Case Report
A 50-year-old male patient reported to the Oral Medicine, Diagnosis and Radiology Department of the Goa Dental College & Hospital, Bambolim, Goa, India with a chief complaint of a swelling and growth in the left maxillary region since four months. There was no associated pain or discharge from the area. The patient gave a history of excision of the lesion intra-orally by a private practitioner two months back (the exact details of the surgical procedure carried out were not recorded and the excised specimen was not sent for histopathological analysis), but the lesion recurred 15 days later. There was no relevant social, medical or drug history.
On extra-oral examination, a diffuse swelling was seen over the left cheek region, extending antero-posteriorly from the left nasolabial fold to the malar region, and supero-inferiorly from the infra-orbital region to a point 2 cms above the left angle of mouth, measuring around 3 x 2 cms. The overlying skin was normal with no evidence of any discharge. On palpation, the swelling was firm in consistency, non-tender, non-pulsatile and non-compressible, with no local rise in temperature. The submandibular, submental and cervical lymph nodes were not palpable.
Intra-oral examination revealed a diffuse swelling in the maxillary left buccal vestibule extending from 24 to 27, causing obliteration of the buccal vestibule. The swelling was firm to hard and non-tender on palpation. A soft-tissue mass was also noted on the maxillary left buccal gingiva, in relation to the 24, 25, 26 region, extending mesio-distally from the mesial aspect of 24 along the buccal gingiva up to the mesial aspect of 26, involving the attached gingiva superiorly, and overlying the middle one-third of the crowns of the involved teeth inferiorly, measuring approximately 2 x 1.5 cms [Table/Fig-1]. The mass was roughly oval in shape, reddish-pink in color and firm in consistency with a surface showing areas of ulceration and bleeding on palpation. There was no evidence of any swelling on the palate. No tenderness or mobility of the teeth in the involved area was noted. Based on the history given by the patient and the clinical features, a provisional clinical diagnosis of a maxillary sinus malignancy was made, with a differential diagnosis of a malignant tumour, hamartoma and metastatic malignancy.
Intra-oral view showing a soft-tissue mass in the maxillary left buccal gingiva and vestibule

An intra-oral periapical radiograph showed a mixed radiolucent-radiopaque lesion with an ill-defined periphery in relation to 24, 25, 26 and 27. Root resorption of 24, 25, 26 with irregular margins was noted upto the middle one-third [Table/Fig-2]. A maxillary cross-sectional occlusal did not show any cortical expansion or bony growth in the affected area. Panoramic radiography showed a large irregular mixed lesion in the left maxilla in relation to 24, 25, 26 and 27, extending inferiorly to the cervical one-third of the roots and superiorly involving the maxillary sinus. The lesion had an ill-defined non-corticated border and the internal structure showed a mixed radiolucent-radiopaque density with irregular amorphous areas of calcification. Root resorption of 24, 25, 26 upto the middle one-third was evident. A paranasal sinus view showed cloudiness in the lower half of the left maxillary sinus.
Intra-oral periapical view showing a mixed radiolucent-radiopaque lesion with ill-defined borders in relation to 24, 25, 26 and 27 causing root resorption of the involved teeth

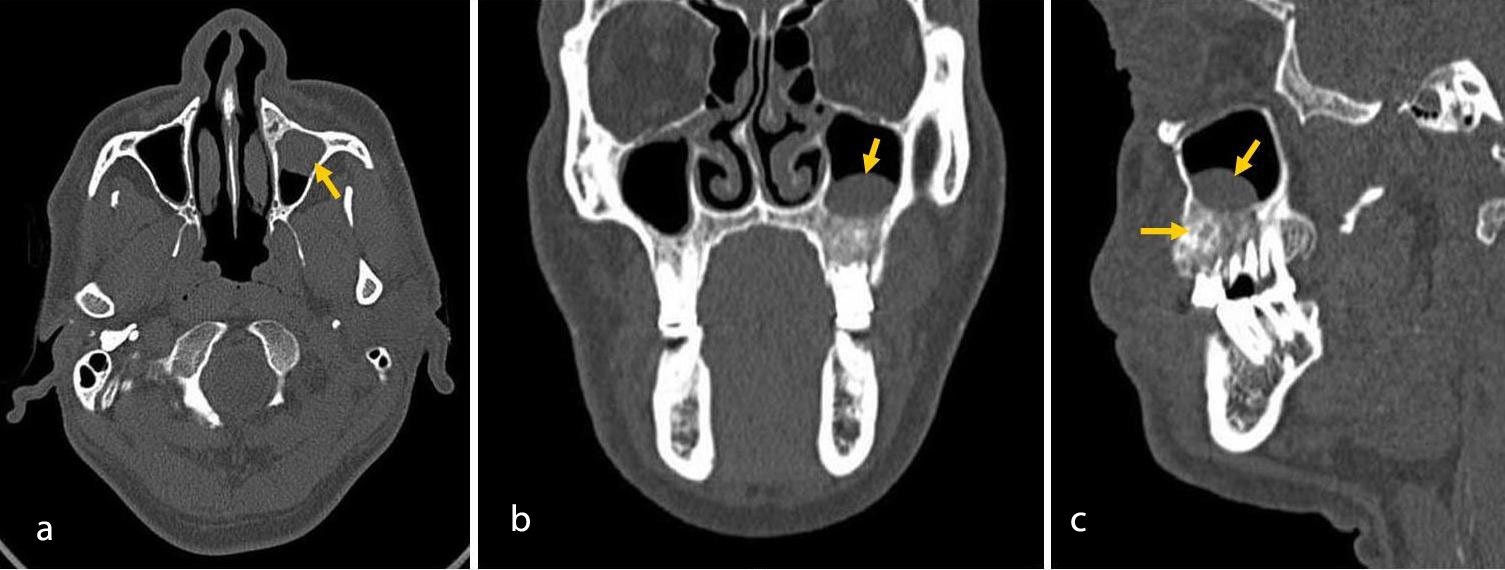
A computerized tomography scan revealed an expansile lesion involving the left maxilla in the premolar and molar region with a dome-shaped extension of the lesion through the floor of the maxillary sinus to involve the lower half of the left sinus. Destruction of the floor of the maxillary sinus was also noted [Table/Fig-3]. The radiographic differential diagnosis included a malignant tumour, central ossifying fibroma, calcifying epithelial odontogenic tumour and cementoblastoma.
CT scan of maxilla (a) Axial Section, (b) Coronal Section, (c) Sagittal Section – showing an expansile lesion involving the left maxilla with a dome-shaped extension into the lower half of the left maxillary sinus, causing destruction of the sinus floor
Blood investigations carried out were all within normal range. An incisional biopsy of the lesion was carried out which showed a fibromyxoid connective tissue stroma containing plump stellate cells with long cytoplasmic processes anastomosing with each other and few pleomorphic spindle cells. The cells showed hyperchromatism, pleomorphic and some vesicular nuclei. The findings of the incisional biopsy were suggestive of a malignant mesenchymal tumour.
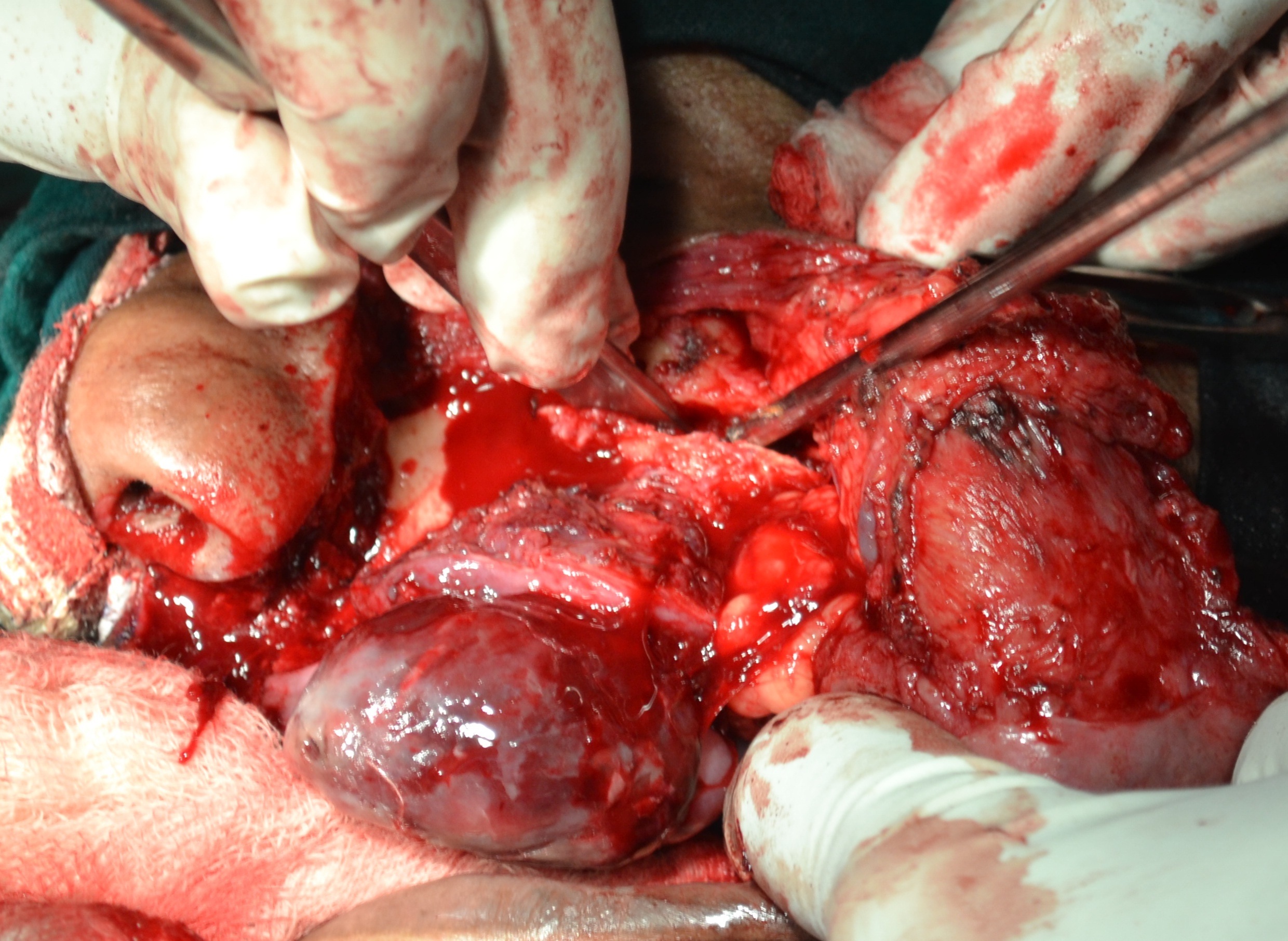
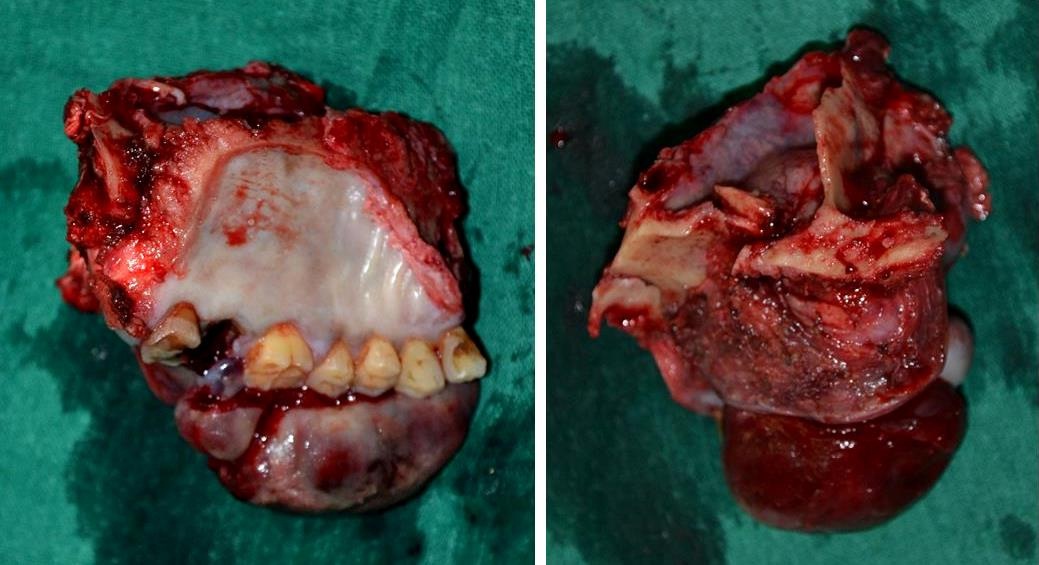
A week after the incisional biopsy, the patient reported to our department with a significant increase in the size of the intra-oral growth. The mass had increased to 8 x 5 cms in diameter (around four times its initial size) and had begun to interfere with mastication and speech [Table/Fig-4]. Computed tomography, a chest radiograph and ultrasound examination was advised to rule out local metastases. These investigations however, did not reveal any evidence of metastases. Based on the clinico-radiographic features and findings of the incisional biopsy, a subtotal maxillectomy was performed under general anesthesia. This procedure was performed using the Weber-Ferguson approach, in which an incision line was drawn through the vermilion border, along the philtrum of the lip, around the base of the nose and along the facial nasal groove, extending infraorbitally 3-4 mm below the ciliary line to the lateral canthus of the eye. The incision was carried down through the periosteum to facilitate elevation of the cheek flap laterally in a subperiosteal plane over the maxilla. Osteotomy cuts were then carried out and resection of the left hemi-maxilla was performed [Table/Fig-5,6a,b]. After completion of the resection, a medicated gauze pack was placed in the cavity and was covered by a palatal obturator to close the oro-nasal communication [Table/Fig-7,8].
Intra-oral view showing significant increase in size of the lesion following incisional biopsy

Intra-operative view showing resection of left hemi-maxilla
Resected left hemi-maxilla
Postoperative intra-oral view
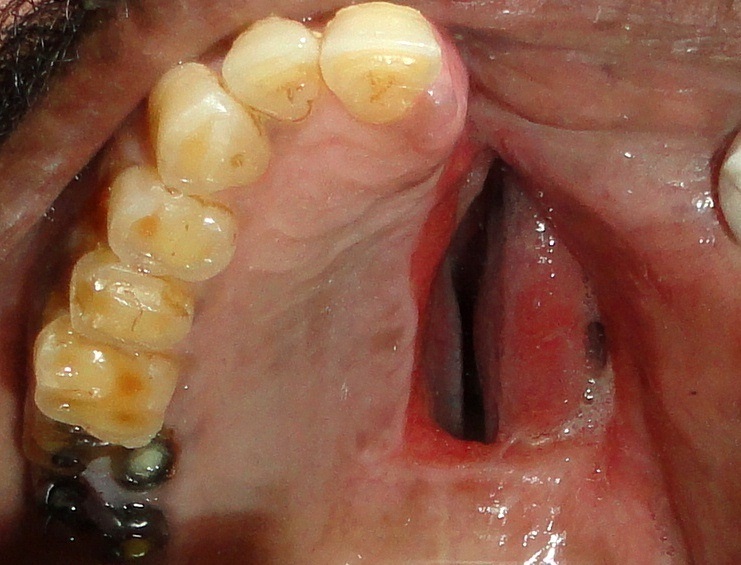
Postoperative intra-oral view following placement of palatal prosthesis

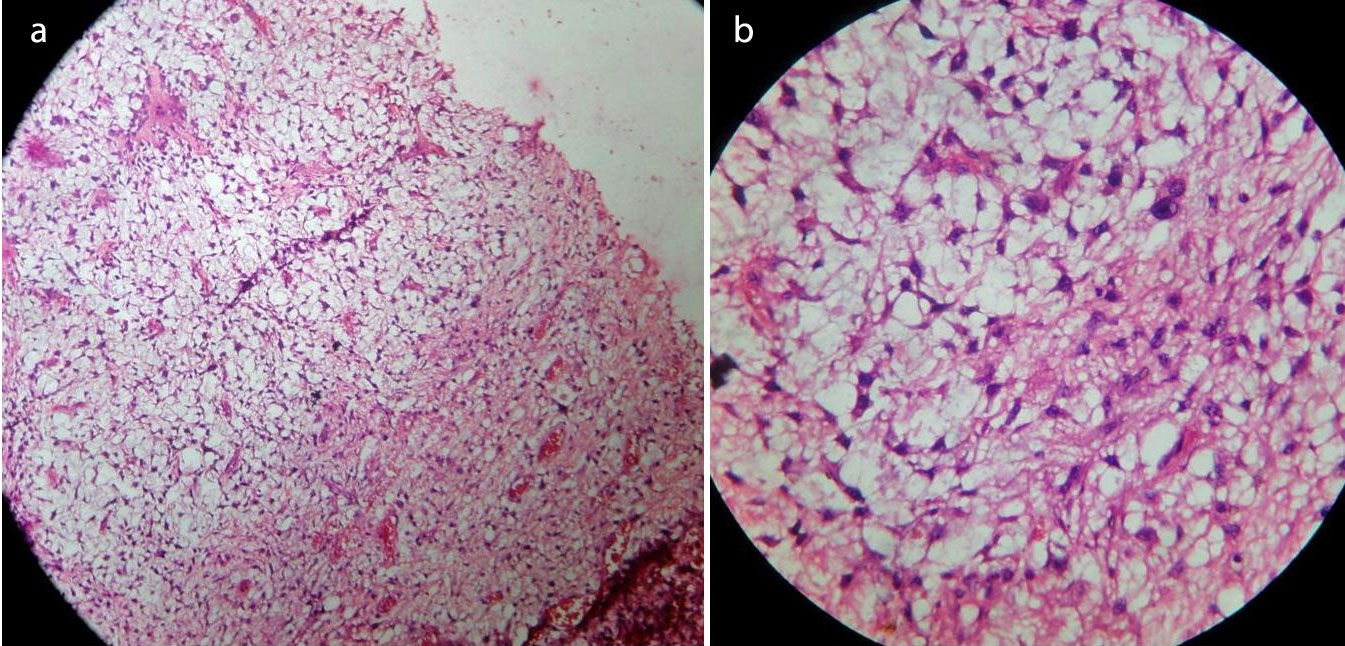
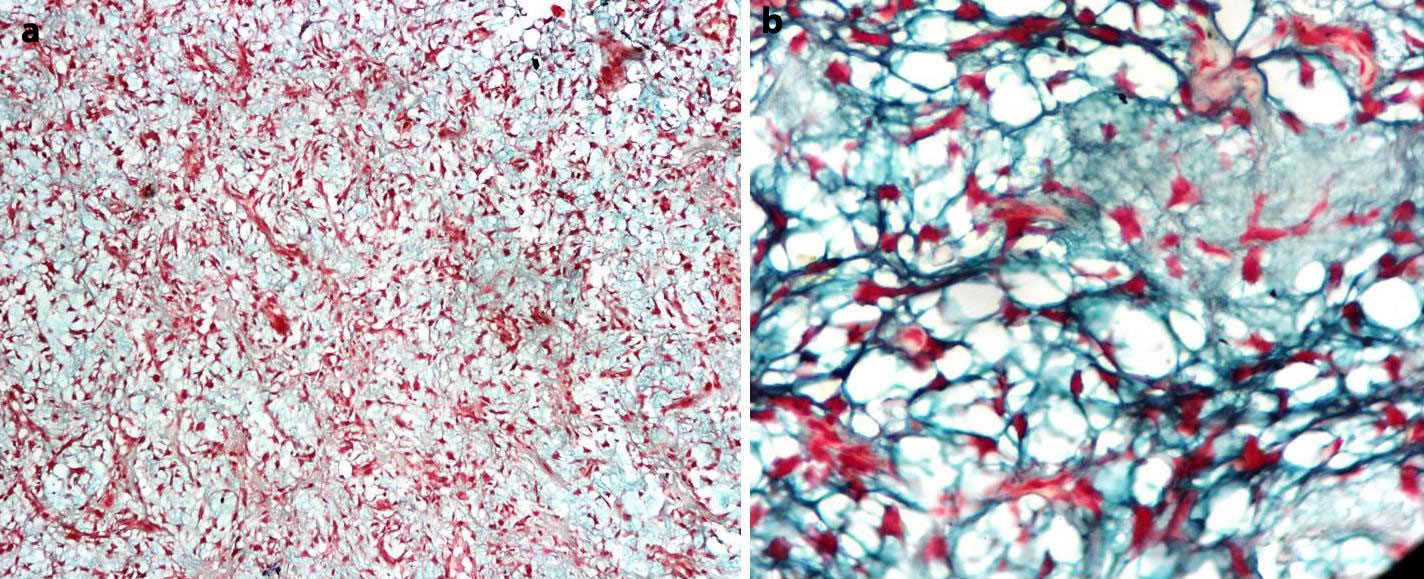
Histopathological examination of the resected specimen showed the presence of spindle and stellate cells proliferating in an abundant myxoid stroma, with focal reactive bone trabeculae. Nuclear hyperchromasia, pleomorphism and atypical mitosis were evident [Table/Fig-9]. Staining with Alcian blue showed a positive uptake of the dye by the myxomatous tissue [Table/Fig-10]. Immunohistochemistry markers were positive for vimentin, smooth muscle actin and Ki-67 under 65%, while CD-34, S-100, desmin and myogenin were negative. Thus, based on the histopathological findings of the resected specimen, a final diagnosis of a myxosarcoma was made.
(a) Photomicrograph showing spindle-shaped and stellate cells in an abundant myxoid stroma with reactive bone trabeculae (H&E stain at 10x magnification). (b) Higher magnification showing nuclear hyperchromasia and pleomorphism in the cells (H&E stain at 40x magnification)
Photomicrograph of Alcian blue stained section showing positivity of myxomatous stroma (a) 10x magnification, (b) 40x magnification
Postoperative healing was uneventful. The patient has been under regular follow-up for the last three years, during which time no recurrence has been noted [Table/Fig-11].
Postoperative panoramic radiograph

Discussion
Sarcomas are malignant tumours of mesenchymal origin and may arise from bone, cartilage, muscle, neural or vascular tissue [1,2]. Myxomatous tissue is a derivative of connective tissue and can probably originate from the metaplasia of different types of connective tissue. Myxomatous tumours histologically resemble primitive mesenchymal tissue consisting chiefly of stellate cells set in a loose matrix of reticulum and collagen fibres; and separated by a mucoid material which consists mainly of polysaccharides [3]. The stellate shape of the cells helps to differentiate true myxoid lesions from other tumour varieties that show myxoid areas [4].
Sarcomas of the head and neck, especially myxosarcomas, are rare in literature and very few cases have been reported in the past. The myxosarcoma is regarded by many authors as a variant of fibrosarcoma, with abundant interstitial proteoglycans (connective tissue mucins) and is a very rare tumour [5]. Other authors however regard it as a malignant version of the odontogenic myxoma [6]. The exact origin of these lesions remains unknown. Among the various theories postulated, the two most commonly entertained are: (a) derivation from embryonal rests of mucous tissue, and (b) metaplasia of existing connective tissue [3].
Myxosarcomas are most likely to be diagnosed in individuals between the ages of 40 and 60 years, and show no special predilection for either sex [3]. They may occur in many tissues of the body, like the heart, bones, genitourinary system and skin. Jaw involvement is relatively uncommon. Clinically, lesions may present as an innocuous hemorrhagic mass similar in appearance to an ulcerated pyogenic granuloma or may occur as a rapidly enlarging or infiltrative growth that tends to recur repeatedly after inadequate local excision [7]. The growth rate is thought to vary, and local aggressiveness rather than metastasis is a prominent feature of this lesion [8]. Our patient presented with a diffuse swelling in the buccal vestibule and a roughly oval-shaped growth involving the buccal gingiva which showed surface ulceration and bleeding. The lesion also recurred after being excised (by a private practitioner) and showed a rapid increase in size. The age of the patient and clinical appearance of the present case was thus similar to that described in literature.
Myxosarcomas do not have any specific radiographic features that can differentiate them from other sarcomas. Radiographically, lesions are generally irregular in shape and usually show ill-defined borders with lack of cortication. While most lesions show a typically radiolucent internal structure, occasional lesions may stimulate the formation of reactive bone. Bone destruction due to osteolytic activity may be seen, and lesions may erode through bone to invade the adjacent soft tissue [4]. Destruction of adjacent structures is also a common feature [8]. Our case presented as an ill-defined lesion with a mixed radiolucent-radiopaque internal structure with irregular areas of calcification, which extended superiorly to involve the maxillary sinus, with destruction of the sinus floor. Irregular areas of bone and root resorption were also noted which were suggestive of a rapidly growing malignant tumour. There was absence of any periosteal reaction and no bony growth was evident on the occlusal radiograph. While the present case had ill-defined non-corticated borders, the internal structure contained irregular radiopaque calcified areas, which is in contrast to most previously reported cases, which predominantly showed radiolucent areas of bone destruction.
The histological picture presented by this tumour shows many variations. Loosely arranged stellate or spindle-shaped cells of various sizes are found in a majority of these neoplasms, though some tumours show only round cells in the cellular areas [3]. These cells show nuclear pleomorphism and atypical, bizarre mitotic figures, which are seen in appreciable numbers and are numerous in some tumours [9]. Our case also showed similar features as described above, with proliferation of spindle and stellate cells in an abundant myxoid stroma, and presence of nuclear hyperchromasia, pleomorphism and atypical mitosis. The presence of a predominantly myxoid stroma and absence of a herring-bone pattern on histopathological evaluation helped in ruling out a fibrosarcoma.
Sarcomas have an abundant blood supply, and therefore disseminate almost exclusively through the blood stream. Soft-tissue sarcomas have a smaller metastatic potential compared to bone sarcomas [10]. However, the metastatic potential of soft tissue sarcomas like myxosarcoma occurring within bone remains controversial since very few case reports have been described in literature. The treatment of choice for myxosarcomas is surgical resection with a wide margin. The need for adjuvant radiotherapy and/or chemotherapy is still unclear. Prophylactic neck dissection is also controversial. These lesions are thought to be locally malignant but regional and distant metastasis is rare; hence neck dissection is usually not indicated in the absence of palpable adenopathy [6]. The present case was treated with surgical resection (subtotal maxillectomy) followed by placement of a palatal obturator.
Conclusion
Myxosarcomas are considered to be a type of soft tissue sarcoma; however, in rare cases they may originate as an intra-osseous lesion. This was observed in the present case, which also showed atypical clinical and radiographic features. Histopathological evaluation, along with an immunohistochemical analysis thus plays an important role in providing a definitive diagnosis in such cases.
[1]. Dalirsani Z, Mohtasham N, Falaki F, Bidram F, Nosratzehi T, Malignant Fibrous Histiocytoma of Mandible: A Review of Literatures and Report a CaseAust J Basic Appl Sci 2011 5(5):936-42. [Google Scholar]
[2]. Pandey M, Thomas G, Sarcoma of the oral and maxillofacial soft tissue in adultsEur J Surg Oncol 2000 26(2):145-48. [Google Scholar]
[3]. Thibaudeau AA, Kress LC, Myxosarcomata: With a Report on 51 Cases Studied at the State Institute for the Study of Malignant Disease, Buffalo, New YorkAm J Cancer 1935 23:267-81. [Google Scholar]
[4]. Wolfowitz BL, Schmaman A, Unusual Malignant Tumours of the Maxillary SinusesS Afr Med J 1975 49:387-91. [Google Scholar]
[5]. Lam KH, Wong J, Lim ST, Ong GB, Primary sarcomas of the jawAust N Z J Surg 1979 49(6):668-75. [Google Scholar]
[6]. Lamberg MA, Calonius BP, Makinen JE, Paavolainen MP, Syrjanen KJ, A case of malignant myxoma (myxosarcoma) of the maxillaScand J Dent Res 1984 92(4):352-57. [Google Scholar]
[7]. Knerler C, Rowe L, Myxosarcoma of the SkinAMA Arch Derm 1955 72(2):173-75. [Google Scholar]
[8]. Foo GC, Zain RB, Well-Differentiated Fibrosarcoma of the Maxilla - A Case ReportSingapore Med J 1984 25(4):274-77. [Google Scholar]
[9]. DeFatta RJ, Verret DJ, Ducic Y, Carrick K, Giant Myxomas of the Maxillofacial Skeleton and Skull BaseOtolaryngol Head Neck Surg 2006 134(6):931-35. [Google Scholar]
[10]. Shmookler B, Bickels J, Jelinek J, Sugarbaker PH, Malawer MM, Bone and Soft-tissue Sarcomas: Epidemiology, Radiology, Pathology and Fundamentals of Surgical Treatment. In: Malawer MM, Sugarbaker PH, editorsMusculoskeletal Cancer Surgery: Treatment of Sarcomas and Allied Diseases 2001 New YorkSpringer:3-35. [Google Scholar]