Brain and Lung Abscesses in a 48-year-old Man with Focal and Segmental Glomerulosclerosis
Ali Momeni1, Fereidoon Rahmani2, Hamid Nasri3
1Nephrologist, Department of Nephrology, Shahrekord University of Medical Sciences, Shahrekord, Iran.
2Infectious Disease Specialist, Department of Infectious Diseases, Shahrekord University of Medical Sciences, Shahrekord, Iran.
3Researcher, Department of Nephrology, Isfahan University of Medical Sciences, Isfahan, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hamid Nasri, Researcher, Department of Nephrology, Division of Nephropathology, Isfahan University of Medical Sciences, Isfahan, Iran.
E-mail: hamidnasri@med.mui.ac.ir
Focal segmental sclerosis (FSGS) is a common cause of idiopathic nephrotic syndrome in the adult population. A patient aged 48- year-old was admitted for evaluation of azotemia. Renal biopsy showed tip lesion FSGS and acute tubular necrosis. After methyl prednisolone pulse therapy, partial remission occurred, and he was stable with oral prednisolone and cyclosporine. Few months later two serious complications including lung and brain abscess occurred. We describe a case of FSGS with lung and brain abscess, who responded to medical management.
Medical management, Nephrotic syndrome, Prednisolone, Serious infections
Case Report
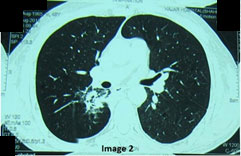
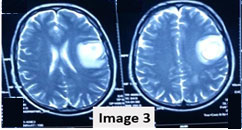
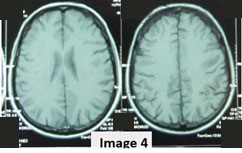
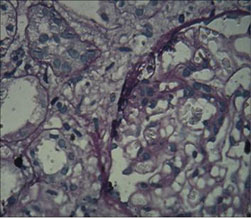
We report a case of FSGS (tip lesion) with nephrotic syndrome and acute renal failure that complicated with pulmonary and brain abscesses and was under immunosuppressive therapy. The patient was a 48-year-old man who was admitted for evaluation of azotemia. There was a history of decreased urine volume in recent days. He presented with BP=160/100 and 3+ leg edema on physical examination. He did not have any history of recent sore throat, hypertension (HTN), oral ulcer, arthralgia, photophobia, skin rash or family history of renal disease. Urinlysis showed 3+proteinuria and 2+hematuria. Serum creatinine was 2.3 mg/dl, blood urea nitrogen=32mg/dl, serum albumin=2.4g/dl, triglyceride=295mg/dl, cholesterol=320mg/dl, Hb=13g/dl and 24 h urine protein was 6580 mg/day. Other laboratory findings were unremarkable. He was oliguric and the serum creatinine gradually increased to 6.8 mg/dl during the next few days. Microscopic urine sediment showed many muddy brown coarse granular cast, dysmorphic RBC and fatty cast. Because of elevated serum creatinine and uncontrolled hypertension and volume overloading, hemodialysis was started and after blood-pressure control (by amlodipine 10mg/day, prazocine 5mg/bid, metoprolol 50mg/bid), renal biopsy was done. The results of serologic examination including ANA, anti-ds DNA, C3, C4, CH50, HBS Ag, HCV Ab, HIV Ab, Cryoglobulin, Anti GBM Ab and ASO were normal. Renal biopsy showed focal segmental glomerulosclerosis (tip lesion type) as well as acute tubular necrosis. Corticosteroid pulse (methyl prednisolone 1000 mg/day) was prescribed for three days and continued with 60 mg prednisolone/day. Conservative management of metabolic acidosis, hyperlipidemia, anemia and hypocalcemia was continued. after hemodialysis three times daily (HD), urine output increased and serum creatinine decreased gradually to 1.5 mg/dl and his oedema decreased to 1+ after two weeks of admission, so he was discharged and prednisolone was tapered gradually to 20 mg/day during 4 months. Because serum creatinine was increased, cyclosporine 100 mg/bid was started and after four weeks, serum creatinine reached to 0.8 mg/dl and urine protein was 740 mg/day. Six weeks later, he suffered from productive cough and shaking chill and fever. Chest x ray and chest CT scan revealed right side pulmonary abscess [Table/Fig-1]. BK (Bacille de Koch) smear of sputum was negative. Treatment with ceftriaxone 1g/bid/IV infusion and clindamycin 600mg/tds/IV infusion was prescribed and after four days, fever disappeared. After two weeks of parenteral treatment, he was discharged and oral antibiotics with Amoxicillin-clavulanate 625mg/TDS continued for four additional weeks, and the, second lung CT scan was near normal [Table/Fig-2]. Cyclosporine dose was reduced to 100 mg/day and serum creatinine remained 1.5 mg/dl. After three months he was again referred to clinic with dysarthria and right side face deviation and hence was admitted. A large round mass like lesion was detected in his right side brain CT scan and MRI [Table/Fig-3]. Differential diagnosis was: bacterial, nocardial or fungal brain abscess, brain lymphoma, and atypical brain tuberculosis. Tuberculin standard test (TST) was <5mm and bone marrow aspiration was normal. The patient was with fered to undergo astreotaxis biopsy of brain lesion but because of his reluctance, empirical treatment with parenteral penicillin 4 million unit /q4hr + metronidazole 750mg/tds + trimethoprim sulfametoxazole 800/4000 mg/q24hr, IV infusion, were started. After two weeks of treatment, severity of dysarthria and size of brain lesion decreased [Table/Fig-4,5]. This parenteral antibiotics regimen continued for eight weeks in hospital and due to high suspicious of brain Nocardiosis, oral trimethoprim sulfametoxazole, was continued for additional eight months. Also, treatment of FSGS was continued with prednisolone 20 mg/day, losartan 25mg/bid, furosemide 40mg/bid, prazocine 5mg/bid, atorvastatin 20mg/day, ASA 80 mg/day and diltiazem 30 mg/bid. After 10 months of treatment, he is well without any focal neurologic abnormality, and near normal brain MRI. His serum Cr is between 0.9 mg/dl and urine protein is 625 gm/day.
Discussion
FSGS is the second most common cause of nephrotic syndrome in adults, as in some countries prevalence of FSGS has been greater than membranous nephropathy especially at recent decades [1] . Two forms of FSGS were described, as primary or idiopathic FSGS which most often presents with the nephrotic range proteinuria and secondary FSGS, with non-nephrotic proteinuria and often some degree of renal insufficiency [2] . Histological types of FSGS consist of Classic FSGS, also called FSGS NOS that is the most common form, Collapsing, Tip, Perihilar and Cellular variant [3,4] . The patients with tip lesion type may are to present abruptly with the nephrotic syndrome and are more likely to respond to glucocorticoid therapy and some patients may undergo spontaneous remission without immunosuppressive treatment [5,6] .
Patients with long course treatment with corticosteroid are predisposed to opportunistic infections. For example tuberculosis as a primary infection or reactivation of old TB is the one of the most common and serious infection in these patients. Also, pulmonary Nocardiosis is an infrequent and severe infection as a subacute or chronic disease that can complicate them [7] . There are a few reports about complication of FSGS with lung or brain abscess, for example Han reported a case of nocardial brain abscess in a FSGS patient during treatment of high dose of corticosteroid [8] . Besides, four cases of noncardial brain abscess were reported by Tamarit, one case did not have any predisposing factors, second case was HIV positive antibody, third case was an old man with history of silicosis and last one was a patient with alcoholic hepatitis, sarcoidosis and longtime corticosteroid consumption. In all patients surgical drainage of brain abscess was done and one patient died despite of treatment [9] .
Right pulmonary abscess before treatment

Near complete resolution of lung abscess after treatment
Left hemisphere brain abscess before treatment
Resolution of abscess after treatment
Renal biopsy in accordance with FSGS
Conclusion
To the best of our knowledge, this is the first report of combination of brain and lung abscess in FSGS where the patient was treated by antibiotic without invasive approach and abscess drainage. The case signifies a higher risk of opportunistic and serious infection in the patients with nephrotic syndrome especially those on immunosuppressive agents.
Acknowledgement
We thank Research and Technology Deputy of Shahrekord University of Medical Sciences for all their help.
[1]. GL Braden, JG Mulhern, MH O’Shea, SV Nash, AA Ucci, MJ Germain, Changing incidence of glomerular diseases in adultsAm j kidney dis 2000 35(5):878-83. [Google Scholar]
[2]. A Meyrier, Nephrotic focal segmental glomerulosclerosis in 2004: an updateNephrol, dial, transplant 2004 19(10):2437-44. [Google Scholar]
[3]. V D’Agati, Pathologic classification of focal segmental glomerulosclerosisSeminars in Nephrology 2003 23(2):117-34. [Google Scholar]
[4]. E Ibrahim Seif, E Abdel-Salam Ibrahim, N Galal Elhefnawy, M Ibrahim Salman, Histological patterns of idiopathic steroid resistant nephrotic syndrome in Egyptian children: A single centre studyJ Nephropathol 2013 2(1):53-60. [Google Scholar]
[5]. MB Stokes, GS Markowitz, J Lin, AM Valeri, VD D’Agati, Glomerular tip lesion: a distinct entity within the minimal change disease/focal segmental glomerulosclerosis spectrumKidney int 2004 65(5):1690-702. [Google Scholar]
[6]. S Shakeel, M Mubarak, IK J, N Jafry, E Ahmed, Frequency and clinicopathological characteristics of variants of primary focal segmental glomerulosclerosis in adults presenting with nephrotic syndromeJ Nephropathol 2013 2(1):28-35. [Google Scholar]
[7]. AR Tunkel, Brain Abscess in: Mandell, Douglas,and Bennett’s Principles and Practice of Infectious Diseases: Churchill Livingstone 2010 [Google Scholar]
[8]. KY Han ST, SH Song, Y Uh, BG Han, SO Choi, JW Yang, A Case of Nocardia farcinica Brain Abscess in a Focal Segmental Glomerulosclerosis Patient after Steroid TreatmentKorean J Nephrol 2011 30(1):98-101. [Google Scholar]
[9]. M Tamarit, P Poveda, M Baron, JM Del Pozo, Four cases of nocardial brain abscessSurg Neurol Int 2012 3:88 [Google Scholar]