 2012 6th edSt. Louis, MOSaunders Elsevier:373-89. [Google Scholar]
[9]. Neville BW, Damm DD, Allen CM, Bouquot JE, Oral and Maxillofacial Pathology 2009 3rd edSt. Louis, MOSaunders Elsevier [Google Scholar]
[10]. Bakland LK, Root resorptionDent Clin North Am 1992 36:491-507. [Google Scholar]